5Management of Biological Complications
Therapy of peri-implant mucositis should be considered as a preventive measure for the onset of peri-implantitis (Salvi and Zitzmann 2014). Treatment of peri-implant mucositis includes a thorough removal of the supra- and submucosal peri-implant biofilm in combination with reinforcement of self-performed oral hygiene. Non-surgical mechanical removal of calculus and biofilm can be performed using a range of instruments, including hand curettes and ultrasonic devices with plastic, carbon-fiber, or titanium tips. Peri-implant biofilms can also be removed using air-abrasive devices, Erbium-YAG lasers, photodynamic therapy, or rubber polishing cups. The clinician should choose a method that minimizes damage to the surface of the transmucosal parts of the prosthesis or implant. Antiseptics such as chlorhexidine solution or gel can also be recommended as an adjunct to mechanical cleaning.
Importantly, if contributing factors such as an ill-fitting or overcontoured prosthesis, a loose abutment or screw, or the presence of a foreign body are identified, these must be corrected in order to achieve a satisfactory treatment outcome.
Peri-implant mucositis is considered to be a reversible condition, as was demonstrated in an experimental human study where clinical signs of peri-implant inflammation (bleeding on probing) resolved when oral hygiene was reinstated after a period of three weeks of undisturbed plaque accumulation (Salvi and coworkers 2012).
Studies evaluating various treatment protocols using a variety of antiseptic agents and toothpastes have shown significant clinical improvements with a reduction in bleeding on probing, and probing depths following treatment (Figs 1a-c and 2a-b).
However, in these studies complete resolution of the peri-implant mucositis in all cases is infrequently reported. The location of the implant-supported restoration margin may influence the treatment response. This was shown in a clinical study where implants diagnosed with peri-implant mucositis with submucosal restoration margins had less favorable treatment outcomes compared to those with equi- or supramucosal margins (Heitz-Mayfield and coworkers 2011).
The use of systemic antibiotics for the treatment of peri-implant mucositis is not justified (Hallström and coworkers 2012).

5.2Treatment of Peri-implantitis
Once a patient is diagnosed with peri-implantitis, it is important to implement an anti-infective treatment protocol. If left untreated, it is likely that there will be progression of bone loss and possible eventual loss of the implant.
The primary goal of peri-implantitis treatment should be to establish healthy peri-implant tissues. A cause-related treatment approach is required, aimed at resolution of the infection and the prevention of disease progression. Secondary goals may include peri-implant bone regeneration and fill of the intrabony defect.
There are many different peri-implantitis treatment approaches reported in the literature; however, it is not yet known which is the most effective (Esposito and coworkers 2012).
A recent systematic review prepared for the 5th ITI Consensus Conference identified a number of study protocols where successful treatment outcomes were achieved in the majority of patients at twelve months (Heitz-Mayfield and Mombelli 2014). This systematic review also found that, while favorable short-term outcomes were documented in many studies, a lack of disease resolution as well as progression and recurrence of the disease and implant loss despite treatment were also reported (Heitz-Mayfield and Mombelli 2014).
The following sequence of treatment is recommended, based on similarities in the treatment approaches between studies included in this systematic review (Heitz-Mayfield and coworkers 2014):
•Assessment of the peri-implant soft tissues, bone levels and the prosthesis in order to make a diagnosis and to establish the cause of the infection.
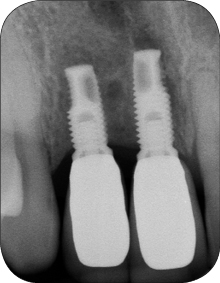
A correctly aligned radiograph showing the marginal bone levels should be made and clinical probing measurements recorded. This will give an indication of the severity of the bone loss, and allow identification of any hardware or technical complication that may manifest itself as a biological complication, for example an inadequate fit of prosthetic components. In addition, obtaining previous radiographic records from the time of the prosthesis insertion will allow a comparison with the current marginal bone levels.
•Reduction of risk factors for peri-implant infection—in particular poor oral hygiene, inadequate prosthesis design, tobacco use, presence of periodontal diseases and systemic diseases that may predispose to peri-implant infection.
Treatment may include:
– Smoking cessation counseling
– Periodontal therapy in partially dentate patients with the presence of pockets greater than 5 mm, with concomitant bleeding on probing
– Individual oral hygiene instructions
•If the prosthesis is screw-retained, it may have to be removed to assess the prosthetic components or modify the prosthesis’ contours. Removal may also improve access to the implant surface for subsequent debridement.
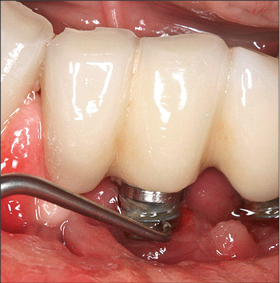
Non-surgical debridement should be aimed at the removal of calculus and biofilm supramucosally, and on the contaminated implant surface if accessible (Figs 3 and 6a-b). This can be achieved using a range of instruments including curettes or ultrasonic instruments with carbon-fiber or plastic tips (Fig 3), air-abrasive devices using sodium bicarbonate or glycine powder (Fig 4), Er:YAG lasers, or photodynamic therapy.
Due to the topography of the implant and the limited access to the implant surface, care should be taken using instruments submucosally in deep pockets to avoid breakage of the instrument, or damage to the surrounding tissues.
Antiseptics (e.g. chlorhexidine), local antimicrobials (e.g. minocycline-HCL microspheres) (Figs 5a–b), or systemic antimicrobials may be used in conjunction with the non-surgical debridement. The severity of the peri-implantitis lesion appears to play a role in the success of non-surgical therapy, with a more favorable treatment outcome at implants without advanced bone loss and without deep peri-implant probing depths.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses