Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Describe the clinical and radiographic features of enamel fractures, uncomplicated crown fractures, complicated crown fractures, crown-root fractures, root fractures, concussion, subluxation, luxations (lateral, extrusive, and intrusive), avulsions, and alveolar fractures.
- 2.
Describe possible short- and long-term responses of pulp, periradicular tissues, and hard tissues to the injuries listed previously.
- 3.
List pertinent information needed when examining patients with dental injuries (health history, nature of injury, and symptoms).
- 4.
Describe the diagnostic tests and procedures used in examining patients with dental injuries and interpret the findings.
- 5.
Describe appropriate treatment strategies (immediate and long term) for various types of traumatic injuries.
- 6.
Recognize outcomes of traumatic dental injuries.
- 7.
Recognize pulp space obliteration and describe management considerations.
- 8.
Recognize surface resorption, inflammatory (infection-related) resorption, and replacement (ankylosis-related) resorption, and describe their respective treatment strategies.
- 9.
Describe the differences in treatment strategies for traumatic dental injuries in primary and permanent dentition.
Trauma to teeth involves the dental pulp and the periodontium either directly or indirectly; consequently, endodontic considerations are important in evaluating and treating traumatic dental injuries. The purpose of this chapter is to describe the incidence of dental trauma, etiologic factors, examination procedures, emergency care, treatment options, and possible sequelae in traumatized teeth. Because injuries occur to primary teeth also, a separate section has been included for these teeth. The recommendations for managing traumatic dental injuries are based on the guidelines published by the International Association of Dental Traumatology, which publishes updated guidelines on its Web site ( www.iadt-dentaltrauma.org ).
Epidemiologic studies have shown that the incidence of dental trauma ranges from 25% to 58%, and the most common age group affected is children 8 to 12 years. Sgan-Cohen and colleagues reported a total prevalence of 29.6%. Severe trauma, at least involving the dentin, was found among 13.5% and was more prevalent among children with an incisal overjet and incompetent lip. Falls were the main cause of dental trauma (44.9%), but sports and violence also were important causes. Fractures of enamel or enamel and dentin are the most common sequelae of dental trauma. The teeth most often traumatized are the maxillary central incisors (88%), maxillary laterals (7%), and mandibular incisors (5%). Among sports, basketball is associated with the highest injury rate, with an incidence of 10.6 injuries per 100 athlete-seasons among men and 5 injuries per 100 athlete-seasons among women. The incidence for basketball players was five times higher than that for football players, for whom mouthguard use is mandatory.
Age is an important factor in trauma to teeth. By age 14, about 25% of children will have had an injury involving their permanent teeth. The significance of age is a “good news/bad news” situation. The good news is that pulps in children’s teeth have a better blood supply than those in adults and better repair potential. The bad news is that root development is interrupted in teeth with damaged pulps, leaving the roots thin and weak. Cervical fractures often occur either spontaneously or from even minor injuries because of thin dentin walls. Therefore, when dental injuries occur in children, every effort must be made to preserve pulp vitality.
Classification of traumatic injuries promotes better communication and dissemination of information. The system used in this chapter is based on Andreasen and Andreasen’s modification of the World Health Organization classification ( Box 11.1 ). Feliciano and de Franca Caldas evaluated 164 articles and 54 different classifications and concluded that, according to the literature, the Andreasens’ model was the most frequently used classification system (32%). Treatment recommendations are based on the official guidelines of the International Association of Dental Traumatology (IADT).
- ▪
Enamel fracture: Involves the enamel only and includes enamel chipping and incomplete fractures or enamel cracks.
- ▪
Crown fracture without pulp exposure: An uncomplicated fracture involving the enamel and dentin with no pulp exposure.
- ▪
Crown fracture with pulp exposure: A complicated fracture involving the enamel and dentin and exposure of the pulp.
- ▪
Crown-root fracture: Tooth fracture that includes the enamel, dentin, and root cementum and may or may not include the pulp.
