Introduction
Maxillary impaction and bimaxillary osteotomies are used to treat anterior open-bite malocclusions but can have adverse soft-tissue effects. Correcting an anterior open bite with a single mandibular procedure avoids these undesirable soft-tissue effects, but the stability of this procedure is unknown. The purpose of this study was to assess the long-term stability of anterior open-bite correction with bilateral sagittal split osteotomy and rigid internal fixation.
Methods
Orthognathic surgical records of 1 oral surgeon were searched for all patients treated for anterior open bite with bilateral sagittal split osteotomy and surgical closing rotation of the mandible with rigid internal fixation. Cephalometric films from initial consultation, presurgery, postsurgery, orthodontic appliance removal, and a mean of 4.5 years after orthodontic appliance removal were collected, traced, and measured.
Results
Thirty-one patients fit the inclusion criteria for this study and had an initial mean open bite of –2.6 mm (SD, 1.1 mm). The patients experienced an average mandibular closing rotation of 3.7° (SD, 2.4°) with surgery. By orthodontic appliance removal, the mandible rotated open 1.1°, and incisor overlap was 1.4 mm (SD, 1.0 mm). Approximately 4.5 years after orthodontic appliance removal, the mean incisor overlap was maintained at 1.0 mm (SD, 1.0 mm), yet the mandible rotated open an additional 1.1°. Only 3 patients relapsed to no incisor overlap in the long term, and only 3 patients experienced relapse greater than 1 mm in the long term.
Conclusions
Approximately 90% of the treated patients had a positive incisor overlap 4.5 years after orthodontic appliance removal. Despite a 60% loss of mandibular surgical closing rotation, only 10% of the patients relapsed to no incisor overlap in the long term. Bilateral sagittal split osteotomy and surgical closing rotation of the mandible by using rigid internal fixation should be considered a stable alternative in the treatment of mild-to-moderate anterior open-bite malocclusions.
Anterior open bite is a term used to describe instances when the maxillary and mandibular incisors fail to overlap or contact with each other, resulting in significant esthetic and functional difficulties. When open bites have skeletal components, as in many nongrowing patients, they are often associated with greater vertical facial relationships and are not self-correcting. The correction of such a vertical discrepancy can be difficult and often necessitates surgery.
Historically, a bilateral sagittal split osteotomy with closing rotation of the mandible using intermaxillary wire fixation was used to treat patients with anterior open bite and had a significant rate of relapse. Factors that contributed to relapse included improper condylar seating, unstable fixation, magnitude of advancement, pterygoid muscle and connective or soft-tissue pull, and postoperative muscle strength and length changes.
The focus then shifted to maxillary impaction surgery for the correction of anterior open bite. However, the adverse soft-tissue effects of this surgery made this option less desirable for some patients. These effects include increased alar cartilage width, an upturned nose with increased nares exposure, flattening of the upper lip, thinning of the vermilion, an obtuse nasolabial angle, and excessive gingival display. The use of dual jaw surgery has attempted to ameliorate these soft-tissue effects, yet patients can still suffer from undesirable esthetic results.
With the advent of rigid internal fixation, improved stability in mandibular surgical procedures has been documented. Now used in most orthognathic surgical corrections, rigid internal fixation has allowed the revisitation of mandibular correction to treat mild-to-moderate anterior open bite and has achieved favorable clinical results. This procedure has a reduced risk of negative soft-tissue effects and the added benefit of simultaneous vertical anterior open-bite correction and anteroposterior correction with 1 mandibular procedure. Despite these advantages, the long-term stability of this procedure has yet to be determined.
The purposes of this retrospective study were to evaluate the long-term stability of anterior open-bite correction with orthodontic treatement and bilateral sagittal split osteotomy, and to describe the long-term dental and skeletal changes during and after this procedure, once the orthodontic fixed appliances were removed.
Material and methods
Institutional review board approval for the use of human subjects was obtained from the University of Washington in Seattle. The electronic health records and surgical calendars of 1 oral surgeon (D.S.B.) from 1988 to 2009 were searched for all patients with anterior open bite who were consecutively treated (independent of outcome) with orthodontics and bilateral sagittal split osteotomy with surgical closing rotation of the mandible using rigid internal fixation only. Patients who received any form of surgery involving the maxilla to correct the anterior open bite during this time frame were excluded from the study. Once patients were identified, an attempt was made to collect cephalometric films from the oral surgeon or the treating orthodontist.
