Mandibular osteotomy is the most commonly used surgical procedure for correction of dentofacial deformities, particularly mandibular deficiency. Although there are numerous technical variations, sagittal split osteotomy is the technique most familiar and widely used by oral and maxillofacial surgeons. The purpose of this chapter is to provide a practical guide for surgeons in treatment planning and performing the bilateral sagittal split osteotomy (BSSO) for mandibular advancement.
Anatomic Consideration
The mandible is surrounded by a rich network of vascular and neural structures. Potential hemorrhage, although rare, may occur when the soft tissue is not properly retracted and the vessels located within the periosteal envelope are violated, such as maxillary, facial, and retromandibular vessels and their tributaries. Aside from the vascular structure surrounding the mandible, there is essentially one major anatomic structure of which surgeons must be aware in performing BSSO—the inferior alveolar (IA) nerve. Avoiding damage to the IA nerve is a major surgical goal, although postoperative neurosensory disturbance is an expected sequela of this technique and its avoidance is nearly impossible. Consistency in well-defined criteria for neurosensory deficit in the literature is sketchy at best. However, it would be misleading to say that the patients’ neurosensory recovery following BSSO would return to 100% of the baseline before surgery, because there are many instances where this is not the case. The clinical implications of neurosensory disturbances following BSSO will be discussed further in the latter part of this chapter, but the anatomic relationship of the IA canal to the buccal cortex of the mandible has been shown to be a factor in the development of neurosensory disturbance after BSSO. The IA canal that comes in contact with the buccal cortical bone has a significantly greater incidence of neurosensory disturbance than the IA canal that does not contact the buccal cortex, and it is also significantly more likely that altered sensation will be present 1 year after surgery. Contrary to the conventional wisdom, manipulation of the IA nerve does not consistently result in nerve dysfunction based on sensory-evoked potential, but the nerve conduction is clearly disturbed in cases with nerve laceration. Short mandibular height and the location of the mandibular canal near the inferior border of the mandible may increase the risk of IA nerve injury.
Diagnostic Studies
Lateral cephalometric and panoramic radiographs are routine diagnostic imaging necessary for surgical planning. Cone beam computed tomography (CT) is gaining popularity in orthognathic surgery, and although it can be a valuable adjunct to plain films in diagnosing jaw asymmetry and condylar abnormalities, routine use can be inhibitive in terms of cost to the patient.
Condylar morphology, position of the IA nerve, presence of impacted third molars, differential silhouettes of the inferior border of the mandible suggesting skeletal asymmetry, and steepness of the mandibular plane angle are some of the crucial checkpoints that must be evaluated on the plain films or CT images if they are available.
Diagnostic Studies
Lateral cephalometric and panoramic radiographs are routine diagnostic imaging necessary for surgical planning. Cone beam computed tomography (CT) is gaining popularity in orthognathic surgery, and although it can be a valuable adjunct to plain films in diagnosing jaw asymmetry and condylar abnormalities, routine use can be inhibitive in terms of cost to the patient.
Condylar morphology, position of the IA nerve, presence of impacted third molars, differential silhouettes of the inferior border of the mandible suggesting skeletal asymmetry, and steepness of the mandibular plane angle are some of the crucial checkpoints that must be evaluated on the plain films or CT images if they are available.
Model Surgery Checklist
In setting up the models for mandibular advancement, one has to check for the following:
- 1
Presence of nonfunctional maxillary second molar following mandibular advancement.
- 2
Incisor and canine relationship after simulated mandibular advancement.
- 3
Presence of the curve of Spee. If the curve of Spee is to be leveled postoperatively, then 0.5 to 1 mm extra overjet should be built into the final set-up, because the lower incisors will move forward during postoperative leveling of the curve of Spee.
- 4
Extent of the curve of Wilson (if there is a residual dental compensation evidenced by buccal tipping of the maxillary molars and lingual tipping of the mandibular molars) (see the section Adjunctive Technique: Midline Osteotomy ).
- 5
Presence of residual bicuspid extraction spaces. Sometimes, the orthodontist was not able to fully close the extraction spaces prior to surgery; one must then consider use of a temporary anchorage device for protraction of posterior segment for extraction space closure, or for overcorrection to an end-to-end incisor relationship to account for postoperative retraction of the lower incisors to close the extraction space.
