Fig. 16.1
Syllable intelligibility in 27 maxillectomized patients
Fig. 16.2
Speech intelligibility in 27 maxillectomized patients
Xerostomia is also a common side effect of radiation treatment secondary to inadequate salivation. Xerostomia may affect the resonance of sound through dry vocal tract and articulation produced by dry oral structures. An oral moisture-checking device (Mucus™) was developed in Japan (Fig. 16.3). Xerostomia can be quantitatively evaluated using this instrument. Future research using a sophisticated acoustic signal analyzer (Fig. 16.4) and an oral moisture-checking device will reveal the relationship between xerostomia and speech affected by xerostomia.
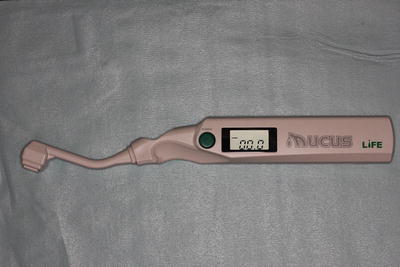
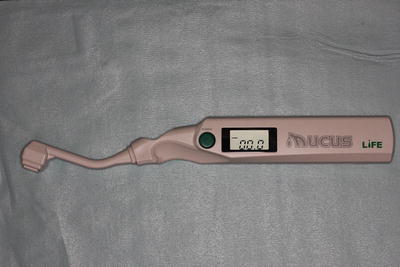
Fig. 16.3
Oral moisture-checking device (Mucus™)
Fig. 16.4
An example of the three-dimensional display of speech sound analyzed using Hilbert transform
This chapter focuses on articulation and resonance that are most frequently affected by treatment of oral cancer. Evaluation of speech in oral cancer patients is also introduced.
16.2 Articulation
Adequate control of the lips, tongue, and soft palate is crucial for the production of intelligible speech. Any impairment in the range of motion, strength, and/or flexibility of these dynamic articulators may affect the ability to make the precise individual speech movements and coarticulations needed in connected speech. The resulting articulatory impairments typically cluster along placement, manner, and/or voicing parameters as opposed to misarticulation of an individual or isolated phoneme.
Management of articulatory deficits that may develop following oral cancer treatments typically follows five paradigms: oral facilitative exercise, directed articulation therapy, compensatory technique, surgical procedure, and prosthetic appliance.
16.2.1 Oral Facilitative Exercises
Oral facilitative exercises are generally prescribed exercises designed to increase strength, range of motion, and flexibility of the oral articulators. These exercises may also improve swallowing function, as adequate control of the oral musculature is necessary to prepare and propel a bolus from the oral cavity to the oropharynx. In a study of 102 patients who received range-of-motion exercises following surgical treatment for oral and oropharyngeal cancer, significant differences in global measures of swallowing and improvement in speech intelligibility were found at 3 months posttreatment [2].
Muscular strength and endurance can be improved through three basic types of exercises: isometric, isotonic, and isokinetic.
Isometric, or static, training involves resistance without movement [3]. An example of an isometric exercise to increase tongue strength would be to push the dorsum of the tongue against the palate as hard as possible. Clark has found that maximal isometric contractions of 6-s duration repeated 5–10 times daily produce the best results [4] (Figs. 16.5 and 16.6). Atha has studied the effects of isometric exercises and found that they should be performed at maximal effort, last long enough to involve all muscle fibers, and be repeated several times daily [5]. Isometric exercise can also be used to develop increased range of motion.



Fig. 16.5
Lip-strengthening exercise (button-pull exercise). Maximal effort for lip closure lasts 6 ~ 10 s. This exercise is repeated 6–10 times a day

Fig. 16.6
Lip-strengthening exercise (blade-holding exercise). Maximal effort for lip closure lasts 6 ~ 10 s. This exercise is repeated 6–10 times a day
Isotonic, or dynamic, exercises use the principles of resistance with added motion. Lifting an object is an example of isotonic contractions. This exercise requires both a concentric or shortening contraction of the muscles and an eccentric or lengthening contraction. The advantage of this type of exercise is that it strengthens the targeted muscle through a range of motion as opposed to a static point.
Isokinetic exercises combine resistance techniques at a constant speed of repetition. The target muscle shortens against an accommodating resistance that matches the force produced by the muscle throughout full range of motion [6]. An example of this type of exercise applied to improving tongue motion and strength might be to forcefully move the tongue laterally while applying a resisting pressure from the back of a metal spoon at a constant speed of repetition. Each of three basic types of exercises including isometric, isotonic, and isokinetic exercise is also very effective on the improvement of dysphagia following treatment for oral cancer.
A tongue pressure-measuring device consisting of a disposable probe and manometer was developed in Japan (Figs. 16.7 and 16.8). A labial closure strength device consisting of an indicator with a lip holder mounted to the sensor was also developed in Japan (Figs. 16.9 and 16.10). Using these measuring devices, the effectiveness of applied exercises can be evaluated quantitatively and easily.
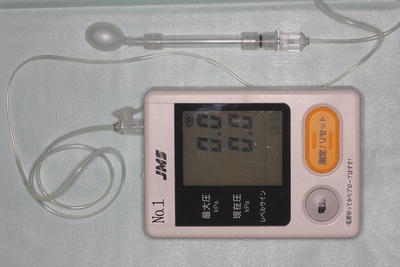
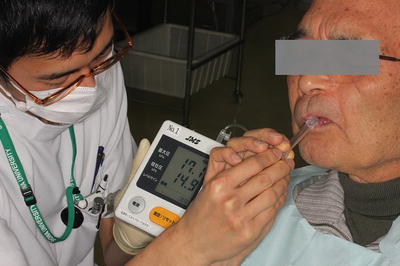