- ▪
Root fracture: Fracture of the root only involving the cementum, dentin, and pulp; also referred to as a horizontal root fracture.
- ▪
Luxation injuries: Tooth luxations include concussion, subluxation, extrusive luxation, lateral luxation, and intrusive luxation.
- ▪
Avulsion: Complete displacement of a tooth out of its socket.
- ▪
Fracture of the alveolar process (mandible or maxilla): Fracture or comminution of the alveolar socket or of the alveolar process.
Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Describe the clinical and radiographic features of enamel fractures, uncomplicated crown fractures, complicated crown fractures, crown-root fractures, root fractures, concussion, subluxation, luxations (lateral, extrusive, and intrusive), avulsions, and alveolar fractures.
- 2.
Describe possible short- and long-term responses of pulp, periradicular tissues, and hard tissues to the injuries listed previously.
- 3.
List pertinent information needed when examining patients with dental injuries (health history, nature of injury, and symptoms).
- 4.
Describe the diagnostic tests and procedures used in examining patients with dental injuries and interpret the findings.
- 5.
Describe appropriate treatment strategies (immediate and long term) for various types of traumatic injuries.
- 6.
Recognize outcomes of traumatic dental injuries.
- 7.
Recognize pulp space obliteration and describe management considerations.
- 8.
Recognize surface resorption, inflammatory (infection-related) resorption, and replacement (ankylosis-related) resorption, and describe their respective treatment strategies.
- 9.
Describe the differences in treatment strategies for traumatic dental injuries in primary and permanent dentition.
Trauma to teeth involves the dental pulp and the periodontium either directly or indirectly; consequently, endodontic considerations are important in evaluating and treating traumatic dental injuries. The purpose of this chapter is to describe the incidence of dental trauma, etiologic factors, examination procedures, emergency care, treatment options, and possible sequelae in traumatized teeth. Because injuries occur to primary teeth also, a separate section has been included for these teeth. The recommendations for managing traumatic dental injuries are based on the guidelines published by the International Association of Dental Traumatology, which publishes updated guidelines on its Web site ( www.iadt-dentaltrauma.org ).
Epidemiologic studies have shown that the incidence of dental trauma ranges from 25% to 58%, and the most common age group affected is children 8 to 12 years. Sgan-Cohen and colleagues reported a total prevalence of 29.6%. Severe trauma, at least involving the dentin, was found among 13.5% and was more prevalent among children with an incisal overjet and incompetent lip. Falls were the main cause of dental trauma (44.9%), but sports and violence also were important causes. Fractures of enamel or enamel and dentin are the most common sequelae of dental trauma. The teeth most often traumatized are the maxillary central incisors (88%), maxillary laterals (7%), and mandibular incisors (5%). Among sports, basketball is associated with the highest injury rate, with an incidence of 10.6 injuries per 100 athlete-seasons among men and 5 injuries per 100 athlete-seasons among women. The incidence for basketball players was five times higher than that for football players, for whom mouthguard use is mandatory.
Age is an important factor in trauma to teeth. By age 14, about 25% of children will have had an injury involving their permanent teeth. The significance of age is a “good news/bad news” situation. The good news is that pulps in children’s teeth have a better blood supply than those in adults and better repair potential. The bad news is that root development is interrupted in teeth with damaged pulps, leaving the roots thin and weak. Cervical fractures often occur either spontaneously or from even minor injuries because of thin dentin walls. Therefore, when dental injuries occur in children, every effort must be made to preserve pulp vitality.
Classification of traumatic injuries promotes better communication and dissemination of information. The system used in this chapter is based on Andreasen and Andreasen’s modification of the World Health Organization classification ( Box 11.1 ). Feliciano and de Franca Caldas evaluated 164 articles and 54 different classifications and concluded that, according to the literature, the Andreasens’ model was the most frequently used classification system (32%). Treatment recommendations are based on the official guidelines of the International Association of Dental Traumatology (IADT).
- ▪
Enamel fracture: Involves the enamel only and includes enamel chipping and incomplete fractures or enamel cracks.