Surgical Technique
The incision is made over the anterior portion of the vertical ramus, extending to the mesial aspect of the first molar. Subperiosteal dissection is carried down to the inferior border of the mandible, and a lateral channel retractor is placed. The exposure should be limited posteriorly to preserve the blood supply to the proximal segment. A forked retractor is used to strip the temporalis attachment superiorly, at least to the level of the sigmoid notch to ensure adequate access for the medial cut. Posteromedially, the periosteum must be reflected to the medial flare of the condylar neck. Inferiorly, the medial cortex is exposed to immediately above the lingula, and a medial channel retractor is placed.
A long bur is used to make a horizontal bone cut through the medial cortex of the ramus, just above the lingula. The medial cut should be approximately halfway into the ramus, and the surgeon must be able to look straight down to the cup of the medial channel retractor. The vertical cut is made through the buccal cortex, distal to the second molar or further anteriorly if a greater advancement is necessary. The cut must be made perpendicular to the inferior border and just through the lateral cortex, because the IA nerve is typically located just medial to the lateral cortex. The vertical and horizontal cuts are connected in the sagittal plane using a short-taper fissure bur or saw blade, just into the cancellous bone. In younger patients with a tendency for slower split, the sagittal bone cut is made a little deeper to facilitate the split propagating through the marrow space. If a third molar is present and is completely impacted, then the cut should be made through the entire mesiodistal width of the crown so that the crown will split into two halves as the mandibular split progresses.
Next, a curved osteotome is used to make sure that the medial cortical split is completed. A fine straight osteotome is tapped into the sagittal cut. A spreader and a narrow osteotome are used to gently lift the lateral cortex, and the osteotome is used to step along the connecting cut to ensure that the split stays close to the lateral cortex. Caution must be taken to visualize the IA nerve as soon as possible, because it is easy to lose sight of the nerve as the lateral cortex is split off from the medial cortex. Once the split is complete, the periosteal attachment of the medial pterygoid is stripped off the proximal segment to allow tension-free movement between the proximal and distal segment. A groove can be made with an acrylic bur in the inner aspect of the proximal segment to accommodate the IA nerve and decrease the chance of nerve compression as the proximal and distal segments are approximated and fixated.
In the case of a “bad split,” measures must be taken to correct the unfavorable split if possible. If there is a buccal cortex fracture, the fractured segment must be fixated with plates and monocortical screws to reestablish the continuity of the proximal segment. If there is a lingual cortex fracture, a bicortical fixation is necessary to secure both cortices, because it is typically not easy to plate the lingual cortex. If the split goes superiorly to the condyle, either the condyle must be fixated or the patient must be placed in maxillomandibular fixation and the procedure aborted. The condyle must be allowed to heal for at least 12 months before proceeding with mandibular osteotomy again, and computed tomography may be a better method of assessing condylar healing than plain films. Caution should be exercised when evaluating condylar healing solely based on a plain film, because it may give a false sense of security when taking the patient back to the operating room for reoperation. Patients may not display symptoms and signs of condylar dysfunction and may mask the incomplete healing of the condyle, resulting in an unstable condylar segment and potential distortion of condylar guidance during BSSO fixation.
A prefabricated surgical splint is inserted and maxillomandibular fixation wires are placed. Fixation techniques are variable depending on the surgeon’s preference, either monocortical plates and screws and/or bicortical screws, either transorally or transbucally. Following the release of maxillomandibular fixation wires, occlusion must be confirmed, and condylar seating must be checked by applying gentle posterior–superior pressure at the labiomental fold. If the mandibular midline shifts to one side, the side toward which the mandibular midline is shifting must be released and fixated again, because the condyle drops back and the dental midline shifts toward the side where the condyle was not seated properly. Incisions are closed with a resorbable running suture. Drains and pressure bandages are not necessary.
Adjunctive Technique: Midline Osteotomy
Transverse problems in dentofacial deformity are one of the most underdiagnosed and unrecognized issues that can compromise the final results after orthodontic and orthognathic surgical treatments. Often, a transverse problem is not recognized until after the surgical correction is done, making it difficult, if not impossible, to obtain an adequate buccal overjet in the posterior region that is stable long term.
