Ten percent of all non-fatal ballistic injuries involve the face. Management of these wounds is challenging because of the complex functional anatomy, mechanisms of injury, extensive composite tissue destruction, and uncertain prognosis. If not treated promptly and aggressively, tissue necrosis, infection, and scar contracture result. The approach to assessment and management of avulsive gunshot wounds to the face has changed in recent decades as our understanding of the mechanisms of tissue injury, diagnostic tools, and reconstructive options have improved.
Etiopathogenesis/Causative Factors
Ballistic wounds are highly heterogeneous because of the complex interaction between the projectile and the tissues penetrated. Handguns, shotguns, and other firearms can produce different injury patterns. An understanding of the factors that determine the severity of ballistic wounds and how these factors are interrelated is critical for effective treatment of ballistic trauma. Wounds can generally be classified by the amount of energy imparted to create the wound. Projectile energy is calculated as kinetic energy according to the formula KE = ![]() mv 2 . Ballistic injuries are classified as low energy (speed <1200 ft/s) or high energy (speed >2000 ft/s). High-energy injuries have greater capacity for tissue damage and devascularization, although there are many other factors that determine actual wound severity and prognosis.
mv 2 . Ballistic injuries are classified as low energy (speed <1200 ft/s) or high energy (speed >2000 ft/s). High-energy injuries have greater capacity for tissue damage and devascularization, although there are many other factors that determine actual wound severity and prognosis.
First, it should be noted that the kinetic energy equation simply estimates the maximum energy available—it does not calculate the energy dissipated within the target, which would be a much more complex mathematic function and would need to include not only projectile mass and velocity but also the size and shape of the projectile, its propensity for deformation and fragmentation, the amount of deflection of the projectile, and the exit velocity of the projectile. The shape of the projectile and its deflection (yaw, precession, and tumble) affect the amount of drag encountered while passing through tissues. Drag is a key mechanism of energy exchange. If the bullet deforms easily, it becomes wide and flat, thereby presenting a wider cross-sectional area and thus increasing drag. Fragmentation of the projectile increases yaw, deflection, and tissue drag and results in a larger wound. If the round passes completely through the body, whatever kinetic energy it retains reduces the maximum potential of the wound. To illustrate this point, it is useful to compare a shotgun with a rifle. Shotgun pellets travel at approximately 1200 ft/s, whereas rifled weaponry can fire high-velocity rounds well in excess of 2000 ft/s. A shotgun blast at close range, however, produces a more devastating wound than a high-velocity rifle at the same distance does. Shotgun pellets are soft with low mass and thus produce a wide wound with extensive soft tissue damage. Rifle ammunition is solid with hard tips or casings that resist deformation and fragmentation and consequently result in less tissue drag. This favors deep penetration with limited dissipation of energy. Handguns have a variety of munitions that produce variable wounding patterns. However, few handguns are capable of achieving greater than 1200 ft/s and therefore produce low-energy wounds with limited capacity for avulsion injuries and progressive necrosis.
Pathologic Anatomy
Gunshot wounds may be classified into four major patterns of involvement: frontal cranium, orbit, lower mid-face, and mandible. Shotgun wounds, however, are best characterized by the region of tissue loss, with the patterns being (1) lateral mandible, (2) central face, (3) lateral mid-face and orbit, and (4) lateral cranium and orbit.
Ballistic wounds generally demonstrate the following features:
- •
Penetration is the maximum depth that the projectile reaches in tissues. It is affected by projectile momentum and drag of the tissues on the bullet.
- •
Permanent cavity refers to tissue destruction as a result of direct passage of the projectile and its fragments. It is determined by penetration, the cross-sectional area of the projectile, yaw, precession, and deformation.
- •
Temporary cavity is the transient radial deformation of tissues adjacent to the permanent cavity as the projectile passes by. In elastic soft tissues, the temporary cavity can be much larger than the permanent cavity. The quantity of damaged tissue is difficult to estimate. Mature bone, however, is capable of minimal elastic deformation before failure, and therefore bone in the region of the temporary cavity is usually fractured if the shock wave produced by the passing bullet is sufficient. The tendency for progressive necrosis to develop in the zone of tissue injury is difficult to predict, and this has significant implications for management.
- •
Fragmentation , if it occurs, enlarges the volume of injured tissue. Fragmentation is significantly increased if the projectile strikes hard or inflexible tissues such as bone.
Diagnostic Studies
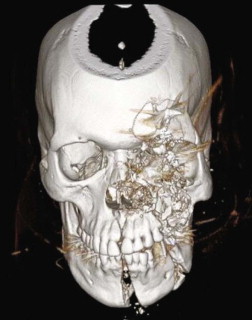
A craniofacial protocol computed tomography (CT) scan with 1-mm cuts in the axial, sagittal, and coronal planes with three-dimensional remodeling is the diagnostic study of choice and can provide detailed information on both the soft and hard tissue extent of injury ( Fig. 45-1 ). Furthermore, CT can be used to evaluate for possible concomitant cervical spine or vascular injuries. Plain films, such as the panoramic tomogram, are useful in relating the injuries to the occlusion. However, they are often plagued by superimposition artifact and poor clarity in the central region of the face/symphysis.
In addition, high-quality digital photographs of the face in the frontal, oblique, and side views with documentation of the site and extent of injury, as well as pre-injury photographs, are important to assist in the reconstructive effort.
Reconstructive Goals
The current philosophy of initial treatment is (1) serial inspection and débridement, (2) early reduction and fixation of bone, and (3) early definitive reconstruction, which may require recruitment of hard or soft tissue. Secondary revisions may be performed at a later stage if needed. This approach simplifies the procedures, reduces operating time, and lowers associated morbidity.
Specific Treatment and Techniques
Emergency Management and Triage
Initial management of any ballistic wound should follow the advanced trauma life support protocol. The airway should be addressed first and can be problematic to identify and secure. Normal anatomic landmarks can be distorted by edema, local tissue collapse because of loss of supporting bone, and hemorrhage. The best technique for airway management will depend on any concomitant cervical spine injury, the general condition of the patient, and the specifics of the maxillofacial injury. Orotracheal or nasotracheal intubation is always the preferred method of initial airway control, although nasal intubation should be avoided in patients with severe bleeding. Even though elective tracheostomy is often required in these patients, cricothyroidotomy is the most reliable surgical airway in the emergency setting, with future conversion to a formal tracheostomy in a controlled setting.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


