Introduction
Mandibular lip-bumper (LB) nonextraction treatment, usually started before complete second molar (M2) eruption, inevitably interacts with the development of the dentition. Yet, its effects on M2 eruption are still unknown. The first aim of this study was to retrospectively investigate whether LB therapy (260 patients) enhances the risk for M2 ectopic eruptions and impactions in comparison with 135 untreated subjects. The second aim was to assess, among treated patients (n = 197), the main potential determinants of M2 impaction and ectopic eruption.
Methods
M2 eruption and impaction were determined on panoramic radiographs. To assess the predictive role of M2 inclination in relation to the first molar, a panoramic radiograph suitable for this measurement before treatment was required. The data were analyzed by using software (version 8.2, SAS, Cary, NC).
Results
LB treatment significantly enhanced M2 impaction and ectopic eruption. Negative prognostic factors were found. An initial inclination of the M2 greater than 30° was significantly associated with a higher impaction risk compared with an angulation less than10°. LB treatment duration longer than 2 years increased the risk of ectopic eruptions.
Conclusions
While gaining space in the anterior arch, unwanted effects might be produced in the posterior arch. To be informed about these unplanned events is necessary to better optimize treatment.
Mandibular second molar (M2) eruption is a complex event, requiring the uprighting of its mesially inclined path, further guided by the distal root of the first molar (M1) and resorption of the mandibular anterior ramus. Failure of the M2 to correctly erupt can lead to disturbances from ectopic eruption to impaction. The latter event is increasing in normal populations, and its multifactorial etiology is not completely clear. Among the registered risk factors, a marked M2 to M1 angulation (>20°) was indicated. This physical relationship between M1 and M2 is delicate and requires adequate spacing in the bone. Hence, both space deficit and surplus appear to be possible factors disturbing the correct eruption of M2. Because the management of arch spacing belongs to the orthodontic specialty, its treatments have already been cited among the hypothetic causes or concauses for eruption delays, disturbances, and impactions. The therapies discussed here are nonextraction treatments started early, before complete eruption of M2. Indications for early intervention are usually dental crowding and biprotrusion correction. In addressing this issue, the most used device is the mandibular lip bumper (LB), widely recognized for successfully expanding dental arches in the transversal, sagittal, and vertical planes. More specifically, LBs produce posterior sagittal expansion of the arch, through distal tipping of the M1, which becomes more effective when adding buccal shields. If M1 distal tipping creates mesial space, thus helping crowding resolution, it also reduces distal space, presumably disturbing the adjustment processes of M1, M2, and bone spacing, necessary for a physiologic eruption of M2.
The implications and effects of LB use on M2 eruption are yet to be investigated.
The primary aim of this retrospective investigation was to verify whether LB treatment enhances the risk of M2 impaction or ectopic eruption in comparison with untreated subjects.
The secondary aim was to assess, among treated patients, the main determinants in the development of impaction or ectopic eruption problems.
Material and methods
From 890 patients who consecutively visited an experienced orthodontist from 1982 to 2004, those with anterior mandibular crowding of 2 mm or more were collected for this study (n = 683). Exclusion criteria were M2 eruption and all possible factors predisposing or impeding M2 impaction, such as agenesis, dental inclusions, destroying caries, and previous dental extractions. Patients with inadequate documentation or without a panoramic radiograph for M2 eruption or impaction diagnosis were excluded ( Fig ).
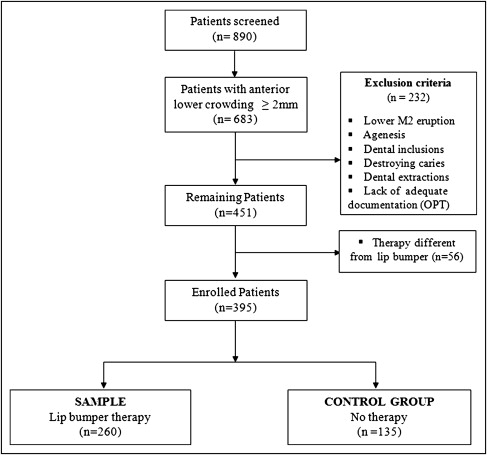
Of the 451 remaining subjects, 56 had treatments other than gingival LBs and were excluded from the investigation. The 260 patients treated with the LB and the 135 who received no therapy were included in the study.