- ▪
Crown fracture without pulp exposure: An uncomplicated fracture involving the enamel and dentin with no pulp exposure.
- ▪
Crown fracture with pulp exposure: A complicated fracture involving the enamel and dentin and exposure of the pulp.
- ▪
Crown-root fracture: Tooth fracture that includes the enamel, dentin, and root cementum and may or may not include the pulp.
- ▪
Root fracture: Fracture of the root only involving the cementum, dentin, and pulp; also referred to as a horizontal root fracture.
- ▪
Luxation injuries: Tooth luxations include concussion, subluxation, extrusive luxation, lateral luxation, and intrusive luxation.
- ▪
Avulsion: Complete displacement of a tooth out of its socket.
- ▪
Fracture of the alveolar process (mandible or maxilla): Fracture or comminution of the alveolar socket or of the alveolar process.
Examination and Diagnosis
Examination of a patient with dental injuries should include the history (chief complaint, history of present illness, pertinent medical history) and a clinical examination. The emphasis in this chapter is on those aspects of the examination that specifically relate to dental trauma.
Stage of Root Development and Dental Trauma
Knowledge of the developmental stages of permanent teeth is essential for clinical practice in several dental specialties because it may influence diagnosis, treatment planning, and outcomes. In 1960 Nolla published a classification system for odontogenic development based on radiographic interpretation ( Table 11.1 ). This system has been widely used, and it is particularly important for appropriate diagnosis and treatment of traumatized teeth. In 1976 Fulling and Andreasen demonstrated that the late differentiation of Aδ nerve fibers in the dental pulp could explain the lack of a reliable and predictable response of erupting and undeveloped teeth to thermal and electrical stimulation. In young patients with immature teeth, carbon dioxide (CO 2 ) snow and dichlorodifluoromethane (DDM) are the most reliable sensitivity tests, followed by electrical pulp testing and ethyl chloride and ice. Therefore, in the absence of reliable clinical tests, radiographic evidence of root development and dentin maturation during follow-up examination may be critical for providing the clinician with reliable information about the presence of a vital dental pulp.
| Classification | Description |
|---|---|
| 0 | No crypt |
| 1 | Presence of a crypt |
| 2 | Initial calcification |
| 3 | One-third crown completed |
| 4 | Two-thirds crown complete |
| 5 | Crown almost completed |
| 6 | Crown completed |
| 7 | One-third root completed |
| 8 | Two-thirds root competed |
| 9 | Root almost open (open apex) |
| 10 | Root apex completed |
History
Pertinent information about traumatic injuries should be obtained expeditiously by following a system.
Chief Complaint
The chief complaint is simply a statement, in the patient’s (or parents’) own words, of the current problem; for example, “I broke my tooth,” or “My tooth feels loose.” It may also be unstated, as in a patient with obvious injuries.
History of Present Illness
To obtain the history of the present illness (injury), the dentist can ask a few specific questions, such as the following.
- ▪
When and how did the injury occur? The date and time of the accident are recorded. The record should include how the injury took place (i.e., bicycle accident, playground, sports, violence, or other). Such information is useful in the search for avulsed teeth and embedded tooth fragments, assessment of possible contamination, determination of the time factor with respect to the choice of treatment and the healing potential, and completion of accident reports.
- ▪
Have you had any other injuries to your mouth or teeth in the past? Individuals may have repeated traumatic injuries if they are accident prone or participate in contact sports. Crown or root fractures may have occurred as a result of an earlier injury but are observed at a later time. A history of previous episodes of trauma may affect the healing potential of the pulp and periodontium. It should also raise concern about the possibility of physical abuse of a child.
- ▪
What problems are you now having with your tooth or teeth? Pain, mobility, and occlusal interference are common symptoms. The patient’s description of symptoms aids diagnosis.
Medical History
The patient’s medical history is often significant. For example, the patient may have an allergy to prescribed medication, may be taking medications that interact with proposed new medications, or may have a medical condition that affects treatment. The patient’s tetanus immunization status should be recorded; a booster may be indicated with contaminating injuries, such as avulsions and penetrating lip and soft tissue lesions.