Clinical scenarios in which transverse problems can be problematic are:
- •
A constricted maxillary arch (absolute transverse deficiency)
- •
A secondary posterior crossbite following mandibular advancement (relative transverse discrepancy)
Constricted Maxillary Arch
In this scenario, a two- or multipiece segmental LeFort I osteotomy would normally be the mainstream treatment depending on the degree of arch constriction, if there are other concomitant vertical, horizontal, or anterior–posterior discrepancies of the maxilla. However, if the transverse problem is the only issue with the maxilla and the mandibular advancement is warranted, then the mandibular midline osteotomy can be considered as an adjunctive procedure to BSSO.
Advantages are obvious in that surgery can be limited to one jaw, which has significant financial implications for the patient and implications for the difference in postoperative care necessary for one-jaw versus two-jaw surgery. As illustrated in the surgical technique section, the mandibular midline osteotomy adds very little to the operating time and can be performed in conjunction with the horizontal osteotomy (genioplasty) of the chin.
Secondary Posterior Crossbite with Mandibular Advancement
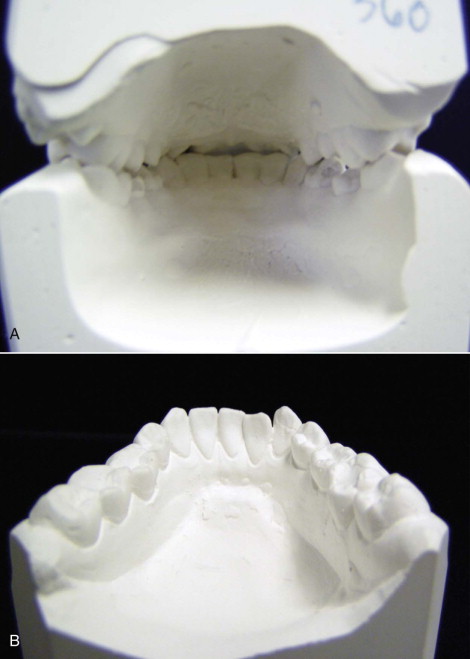
When the patient presents to the surgeon’s office ready for surgery, progress models should be taken to assess the final arch relationship. When the casts are held in Class I canine relationship, it will become apparent if there is a buccal crossbite in the molar area as the surgeon simulates the mandibular advancement. If the orthodontist has appropriately decompensated by uprighting the posterior molars and leveling the curve of Wilson, then the true extent of transverse discrepancy can be visualized. This is best evaluated by viewing the models from the back and visualizing the second molar buccal overjet ( Fig. 75-1 ). If there is a posterior crossbite or a cusp-to-cusp relationship, the surgeon then has to either consider a surgical posterior maxillary expansion to correct this problem, accept the transverse discrepancy as is, or make a more rational choice to consider the mandibular constriction. The surgeon may consider deferring surgery and request that the orthodontist do a further posterior dental expansion by tipping the maxillary molars buccally and mandibular molars lingually; however, this can prolong the treatment time, and these types of dental movements may not be stable long term. It also presents cusp interferences as the mandible is advanced, due to the inferior and buccal rotation of the maxillary palatal cusps. Posterior crossbite after orthognathic surgery is not an easy problem to correct orthodontically; it would require an extensive dental compensation, and the end results would be an unstable occlusal relationship bound to relapse.
Transverse Correction in Class II Mandibular Deficiency
Mandibular advancement tends to aggravate transverse discrepancies as the wider posterior molar segment is brought forward to occlude with the narrower portion of the maxillary arch. Minor discrepancies can be corrected with buccal and lingual crown torque of the maxillary and mandibular molars, respectively. Dental tipping tends to introduce cusp interferences, because the maxillary palatal cusps are rotated buccally and inferiorly. Such movement tends to result in a dental relapse following surgery, and it should be eliminated prior to surgical correction. This clinical dilemma has led to a search for an alternative procedure that is more stable than a segmental maxillary osteotomy.
Similar to the two-piece LeFort I widening, the magnitude of mandibular constriction increases progressively from anterior to posterior, with the greatest constriction occurring in the second molar area. Five-year follow-up shows no statistically significant relapse between the canines and first molars, but a statistically significant relapse of 0.6 mm in the second molar. However, this was clinically insignificant, because there was no incidence of posterior crossbite at the latest follow-up. The maximum, stable mandibular constriction observed is approximately 10 mm, which is comparable to the surgically assisted rapid palatal expansion (up to 14 mm expansion) and the segmental LeFort I expansion (up to 15 mm), but the latter procedures have significantly higher relapse rates of 40% to 50%, with the degree of relapse directly proportional to the magnitude of surgical expansion.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