Because of the variety of LB designs, the appliance was limited to 1 design: the gingival level in the vertical plane, under the action of the perioral muscles.
Patients could remove the LB by themselves but were asked to wear it 24 hours a day, taking it out only for meals. LB treatment duration was individually dictated by crowding severity and cooperation.
Panoramic radiographs were used for the determination of M2 eruption or impaction. An M2 was considered erupted once it reached the functional occlusal plane with its mesial marginal ridge at the same level of the M1’s distal marginal ridge.
Impaction was diagnosed for molars whose eruption was interrupted before gingival emergence by physical barrier or abnormal dental position. Even if three quarters of root development already indicated a good maturational stage for eruption, closed apices were necessary for impaction diagnosis for an easier standardized method. Patient age was calculated at the radiographic diagnosis.
To assess the predicting variables, we used a pretreatment panoramic radiograph when the inclination measurements of M2 to M1 were possible before the beginning of treatment and M2 eruption.
Hence, of the 260 treated patients, 197 with a panoramic radiograph suitable for M2 to M1 inclination measurement were further selected. On these tracings, a line was drawn through the midpoints of the occlusal surfaces and root bifurcations of both M1 and M2; the superior anterior angle resulting from the intersection of M1 and M2’s longitudinal axes indicated the degree of M2 inclination. Age at the beginning of LB treatment was also calculated.
All patients gave their consent for data publications.
Statistical analysis
The data were analyzed by using SAS software (version 8.2, SAS, Cary, NC). Continuous variables were expressed as means and standard deviations and compared with unpaired Student t tests. Category variables were expressed as absolute numbers and percentages and compared by using the chi-square test. The 2 groups (treated and control) were compared with multivariate logistic regression analysis, since a variety of factors might have acted together and influenced the M2 impaction and ectopic eruption. Results were presented as odds ratios (OR) with corresponding 95% confidence interval (CI). For this analysis, the data were summarized at the patient level, defining for each outcome (M2 impaction or ectopic eruption) a variable that was given the value 1 if at least 1 tooth (left or right) reached the outcome, and the value 0 if neither of the 2 teeth reached the outcome. The covariates were included in the models a priori by identifying the potential confounders in the comparison between the 2 groups. Possible differences in patient follow-ups between the 2 groups were taken into account, including age at radiographic diagnosis in the model.
For the second aim, generalized estimating equation logistic regression models were used to identify the main potential determinants of M2 impaction and ectopic eruption in the treated group, but using data at the dental level. A generalized estimating equation regression model was used to account for patient-level clustering. Statistical significance was assessed for P <0.05.
Results
The selected treated and untreated groups were similar concerning sex, type of malocclusion, and diagnosis age. Mean anterior mandibular crowding was more severe in the control group (4.8 mm; SD, 2.1) than in the treatment group (3.8 mm; SD, 1.3) ( Table I ).