The need for neurologic evaluation should always be considered and ruled out. Concussion is a disturbance in brain function caused by direct or indirect force to the head. It is a functional, rather than structural, injury that results from shear stress to brain tissue caused by rotational or angular forces; direct impact to the head is not required. Headache is the most common symptom of concussion, although a variety of clinical domains (e.g., somatic, cognitive, affective) can be affected ( Box 11.2 ). Signs and symptoms are nonspecific; therefore, a temporal relationship between an appropriate mechanism of injury and the symptoms must be determined. In cases in which a head concussion is suspected, the patient should be immediately referred for a full neurologic examination.
Affective/emotional symptoms
Cognitive symptoms
Sleep
Somatic/physical symptoms
- ▪
Blurred vision
- ▪
Convulsions
- ▪
Dizziness/poor balance
- ▪
Fatigue
- ▪
Headache
- ▪
Lightheadedness
- ▪
Light sensitivity
- ▪
Nausea
- ▪
Noise sensitivity
- ▪
Numbness/tingling
- ▪
Tinnitus
- ▪
Vomiting
Clinical Examination
The lips, oral soft tissues, and facial skeleton should be examined, in addition to the teeth and supporting structures.
Soft Tissues
The purpose of the soft tissue evaluation is to determine the extent of tissue damage and to identify and remove foreign objects from wounds. In crown fractures with adjacent soft tissue lacerations, wounds are examined visually and radiographically for tooth fragments. Lips are likely areas for a foreign body impaction. Also, severe lacerations require suturing ( Fig. 11.1 ).

Facial Skeleton
The facial skeleton is evaluated for possible fractures of the jaw or alveolar process. Such fractures, when they involve tooth sockets, may produce pulpal necrosis in teeth associated with fracture lines. Alveolar fractures are suspected when several teeth are displaced or move as a unit; when tooth displacement is extensive; when occlusal misalignment is present; or when there is continuous bleeding from gingival tissues.
Teeth and Supporting Tissues
Examination of teeth and supporting tissues should provide information about damage that may have occurred to dental hard tissues, pulps, periodontal ligaments, and bony sockets. The following sections present guidelines for a method of collecting information systematically.
Mobility
The clinician examines the teeth (gently) for mobility, noting whether adjacent teeth also move when one tooth is moved (indicating an alveolar fracture). The degree of horizontal mobility is recorded: 0 for normal mobility; 1 for slight mobility (less than 1 mm), 2 for marked mobility (1 to 3 mm); and 3 for severe mobility (greater than 3 mm), both horizontally and vertically. If there is no mobility, the teeth are percussed for sounds of ankylosis (metallic sound). Absence of normal mobility may indicate ankylosis or “locking” of the tooth in bone, such as with intrusion and lateral luxation.
Displacement
A displaced tooth has been moved from its normal position. If this occurs as a result of a traumatic injury, it is referred to as luxation (discussed later in the chapter).
Periodontal Damage
Injury to the supporting structures of teeth may result in swelling and bleeding involving the periodontal ligament. The involved teeth are sensitive to percussion, even light tapping. Apical displacement with injury to vessels entering the apical foramen may lead to pulp necrosis if the blood supply is compromised.
The use of percussion can help identify periodontal injury. This testing procedure must be done gently because traumatized teeth are often exquisitely painful to even light tapping. In a combined histologic, bacteriologic, and radiographic study, Andreasen showed that only tenderness to percussion at the time of diagnosis of pulp necrosis was related to an infected, necrotic pulp. Therefore, special attention should be given to this test, especially when the tooth consistently and reliably shows an abnormal tenderness to percussion. Uninjured teeth should be examined first to enhance the patient’s confidence and understanding of the procedures. In addition to testing the tooth or teeth involved in the patient’s complaint, it is important to include several adjacent and opposing teeth. This permits recognition of other dental injuries of which the patient may not be aware and that may not be obvious clinically. If later complications develop involving one of these adjacent or opposing teeth, previous information aids diagnosis.