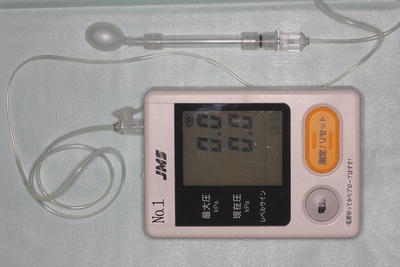
Fig. 16.7
A tongue pressure-measuring device (JMS tongue pressure measurement device™)
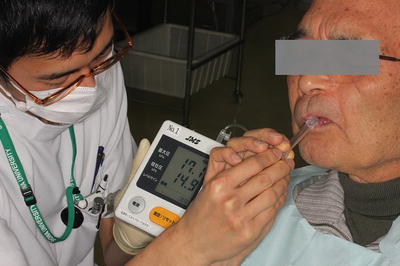
Fig. 16.8
Measurement of the maximal tongue pressure (JMS tongue pressure measurement device™)

Fig. 16.9
A lip closure strength indicator [Lip De Cum®] with a lip holder [Ducklings®] mounted to the sensor

Fig. 16.10
Measurement of the maximal lip closure strength
In addition to strength and range of motion, rapidity, flexibility, and motor skill exercises may be performed to improve the ability to quickly move from one articulatory position to another as accurately as possible. Rapid productions of consonant-vowel syllables may assist not only production of the targeted sound but also the ability to make the rapid adjustments needed for coarticulation. Oral diadochokinetic rate can be easily measured using a measuring device developed in Japan. Using this instrument, improvement in rapid oral motor skills can be assessed quantitatively and easily (Figs. 16.11 and 16.12).



Fig. 16.11
An oral diadochokinetic rate-measuring device (Kenkokun™)

Fig. 16.12
Measurement of oral diadochokinetic rate
16.2.2 Directed Articulation Therapy
Directed articulation therapy is frequently indicated to improve production of specific phonemes and phoneme groups. Patients who have undergone anterior or lateral tongue resections may have difficulty with sounds requiring tongue elevation and/or protrusion. The ability to generate adequate oral air pressure for production of fricatives and plosives may also be compromised in patients who have undergone base-of-tongue resections, as the remaining tongue tissue may not be able to produce adequate and controlled forceful movements. Patients with lip incompetence following lip resections or neural compromise to that area may experience difficulties with bilateral sounds and developing adequate lip plosion. Traditional articulation therapy with lip closure exercise may improve the production of these groups of sounds.
16.2.3 Compensatory Technique
Compensatory technique may need to be considered when the patient does not have the potential for correct placement of a targeted sound or group of sounds. For example, patients who have undergone extended tonsillar/palatal resections with base-of-tongue involvement may be unable to produce velar consonants even after directed articulation therapy; they may, however, be able to substitute a cough-like sound for the targeted /k/ sound, which facilitates adequate intelligibility. It is interesting to note that compensatory patterns differ between patients who have undergone total glossectomy versus those that have had a partial glossectomy. Partial glossectomees have been found to make use of the residual tongue stump in adaptive movements approximating the normal movement, whereas total glossectomees use true compensatory strategies.
The primary purpose of the compensatory strategy is to improve the intelligibility of speech in the most inconspicuous manner possible. Some compensatory strategies are developed unconsciously by the patient.
16.2.4 Surgical Procedures
Although complete tumor removal remains the prime objective during major oral cancer surgery, the emphasis is also on immediate functional restoration through primary reconstruction.
The type and extent of the surgical procedure have to be weighed against the patient’s prognosis, extent of disease, and other comorbid factors influencing wound healing (e.g., history of radiation, chemotherapy, or diabetes).
The type of procedure used to reconstruct surgical defects in the oral and pharyngeal cavities may affect the strength, motion, and flexibility of the oral articulators as well as the shape of the resonating cavities. In general, the quality of life following radical surgery of the oral cavity is largely dependent on the adequacy of reconstruction. Small lesions can frequently be managed with primary suture or split-thickness skin graft. In larger lesions, local or distal flaps may be required. Secondary surgical procedures that may improve tongue mobility may also enhance the oropharyngeal resonating cavity (in the case of strictures) or improve velopharyngeal incompetence (VPI) and articulation after major oral surgery.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


