Immediate function with Brånemark implants is well established for the mandible. This article describes a series of 857 implants placed consecutively in which very few implants failed or lost bone despite the dynamic healing conditions of simultaneous dental extractions and bone leveling. Though these findings are relatively early, 3 years or fewer, it appears that the immediate function All-on-Four procedure can be done with a high degree of confidence for the mandible––putting into question the need for additional implants.
The original Brånemark surgical-prosthetic protocol advocated the placement of four implant fixtures for the restoration of a resorbed mandible and six implant fixtures on mandibles that demonstrated minimal to moderate resorption. Brånemark positioned the fixtures between the mental nerves, thus taking advantage of high cortical density. This symphyseal position, however, also became a limiting factor with respect to the ability to extend the prosthesis posteriorly. Vertical implant placement required the prosthesis to have cantilever lengths of 10 to 20 mm to provide adequate function and aesthetic outcome. Biomechanical studies then demonstrated that regardless of the number of implants used, cantilever spans should not exceed 7 mm to provide optimal stability as extended cantilevers demonstrate double the compressive forces on the distal-most implant.
Multiple surgical solutions arose out of the need to provide improved implant positions for the posterior mandible and decrease the length of the distal cantilever. Jensen and Nock first described repositioning of the inferior alveolar nerve (IAN) for the placement of endosseous dental implants. Brånemark and Jensen also used IAN repositioning to facilitate placement of dental implants in the atrophic posterior mandible. However, lateralizing the IAN to facilitate implant placement produced neurosensory disturbance, the recovery of which was not always certain. Therefore, nerve lateralization was rarely done.
The simple solution of placement of angled implants appeared to solve this problem as it greatly reduced cantilever length while improving anterior-posterior (A-P) spread and thereby stability of the prosthesis. Krekmanov was able to decrease the posterior cantilever length by simply tilting the distal-most implant. The angulation of the distal implant was also found to reduce tensile stress of the prosthesis. Two-dimensional finite elemental analysis showed that the use of cantilevers resulted in higher stress at the marginal bone. Reduction of the cantilever arm by the use of an apically tilted implant mitigated this stress pattern.
The use of distal-angled implants for the support of fixed hybrid prostheses has now been reported as a viable alternative to grafting and nerve lateralization. Further work by Krekmanov and Aparicio showed that tilted implants did not exhibit advanced or extreme bone loss nor did they demonstrate significant bone stress when compared with cantilevers on vertically placed implants.
The next question is: Could tilted implants be immediately loaded? Initial work on immediately loading of nonangulated mandibular implants came from Schnitman and Wohrle, reporting a 10-year experience using Brånemark implants. Since then, the concept of immediate-load full-arch splinted restorations in the edentulous mandible has been well documented by several authors with either four or six implant fixtures. A comprehensive literature review on immediately loaded edentulous mandibles revealed a success rate between 98% and 100% over 1 to 3 years based on the use of four to eight implant fixtures. The use of fewer implants was further studied by Malo and Rangert with the application of the All-on-Four concept with the use of angulated fixtures. The technique employed four NobelBiocare Speedy TiUnite fixtures (Yorba Linda, CA, USA) with two anterior vertical and two posterior 30° angled fixtures. All implants underwent immediate loading with a splinted one-piece all acrylic full-arch restoration. A 1-year follow up demonstrated a prosthesis success rate of 100% and implant success rate of 96.7% to 98.2%, respectively. Khatami and colleagues further validated the success of immediate loaded angulated implants in the edentulous mandible using the All-on-Four approach. The special category of the severely atrophic mandible was addressed by Jensen who used a variation of the All-on-Four concept termed “V-4.” This mandibular fracture-avoidance technique allowed for placement of implants in Cawood Class IV-V mandibles that had between 5 and 7 mm of basal bone available without bone grafting. All four implants were placed in a “V” formation, at 30° angles, all directed toward the symphysis where most bone mass remained.
The next question of importance was immediate loading in extraction sites: could this dependably be done? Placement of implants into immediate extraction sites had become a well accepted treatment option for single teeth but not for full-arch restorations, especially requiring multiple extractions. The survival rate for immediately placed extraction site implants was reported from 91.8% to 99.5%, ranging from 1- to 11-years follow-up. Villa and Rangert reported on placement of dental implants into compromised extraction sites and loading with a provisional all-acrylic prosthesis within 3 days postoperatively. Implant success rate at 44 months was reported at 100% with marginal bone loss of 0.5 to 0.7 mm by the first year. Similar results were reported by Grunder and, separately, by Cosci. Using standard surgical and maintenance protocol, Malo and colleagues reported a cumulative implant survival rate with immediate extraction, placement and loading of 100% after 1 year. Also, marginal bone loss was comparable to previous studies. This was a very important finding. For the first time, full-arch immediate function in the dental extraction case appeared possible. However, there have been very few reports, with only a limited number of patients, since that time. For that reason, a retrospective study was done of 219 consecutive patients treated with angled implants using All-on-Four therapy in the mandible, the majority of which required dental extraction.