Pulpal Injury
The ideal pulpal response to injury is complete recovery after a traumatic injury. Two other potential outcomes may occur: calcific metamorphosis, in which the pulp tissue is gradually replaced with calcified tissue (recognized clinically as a yellowing effect on the crown) or pulp necrosis, which can result in external inflammatory (infection-related) root resorption. Rarely, resorption may occur in the pulp space (internal resorption). In any case, a tooth may undergo resorption without any clinical symptoms, which emphasizes the need for follow-up controls.
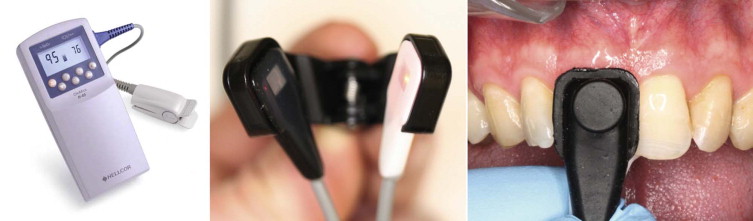
The status of the pulp may be determined by the symptoms, history, and clinical tests (see Chapter 5 ). However, two clinical tests deserve consideration here because of their applicability to traumatized teeth: the electrical pulp test (EPT) and the cold test with dichlorodifluoromethane (DDM) (Endo-Ice; Hygenic Corp., Akron, Ohio). These test the neural tissue (specifically Aδ nerves) within the pulp chamber and are generally reliable for evaluating and monitoring pulpal status except in teeth with incomplete root development. Nevertheless, evaluating the vascular supply to the pulp is the ultimate test to determine vitality of the tissue. Current evidence demonstrates that pulpal blood flow can be accurately assessed with laser Doppler flowmetry (LDF) and with pulse oximetry ( Fig. 11.2 ). Gopikrishna and colleagues compared the efficacy of a custom-made pulse oximeter dental probe with EPT and thermal testing for measuring the pulp vitality status of recently traumatized permanent teeth. The results demonstrated a positive responsiveness to thermal and electrical pulp tests that increased from no response on day 0 to 29.4% teeth on day 28, 82.35% of teeth at 2 months, and 94.11% teeth at 6 months. However, the pulse oximeter gave positive vitality readings that remained constant over the study period from day 0 to 6 months in all patients.
Radiographic Examination
Radiographs can reveal fractures of bone and teeth and the stage of root development. Horizontal root fractures and lateral luxations are often overlooked because the conventional angle may miss irregularities that are not parallel with the x-ray beam. Therefore, multiple exposures should be routine for examination of traumatized teeth to ensure complete disclosure and diagnosis of the injury.
The film size should be such that it can accommodate two incisors without bending or distorting the image. It is also important to use a film holder whenever possible to achieve standardized radiographic images, especially for subsequent comparisons.
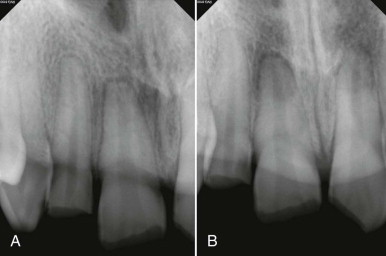
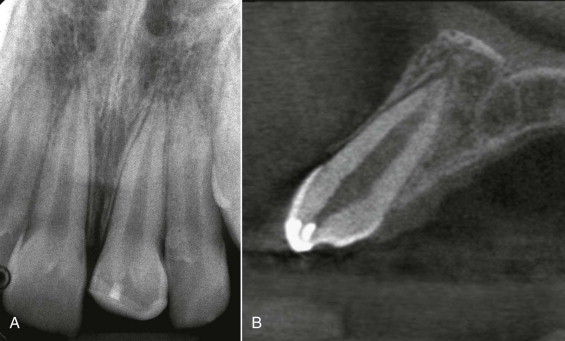
Recent improvements in three-dimensional (3D) digital radiographic imaging have introduced a new perspective, allowing us to evaluate the anatomic structures, both hard and soft tissue, in three spatial planes. The traditional projection (plain film) radiograph is a two-dimensional shadow of a three-dimensional object; 3D imaging overcomes this major limitation by providing a true representation of the anatomy while eliminating superimpositions. Several studies have reported the use of computed tomography (CT) and digital radiography for differential diagnosis, assessment of treatment outcomes, endodontics, oral and maxillofacial surgery, implantology, and orthodontics, with reliable linear measurements for reconstruction and imaging of dental and maxillofacial structures. The indications for cone beam computed tomography (CBCT) in dental traumatology were first described in 2007. Cases that may appear straightforward on periapical radiographs ( Fig. 11.3 ) may reveal a different and more complex situation when evaluated three-dimensionally ( Fig. 11.4 ).