| Treated (n = 260) |
Control (n = 135) |
P value | |
|---|---|---|---|
| Clinical and demographic characteristics | |||
| Male, n (%) | 92 (35.4) | 58 (43.0) | 0.141 |
| Crowding in mm, mean (SD) | 3.8 (1.3) | 4.8 (2.1) | <0.001 |
| Crowding >4 mm, n (%) | 84 (32.3) | 62 (45.9) | 0.008 |
| Angle class of malocclusion, n (%) | 0.187 | ||
| I | 50 (19.2) | 34 (25.2) | |
| II | 194 (74.6) | 89 (65.9) | |
| III | 16 (6.2) | 12 (8.9) | |
| Impaction and eruption | |||
| Age at radiographic diagnosis in years, mean (SD) | 13.4 (1.5) | 13.8 (2.1) | 0.071 |
| Impaction, n (%) | 0.065 ∗ | ||
| Bilateral | 9 (3.5) | 1 (0.7) | |
| Unilateral | 9 (3.5) | 1 (0.7) | |
| None | 242 (93.1) | 133 (98.5) | |
| Ectopic eruption, n (%) † | <0.001 ‡ | ||
| Bilateral | 15 (6.0) | 1 (0.8) | |
| Unilateral | 26 (10.4) | 1 (0.8) | |
| None | 210 (83.7) | 132 (98.5) | |
| Characteristics of 197 treated patients and additional information | |||
| Male, n (%) | 73 (37.1) | ||
| Crowding in mm, mean (SD) | 3.8 (1.4) | ||
| Age at start of treatment in years, mean (SD) | 10.2 (1.1) | ||
| Treatment duration >2 years, n (%) | 99 (50.3) | ||
| Age at radiographic diagnosis in years, mean (SD) | 13.4 (1.5) | ||
| M2 inclination (394 molars) | |||
| <10°, n (%) | 188 (47.7) | ||
| 10°-20°, n (%) | 129 (32.7) | ||
| 21°-30°, n (%) | 52 (13.2) | ||
| >30°, n (%) | 25 (6.4) | ||
LB treatment started at a mean age of 10 years and lasted 28 months on average (range, 7-75 months). At each visit, the LB was kept gingival in the vertical plane, and a distance of 1 to 2 mm from the incisor was kept in the sagittal plane. Activations reflected the patient’s tolerance and perception of esthetics.
During follow-up, of the 395 analyzed patients, 20 exhibited M2 impaction. More specifically, M2 impaction was associated with LB treatment (18 patients; 9 bilaterally) in comparison with the control group (2 patients, 1 bilaterally; Table I ).
According to the multivariate analysis, the risk for M2 impaction in the treated patients was 9.0 times (95% CI, 1.8-45.2) higher than in the control group adjusted for sex, age at radiographic diagnosis, crowding, and Angle class malocclusion. Also, age at radiographic diagnosis and initial anterior crowding were significantly associated with M2 impaction in the multivariate analysis ( Table II ).
| Impaction (yes/no = 20/375) |
Ectopic eruption (yes/no = 43/342) |
|||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Treatment, yes vs no | 9.0 (1.8-45.2) | 0.007 | 18.5 (4.1–82.4) | <0.001 |
| Sex, male vs female | 0.8 (0.3–2.1) | 0.653 | 1.9 (0.9–3.6) | 0.073 |
| Age at radiographic diagnosis in years | 1.3 (1.0–1.7) | 0.048 | 1.3 (1.0–1.6) | 0.020 |
| Crowding in mm | 1.3 (1.0–1.8) | 0.047 | 1.1 (0.9–1.4) | 0.329 |
| Angle class of malocclusion | ||||
| I (reference) | 1.0 | 1.0 | ||
| II | 1.0 (0.3–3.1) | 0.432 | 1.6 (0.6–4.2) | 0.589 |
| III | 1.9 (0.3-11.4) | 0.519 | 1.9 (0.4–8.8) | 0.702 |
In the pooled sample, with the exclusion of bilateral impactions (385 subjects), ectopic eruptions occurred in 43 subjects, without a preference side, but with a more frequent distal inclination. Most significantly, ectopic eruption prevalence was increased by treatment: 41 patients (16.4%) vs 2 untreated subjects (1.6%) ( Table I ). In the multivariate analysis, the OR of treatment was 18.5 (95% CI, 4.1-82.4) compared with the control group. Furthermore, the increased incidence of ectopic eruption was correlated with age at radiographic diagnosis ( Table II ).
Inherently to the second aim, the study was conducted on 394 molars of 197 treated patients, for whom 22 impactions and 42 ectopic eruptions were found ( Table III ). M2 initial inclination greater than 30° was significantly associated with a higher impaction risk compared with an angulation less than 10°.