Patient selection and evaluation
A retrospective study of the All-on-Four protocol was done for both dentate and edentulous patients. The series spanned a diverse patient population treated by the same surgical-prosthetic team (Dental Implant Center, Phoenix, AZ, USA) over the course of 36 months. They performed dental extractions when indicated, simultaneous implant placement, and immediate loading (within 2–3 hours postsurgery) with a fixed acrylic hybrid prosthesis. A total of 857 implants were placed in 219 mandibles, of which 201 had more than three teeth present, 18 were fully edentulous, 7 had one to three teeth, 49 had four to six teeth, and 145 had over seven teeth. All surgeries were completed under monitored IV anesthesia.
The patient selection protocol consisted of a comprehensive prosthetic examination—presurgical consultation with necessary medical and anesthesia evaluations. Only ASA I and II patients were treated as defined by the American Society of Anesthesiologists. Patients were excluded if they demonstrated poorly controlled diabetes mellitus, active neoplastic disease, or a history of bisphosphonate use with a fasting collagen telepeptide (CTx) blood level below 150 pg/mL.
The prosthetic presurgical work-up included cone-beam CT scan (CBCT), and periapical and panoramic radiographs. Impressions of the maxilla and mandible were made, along with facebow transfer and interocclusal records.
Attention was given to the rest position of the lower lip and the relation of the lip to the remaining mandibular anterior dentition, if any, or the existing prosthesis. In order to provide a satisfactory aesthetic outcome, the junction between the prosthesis and the residual ridge needed to lie at least 10 mm apical to the inferior border of the lip. This ensured enough thickness of the prosthesis for structural integrity. The anticipated bone reduction was evaluated clinically and radiographically and noted on the surgical prescription.
Radiographic evaluation
Presurgical radiographic examination included CBCT to evaluate the anatomy of the mandible. Height, width, cortical anatomy, and position of the IAN were evaluated using the CBCT software. The mandible was examined with attention given to the IAN position and its course through the mandible. The anterior loop was identified to predict the need for nerve repositioning.
The CBCT studies were assessed for osseous pathology, arch shape, and bone volume. Mandibles that displayed a U-shape were differentiated from those which had more of a V-shaped anatomy. This finding helped determine implant positioning with regard to A-P spread. Patients with a flat U-shaped anatomy were informed of the possibility of IAN repositioning to avoid straight-line implant placement.
Edentulous atrophic mandibles often presented with tubular anatomy with absent or very poor medullary trabecular bone. Hounsfield unit values in the CBCT software were used to determine the porosity of the mandible. “Hollow mandibles” required inferior border anchorage to obtain adequate stability. The other extreme, that of a completely dense cortical mandible, required careful implant site preparation including tapping. These commonly found bone density variants guided surgical osteotomy preparation to diminish the possibility of adverse outcomes. These variants however, made it impossible to have a uniform data set for evaluation of implant treatment using All-on-Four immediate function.
Reported here are findings and results of treatment of 857 consecutive implants of which 428 were angulated. Representative case reports follow.
Radiographic evaluation
Presurgical radiographic examination included CBCT to evaluate the anatomy of the mandible. Height, width, cortical anatomy, and position of the IAN were evaluated using the CBCT software. The mandible was examined with attention given to the IAN position and its course through the mandible. The anterior loop was identified to predict the need for nerve repositioning.
The CBCT studies were assessed for osseous pathology, arch shape, and bone volume. Mandibles that displayed a U-shape were differentiated from those which had more of a V-shaped anatomy. This finding helped determine implant positioning with regard to A-P spread. Patients with a flat U-shaped anatomy were informed of the possibility of IAN repositioning to avoid straight-line implant placement.
Edentulous atrophic mandibles often presented with tubular anatomy with absent or very poor medullary trabecular bone. Hounsfield unit values in the CBCT software were used to determine the porosity of the mandible. “Hollow mandibles” required inferior border anchorage to obtain adequate stability. The other extreme, that of a completely dense cortical mandible, required careful implant site preparation including tapping. These commonly found bone density variants guided surgical osteotomy preparation to diminish the possibility of adverse outcomes. These variants however, made it impossible to have a uniform data set for evaluation of implant treatment using All-on-Four immediate function.
Reported here are findings and results of treatment of 857 consecutive implants of which 428 were angulated. Representative case reports follow.