A thorough examination and accurate records form the basis for an appropriate treatment plan. The information gathered also provides content for accident reports that may be requested either immediately or later for legal or insurance purposes.
Injuries to the Hard Dental Tissues and the Pulp
Enamel Fractures
Chips and cracks confined to enamel do not in themselves constitute a hazard to the pulp. The prognosis is good; however, the injury that produced the fracture may also have displaced (luxated) the tooth and damaged the blood vessels supplying the pulp. If the tooth is sensitive to percussion or if there are other signs of injury, the clinician should follow the recommended guidelines, according to the type of trauma (i.e., subluxation, luxation) (presented later in the chapter). Grinding and smoothing the rough edges or restoring lost tooth structure may be all that is necessary.
Uncomplicated Crown Fractures
Description
Uncomplicated crown fractures involve enamel and dentin without pulpal exposure. Such injuries are usually not associated with severe pain and generally do not require urgent care. The prognosis is good unless there is an accompanying luxation injury, in which case the tooth may be sensitive to percussion. If it is, the outlined recommendations should be followed according to the diagnosis and type of trauma (presented later in the chapter) must be followed.
Treatment
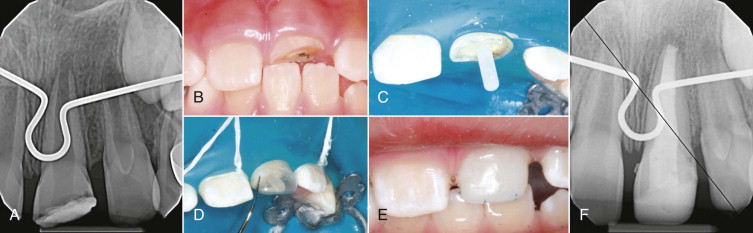
Since the advent of the acid-etch technique, conservative restoration of crown-fractured incisors with composite resin has become possible without endangering the pulp ( Fig. 11.5 ). More conservative yet is reattachment of the separated enamel-dentin fragment. This requires application of a dentin bonding agent after the enamel has been acid-etched to improve the fracture strength of the restored incisor. Both clinical experiments and bonding studies have indicated that reattachment of dentin-enamel crown fragments is an acceptable restorative procedure and does not threaten pulp vitality. In general, fracture bonding represents an advance in the treatment of anterior fractures. The dental anatomy is restored with a normal tooth structure that abrades at a rate identical to that of the adjacent non-injured teeth. Also, pulpal status may be reliably monitored.

Chair time for the restorative procedure is minimal. The use of indirect veneering techniques at a later date to reinforce bonding or to restore the fractured incisor is a conservative approach to improving esthetics and function.
Complicated Crown Fractures
Description
Complicated crown fractures involve the enamel, dentin, and pulp. Because the pulp is exposed, the fracture is considered complicated. The extent of fracture, the stage of root development, and the length of time since injury are noted.
Considering the extent of fracture helps to determine pulpal treatment and restorative needs; a small fracture may undergo vital pulp therapy and can be restored by an acid-etched composite restoration. An extensive fracture may require root canal treatment with a post and core–supported crown, depending on the age of the patient ( Fig. 11.6 ).