The inclusion criteria were (1) cephalometric films available from 5 time periods—initial (T1), presurgery (T2), postsurgery (T3), debond (T4), and long term (T5, >1 year after the braces were removed); (2) no overlap of the incisors, as measured by the distance between the maxillary and mandibular incisal edges parallel to the maxillary occlusal plane at T1; and (3) composite tracing of T2 onto T3 demonstrated the bilateral sagittal split osteotomy with closing rotation of the mandible by using rigid internal fixation (with or without accompanying midline osteotomy or genioplasty at the surgery). The exclusion criteria were (1) incomplete, illegible, or nondiagnostic radiographs; (2) any maxillary surgery; (3) jaw surgery before or after the bilateral sagittal split osteotomy of interest; and (4) pretreatment facial trauma, facial surgery, or any syndrome affecting the face.
On each film, all patient identity information was replaced with study identification numbers. Randomization of films was not possible for the T1, T2, and T3 films because of the malocclusion, appliances, and hardware present. The films at T4 and T5 were randomized by another person so that the researcher tracing the films (A.M.F.) would be blinded.
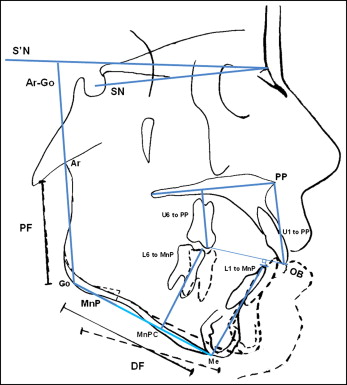
The same author (A.M.F.) both hand-traced conventional films and was responsible for identifying all landmarks. A template from the T2 film was created to aid in landmark identification. When digital films were available, they were printed and also hand-traced for consistency. The orthodontic landmarks and reference lines used to create the descriptive linear and angular measurements of interest are shown in Figure 1 . To better visualize changes occurring in the mandible, the following indirect reference lines were created.
- 1.
S′N: surrogate Frankfort plane made by adding a correction factor of 7° to the sella-nasion line.
- 2.
Constructed mandibular plane (MnPC): the portion of the mandibular plane that represents the distal segment of the mandible after surgery.
- 3.
Proximal segment fiducial: a line drawn 10 mm perpendicular and posterior to the Ar-Go line, representing the proximal fragment of the mandible.
- 4.
Distal segment fiducial: a line drawn 10 mm perpendicular and inferior to the MnPC and used to visually verify that closing rotation has occurred.
The hand-tracings were also used to create an overall superimposition by using the best fit of the cranial base, a maxillary superimposition by using the anatomy of the hard palate, and a distal fragment superimposition by using the symphyseal anatomy of the mandible. When a genioplasty or a midline osteotomy might have altered the symphyseal region, screws placed during surgery were used as superimposition aids. These superimpositions were created for each time period of interest.
All hand-tracings were scanned with a scanner (Expression 1680; Epson, Long Beach, Calif) at 200 dpi and captured into imaging software (version 11.0; Dolphin, Chatsworth, Calif) for measurement. All linear measurements were corrected for magnification. Cephalometric films with a ruler or a magnification scale were adjusted accordingly. For films without rulers, magnification was adjusted by using the millimetric length of the sella-nasion line, since the cranial base is considered relatively stable beyond 7 years of age.
Statistical analysis
Data collection and statistical analysis were completed by using Excel (Microsoft, Redmond, Wash) and the Statistical Package for Social Sciences (version 15; SPSS, Chicago, Ill). To test for significance between overbite and the constructed mandibular plane angle measurements after surgery, a repeated-measures analysis of variance (ANOVA) was performed (α = 0.05). When significant, post-hoc tests with the Bonferroni correction were used to assess where the differences occurred (α = 0.05).
Errors caused by landmark identification, tracing, digitization, and measurement were assessed with Dahlberg’s formula by randomly choosing 5 patients (25 films) for repeated linear overbite and angular S′N-MnPC measurements. The method errors were calculated as 0.23 mm for overbite and 0.41° for S′N-MnPC; both were considered acceptable.