Case report I
A 75-year-old male patient presented with a diagnosis of a hopeless dentition due to severe periodontal disease ( Fig. 1 A). The past medical history was significant for well controlled Type II diabetes (A1c 6.8), hypertension, and hypercholesterolemia. He denied any drug allergies or history of smoking. His current medication included diltiazem hydrochloride 360 mg/day; lisinopril, 40 mg/day; metoprolol, 100 mg/day; glipizide, 10 mg/day; metformin, 300 mg/day; and aspirin, 81 mg /day. The surgical-restorative plan called for the removal of all remaining teeth, debridement of hard and soft tissue, mandibular alveolar reduction of 5 mm, and placement of mandibular implants using the All-on-Four technique.

The CBCT mandibular study revealed 70% to 90% bone loss on the remaining teeth without significant intrabony pathology. Approximately 14.5 mm were measured from the usable crest of the alveolus to the mental foramen bilaterally with no evidence of an exaggerated anterior IAN loop.
The intraoral examination revealed gross periodontal disease, attachment loss, and Class III mobility of the remaining teeth. The patient had been edentulous in the maxilla and partially edentulous in the mandible for 15 years. The maxillary complete denture had noticeable wear on the occluding surfaces of the mandibular anterior teeth with papillomatosis due to lack of proper fit of the prosthesis. The remaining mandibular anterior dentition had over-erupted and drifted, rendering unaesthetic diastemas and an uneven incisal plane suggesting combination syndrome. In addition, the patient had full-crown anterior tooth exposure while in repose. Bone reduction of 5 mm from the cement enamel junction of the incisors and 7 mm from the canines and first premolars was planned.
Surgical treatment was completed under IV sedation including intraoperative glucose monitoring. Teeth were removed via a periotome and forceps. Midcrestal incisions were made bilaterally from the retromolar pad to the midline within keratinized tissue. Inverse hockey incisions were made in the posterior to facilitate flap reflection. The mentalis muscle was partially reflected leaving 50% of the insertion intact. The mental nerve was identified bilaterally in relation to the distal most extraction sites. The alveolar bone shelf was prepared reducing bone level by 5 to 7 mm. The midline was identified and a 2 mm twist drill used to place the Malo guide. Posterior implant sites were developed just distal to the second premolar at 30° angles and the anterior sites at the canine-lateral incisor areas. All sites were prepared in a sequential fashion (without under preparation) using copious sterile saline irrigation. All implants placed were 4 × 18 mm NobelBiocare SpeedyGroovy RP with torque values of 45 Ncm.
Following fixture placement, straight or angulated multiunit abutments (NobelBiocare, Yorba Linda, CA, USA) were placed and torqued following manufacturer’s instructions to allow for immediate prosthetic rehabilitation with fixed acrylic prostheses followed by soft tissue management and closure.
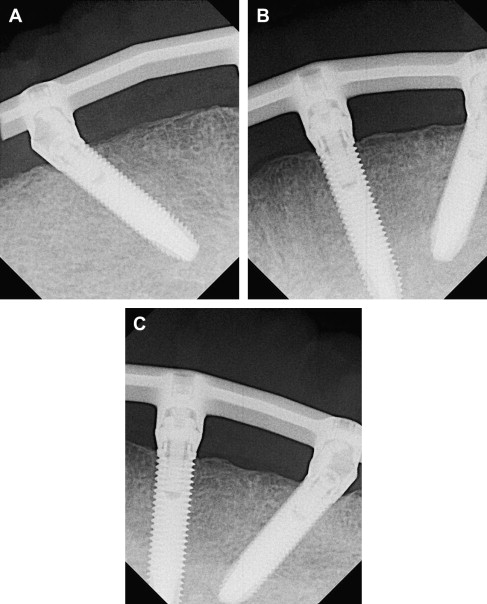
Multiunit impression copings were attached to the prosthetic abutments. An impression was made using a clear disposable tray using cartridge dispensed Aquasil Ultra Rigid Regular Set and Aquasil Ultra Deca (Dentsply Caulk, Milford, DE, USA). The impression was allowed to set, then removed and inspected for completeness. The impression was then poured using soft tissue material (Gigifast Ridgid, Zhermack Technical, Bovino, Italy) and type IV dental stone. Temporary cylinders were then connected to prosthetic abutments and luted to the mandibular complete denture using Trad (GC America, Aslip, IL, USA) acrylic resin verifying the occlusal plane orientation. The interim prosthesis was then finished on the surgical casts and delivered directly over the abutments, about 2.5 hours later. Prosthetic screws were torqued to 15 Ncm and access holes sealed with Teflon tape and Fermit (Ivoclar Vivadent AG, Liechtenstein). The occlusion of the prosthesis was designed in centric and group function. Patients were advised to eat only soft food for the first 4 months. The patient was seen for follow-up appointments after 10 days, 2 months, and 4 months. CBCT and periapical radiographs were obtained to evaluate bone healing around the dental implants (see Fig. 1 B).