The stage of root maturation is an important factor in choosing between pulpotomy and pulpectomy. Immature teeth have thin-walled roots; every effort should be made to preserve the pulp to allow continued root development. The best technique for achieving this goal is a shallow (partial) pulpotomy (described later in the chapter). Vital pulp therapy followed by acid-etched composite restoration or reattachment of the fractured segment also is often feasible in mature teeth. However, if the extent of tooth loss dictates restoration with a crown, root canal treatment is recommended.
The time lapse between injury and examination may directly affect pulpal health. In general, the sooner a tooth is treated, the better the prognosis for preserving the pulp. However, as a rule, pulps that have been exposed for less than a week can be treated by pulpotomy. Successful pulpotomy procedures after pulp exposure of several weeks’ duration have been reported.
Treatment of Crown Fractures
Teeth with crown fractures and exposed pulps can be treated by pulp capping, pulpotomy (vital pulp therapy), or root canal therapy before restoration of lost tooth structure. If vital pulp therapy is planned, it is important to perform treatment as soon after the injury as possible.
Vital Pulp Therapy
The main reason for recommending vital pulp therapy in a tooth with an exposed pulp is to preserve the vitality of the pulp. This is particularly important in immature teeth, in which continued root development results in a stronger tooth that is more resistant to fractures than one with thin root walls.
In the past, pulpotomy meant removal of pulp tissue to or below the cervical level. Loss of pulp tissue in that area prevents dentin formation, which results in a weakened tooth that is more prone to fracture. In recent years, a more conservative and shallow pulpotomy has been popularized by Cvek and has sometimes been referred to as the Cvek technique. This shallow, or partial, pulpotomy preserves all the radicular and most of the coronal pulp tissue, allowing more hard tissue to develop in the root.
The pulp may need to be removed to or below the cervical level when the entire crown of an immature tooth fractures. Pulpotomy then is performed to encourage enough additional root development to allow subsequent crown restoration or post and core construction to support a crown. These situations are relatively uncommon. In recent years, the technique has been modified to use mineral trioxide aggregate (MTA; e.g., ProRoot MTA [Tulsa Dental Products, Tulsa, Oklahoma]) instead of calcium hydroxide.
Case Selection
Both immature and mature teeth that can subsequently be restored with acid-etched composite can be treated with a shallow (partial) pulpotomy. In general, immature teeth are more likely to be involved for the reasons stated previously.
Technique
The shallow (partial) pulpotomy procedure ( Fig. 11.7 ) starts with induction of anesthesia and rubber dam isolation. The exposed dentin is washed with saline or sodium hypochlorite solution. Extruding granulation tissue is removed with a spoon excavator from the pulp wound site; this provides an opportunity to determine more accurately the size and location of the exposure. Next, pulp tissue is removed to a depth of about 2 mm below the exposure. This relatively small amount of pulp removal is the reason the procedure is called a shallow or partial pulpotomy.
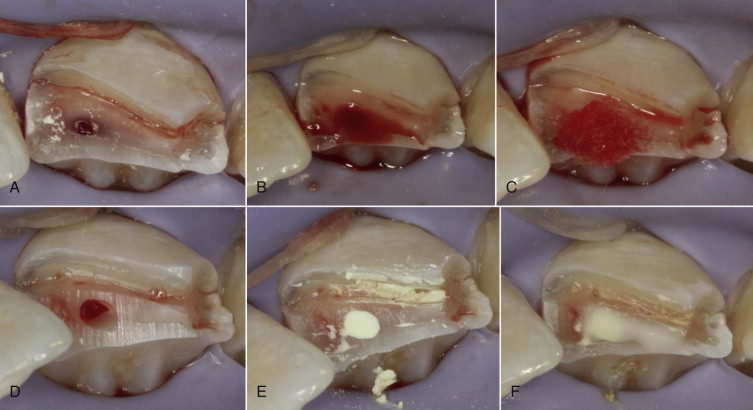
The procedure is accomplished using a water-cooled small round diamond (about the size of a No. 2 or No. 4 round bur) in the high-speed handpiece. Gently and gradually, the surface layers of pulp tissue are wiped away, beginning at the exposure site and extending into the pulp to a depth of about 2 mm below the exposure site.