Results
Ninety-eight patients were identified in the surgical records and treated for anterior open bite with bilateral sagittal split osteotomy and rigid internal fixation. Thirty-one patients fit the inclusion criteria for the study, with most patients excluded for lack of cephalometric films, most notably the long-term film. Table I outlines the initial sample characteristics. The mean open bite at T1 (–2.6 ± 1.1 mm) represented about a 5-mm deviation when compared with a clinically normal positive incisor overlap of approximately 2.5 mm. The average mandibular plane angle relative to S′N (47.6° ± 5.5°) was increased by several degrees compared with the general population’s average. There were 14 patients with Angle Class I malocclusion, 15 patients with Class II malocclusion, and 2 patients with Class III malocclusion. The Class III patients were included in the analysis because their removal made no statistical difference in the results. The long-term follow-up period ranged from 1 year to 10.1 years, with a mean follow-up of 4.5 years after orthodontic treatment. The average time from the end of surgery to the removal of the orthodontic appliances was 10.6 months.
| Sex | 26 women 5 men |
|---|---|
| Mean age at T1 (y) | 26.9 ± 8.2 |
| Mean open bite at T1 (mm) | −2.6 ± 1.1 |
| Mean S′N to MnP at T1 (°) | 47.6 ± 5.5 |
| Mean surgical closing rotation (°) | 3.7 ± 2.4 |
| Angle classification | 14 Class I 15 Class II 2 Class III |
| Mean time from T4 to T5 (y) | 4.5 ± 2.6 years |
| Midline osteotomy | 13 patients |
| Genioplasty | 7 patients |
| Mandibular bonded retention | 23 patients |
Table II gives the mean cephalometric measurements at T1 along with standard normal measurement values for white subjects. The greatest deviations of this surgical population from standard normal values as determined by the investigator (A.M.F.) are shown. They include an increased ANB, a decreased SNB, an increased MnP angle, an increased SN-Ar-Go, a decreased U1-L1 angle, a negative overbite, an increased overjet, a divergent PP-MnP, and an increased lower anterior facial height. These multiple observations were not tested statistically for significant deviations from normal values.
| Measurement | Mean | SD | Normal | Maximum | Minimum |
|---|---|---|---|---|---|
| ANB (°) ∗ | 4.3 | 2.2 | 2 | 8.5 | −1.3 |
| SNA (°) | 80.2 | 3.8 | 82 | 86.8 | 70.4 |
| S′NA (°) | 87.2 | 3.8 | 93.8 | 77.4 | |
| SNB (°) ∗ | 75.9 | 4.3 | 80 | 88.1 | 67.4 |
| S′NB (°) ∗ | 82.9 | 4.3 | 95.1 | 74.4 | |
| SN-MnP (°) ∗ | 40.6 | 5.5 | 32 | 53.1 | 30.5 |
| S′N-MnP (°) ∗ | 47.6 | 5.5 | 60.1 | 37.5 | |
| SN-Ar-Go (°) ∗ | 148.4 | 6.3 | 143 | 162.7 | 138.0 |
| S′N-Ar-Go (°) ∗ | 155.4 | 6.3 | 169.7 | 145 | |
| U1-PP (mm) | 31.5 | 3.0 | 28 | 39.0 | 24.4 |
| U6-PP (mm) | 25.6 | 2.5 | 23 | 31.5 | 20.3 |
| L1-MnP (mm) | 43.5 | 4.0 | 40 | 52.8 | 35.4 |
| L6-MnP (mm) | 32.7 | 3.7 | 31 | 42.9 | 26.2 |
| L1-MnP (°) | 92.9 | 8.3 | 95 | 107.5 | 76.5 |
| U1-SN (°) | 104.7 | 6.5 | 103 | 122.2 | 91.8 |
| U1-S′N (°) | 111.7 | 6.5 | 129.2 | 98.8 | |
| U1-PP (°) | 111.8 | 5.5 | 110 | 127.2 | 97.9 |
| U1-L1 (°) ∗ | 121.8 | 8.9 | 135 | 138.2 | 108.7 |
| OB (mm) ∗ | −2.5 | 1.1 | 2.5 | −0.8 | −5.0 |
| OJ (mm) ∗ | 4.7 | 3.3 | 2.5 | 9.8 | −4.5 |
| PP-MnP (°) ∗ | 33.5 | 4.4 | 25 | 42.1 | 23.1 |
| Ar-Go-Me (°) | 130.5 | 6.5 | 130 | 145.3 | 118.1 |
| N-Me (mm) | 131.9 | 9.0 | 128 | 154.8 | 117.3 |
| N-MxP (mm) | 55.1 | 4.3 | 55 | 65.1 | 48.7 |
| ANS-Me (mm) ∗ | 78.3 | 6.5 | 66 | 91.1 | 65.6 |
| Ar-Go (mm) | 47.7 | 5.5 | 57.5 | 36.3 |
All average cephalometric measurements from the 5 time points are reported in Table III . From T1 to T2, increases in U1-PP, L1-MnP, L6-MnP, N-Me, ANS-Me, and Ar-Go were observed. This suggests some extrusion of the maxillary and mandibular incisors and mandibular molars, as well as increases in anterior facial height, lower anterior facial height, and posterior facial height.