Final impressions were made after 4 months of healing. At that time, maxillomandibular records were obtained with a Denar Slidematic facebow (Whip-Mix Corp, Louisville, KY, USA) and ACU-flow Bite Registration Material (Great Lakes Prosthodontics Tonawanda, NY, USA). The interim prosthesis was removed and implant stability checked manually using a torque wrench. Angulated multiunit abutments were torqued to 15 Ncm and straight abutments to 35 Ncm. A Pattern Resin LS (GC America, Aslip, IL, USA) jig over temporary copings was fixed over corresponding implants and joined with resin. After setting, final impressions were made using Imprint 3 Monophase (Medium Body) and Imprint 3 Penta Heavy Body (3M ESPE, St Paul, MN, USA) impression materials on rigid disposable trays then poured with soft tissue material and type IV dental stone. Irreversible hydrocolloid (Jeltrate Plus, Dentsply, York, PA, USA) impressions were made of the maxillary and mandibular interim prostheses and poured in type III dental stone. Casts obtained from the interim prostheses were then articulated. The master casts were cross-mounted with the interim prosthesis in place while the patient waited in the dental chair. This technique allowed for recording of the patient’s horizontal and vertical dimension of occlusion. The final prosthesis was made following NobelBiocare Procera bridge guidelines with a milled titanium framework. The occlusion was set in centric with group function for laterotrusive and protrusive excursions. The final prosthetic screws were torqued to 15 Ncm and access holes sealed with Teflon tape and composite resin. One-year postsurgical periapical radiographs were obtained and used to evaluate implant bone levels ( Fig. 2 ).
Case report II
A 47-year-old female with a nonrestorable dentition due to severe decay and periodontal disease was treatment-planned for a full-mouth extraction, debridement of soft and hard tissue, alveolar shelf preparation, placement of implants using the All-on-Four immediate load technique, and delivery of an immediate upper denture. Past medical history was noncontributory except for a one pack per day, 25-year smoking history. Her physical examination was significant for multiple decayed and fractured teeth with severe periodontal disease. Intraoral soft tissues displayed typical findings of severe periodontal disease with the remaining teeth showing gross mobility and attachment loss.
The CBCT mandibular study revealed 80% bone loss on the remaining teeth with generalized chronic periapical abscesses ( Fig. 3 ). Approximately 12 mm were measured from the usable crest of the alveolus to the mental foramen bilaterally. There was no evidence of an exaggerated anterior IAN loop.

The patient had been partially edentulous in both the maxilla and mandible for the last 20 years. The maxillary and mandibular remaining dentition exhibited generalized decay. The teeth were deemed hopeless. Bone reduction of 3 mm was planned.
The surgical procedure was completed under IV sedation. The remaining teeth and root remnants were surgically removed. Midcrestal incisions were made from the retromolar pads to the midline bilaterally with inverse distal hockey stick releases. Full-mucoperiosteal flaps were elevated lingually and labially with care to maintain keratinized tissue. The mental foramen was identified bilaterally with the dissection maintained on an equal plane of the foramen. With optimal visibility of the surgical field the extraction sites were debrided of necrotic tissue until only healthy bone was left. The All-on-Four bone shelf was developed at the predetermined level. Bone removed was saved for possible future use. A barrel acrylic bur under copious sterile saline irrigation was used to refine the bone shelf.
The midline was demarcated and distal implant sites prepared at a 30° angle. Anterior sites were developed in the lateral-canine region. Once all primary implant sites were verified as optimal for A-P spread the sites were enlarged with the 2 mm bur to a depth of 18 mm and guide pins were used to verify implant angulation. The 2.4/2.8 drills were used next to the appropriate depth. At this point the bone density was appreciated and all sites were further prepared with the 3 mm drill, except the distal sites were prepared to a depth of 13 mm. The anterior sites were further prepared with the 3.2/3.6 drill to a depth of 15 mm. Before placement all osteotomy sites were irrigated. The implants were placed and torqued to 45 Ncm. Prosthetic abutments were placed and verified against the surgical guide. Wound closure was achieved with 3.0 chromic gut in an interrupted fashion after appropriate soft tissue management.
The same prosthetic procedures described in the previous case were followed following fixture placement. One year later periapical radiographs were obtained to evaluate bone level ( Fig. 4 ).