After the pulp has been amputated to the desired level, a dentin shelf is created surrounding the pulp wound. The wound is gently washed with sterile saline, and hemostasis can usually be expected within 5 minutes. Then the wound is washed again to remove the clot and is dressed with calcium hydroxide. The remainder of the cavity is carefully sealed with hard-setting cement, such as glass ionomer. When the cement has set, the tooth may be restored with acid-etched composite.
Because calcium hydroxide liners disintegrate with time, whenever possible the tooth should be reentered after 6 to 12 months to remove the initial calcium hydroxide layer and replace it with a dentin bonding material. This prevents microleakage at the site where the initial calcium hydroxide has deteriorated and produced a space between the new dentin bridge and the covering restoration.
If MTA is used in place of calcium hydroxide, it is not necessary to wait for bleeding to stop completely. The material requires moisture for curing and can be placed directly onto the pulp tissue. Care must be taken to reduce the risk of forcing the material into the pulp proper; the clinician should gently dab small increments of the material onto the pulp using a moist cotton pellet. The pulpotomy space is filled with MTA white powder so that it is completely flush with the fractured dentin surface. The material is then allowed to cure, which may take 4 to 6 hours. During the curing time, it is not necessary to protect the material with a restoration, but the patient must avoid using the tooth. After curing, the tooth may be restored either with a composite resin or by bonding the fractured crown segment back onto the tooth. It is not necessary to subsequently reenter the tooth, because MTA is stable and does not break down in the manner of calcium hydroxide.
Treatment Evaluation
Treatment is evaluated after 6 months and then yearly. Successful shallow pulpotomy procedures may be considered definitive treatment and have a very good long-term success rate ( Fig. 11.8 ).
Root Canal Therapy
Teeth with mature roots may undergo either pulpotomy or root canal therapy; root canal therapy is usually necessary to accommodate prosthetic requirements. For example, if the crown has fractured in the gingival margin region, root canal treatment allows post and core and crown placement.
Crown-Root Fractures
Description
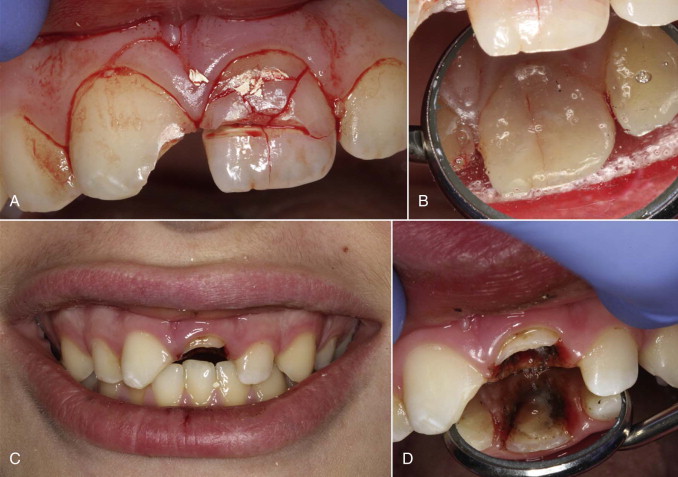
Crown-root fractures are usually oblique and involve both the crown and the root. Anterior teeth show the so-called chisel-type fracture, which splits the crown diagonally and extends subgingivally to a root surface. This type of fracture resembles a crown fracture but is more extensive and more serious because it includes the root. Another variation is the fracture that shatters the crown ( Fig. 11.9 ). The pieces are held in place only by the part of a fractured segment still attached to the periodontal ligament. In all of these fractures, the pulp is usually exposed.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