| T1 mean | T2 mean | T3 mean | T4 mean | T5 mean | |
|---|---|---|---|---|---|
| ANB (°) | 4.3 | 4.6 | 2.2 | 2.5 | 2.9 |
| SNA (°) | 80.2 | 80.5 | 80.3 | 80.4 | 79.9 |
| S′NA (°) | 87.2 | 87.5 | 87.3 | 87.4 | 86.9 |
| SNB (°) | 75.9 | 75.9 | 78.1 | 77.9 | 77.0 |
| S′NB (°) | 82.9 | 82.9 | 85.1 | 84.9 | 84.0 |
| S′N-MnPC (°) | 47.6 | 47.3 | 43.6 | 44.8 | 45.8 |
| SN-Ar-Go (°) | 148.4 | 148.1 | 147.1 | 146.7 | 147.7 |
| S′N-Ar-Go (°) | 155.4 | 155.1 | 154.1 | 153.7 | 154.7 |
| U1-PP (mm) | 31.5 | 32.2 | 32.6 | 33.1 | 32.8 |
| U6-PP (mm) | 25.6 | 26.1 | 26.1 | 25.8 | 26.1 |
| L1-MnPC (mm) | 43.5 | 44.4 | 44.0 | 43.8 | 43.9 |
| L6-MnPC (mm) | 32.7 | 33.7 | 32.5 | 32.1 | 32.2 |
| L1-MnPC (°) | 92.9 | 93.5 | 91.3 | 89.3 | 90.6 |
| U1-SN (°) | 104.7 | 105.1 | 104.4 | 104.9 | 102.2 |
| U1-S′N (°) | 111.7 | 112.1 | 111.4 | 111.9 | 109.2 |
| U1-PP (°) | 111.8 | 112.2 | 111.6 | 111.9 | 109.7 |
| U1-L1 (°) | 121.8 | 121.2 | 127.7 | 128.1 | 128.3 |
| OB (mm) | −2.6 | −2.5 | 0.6 | 1.4 | 1.0 |
| OJ (mm) | 4.7 | 4.6 | 2.6 | 2.9 | 2.7 |
| PP-MnPC (°) | 33.5 | 33.2 | 29.4 | 30.8 | 31.4 |
| Ar-Go-Me (°) | 130.5 | 130.5 | 127.3 | 129.1 | 128.9 |
| N-Me (mm) | 131.9 | 133.1 | 131.6 | 130.8 | 131.9 |
| N-MxP (mm) | 55.1 | 55.1 | 55.2 | 54.8 | 55.4 |
| ANS-Me (mm) | 78.3 | 79.6 | 77.2 | 76.8 | 77.5 |
| Ar-Go (mm) | 47.7 | 49.4 | 50.3 | 48.3 | 48.5 |
The average overbite and constructed mandibular plane angle measurements from all 5 time periods are reported in Tables IV and V , and a qualitative assessment of overbite is presented in Table VI . Patients began with an average open bite of –2.6 mm and a constructed mandibular plane angle of 47.6°. At T2, there was minimal, if any, change in average open bite and constructed mandibular plane angle. However, on closer examination of these patients, it was observed that most experienced a slight improvement in open bite and a slight increase in constructed mandibular plane angle.
| Mean | SD | Maximum | Minimum | |
|---|---|---|---|---|
| T1 | 47.6 | 5.5 | 60.1 | 37.5 |
| T2 | 47.3 | 5.8 | 60.2 | 38.7 |
| T3 | 43.6 | 5.5 | 53.5 | 32.6 |
| T4 | 44.8 | 5.4 | 59.0 | 35.2 |
| T5 | 45.8 | 5.6 | 58.9 | 31.6 |
| Mean | SD | Maximum | Minimum | |
|---|---|---|---|---|
| T1 | −2.6 | 1.1 | −0.8 | −5.0 |
| T2 | −2.5 | 1.4 | 0.1 | −5.0 |
| T3 | 0.6 | 1.0 | 3.2 | −1.2 |
| T4 | 1.4 | 1.0 | 3.9 | −0.7 |
| T5 | 1 | 1.0 | 3.7 | −1.0 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


