Introduction
The objective of this investigation was to examine the factors influencing the long-term prognosis of autotransplanted teeth with complete root formation.
Methods
Thirty-eight teeth, autotransplanted in 32 patients, were examined more than 6 years after transplantation. Periodontal health, condition of restoration, mobility, occlusal contact, level of gingival margin, and course of orthodontic movement were investigated clinically and with radiographs.
Results
More than 6 years after autotransplanation, 33 teeth survived in 27 patients. The survival rate was 86.8% (mean observation time, 9.2 years). Abnormal findings were observed in 9 teeth, so the success rate was 63.1%. An inadequate root filling tended to give rise to abnormal findings.
Conclusions
The success of autotransplantation of a tooth with complete root formation is affected by the quality of root filling. When possible, clinicians should consider autotransplantation before root formation is complete.
Previous studies on tooth autotransplantion have mainly been reported from Scandinavia. Slagsvold and Bjercke reported a survival rate of 100% with little shortening of the root on autotransplanted teeth with incomplete root formation. Czochrowska et al found a survival rate of 90% with good long-term stability, over a mean observation period of 26.4 years. Andreasen et al reported that the survival rate of autotransplanted teeth with imcomplete root formation was over 95% after long-term observations ranging from 1 to 13 years.
In contrast to Scandinavia, in Japan, we have generally performed autotransplantation after the completion of root formation. Autotransplantation is mainly indicated after 12 years of age, after root formation has been completed, together with endodontic treatment. Previous reports have demonstrated high survival rates of autotransplanted teeth with complete root formation over a mean observation period of 5 years. However, little information is available as to the long-term stability of autotransplanted teeth with complete root formation. In addition, since incomplete root formation is associated with lower rates of periodontal and pulpal healing, it is possible that the survival rate decreases as the observation period increases beyond 10 years. This study was therefore designed to determine the factors that affect the long-term prognosis of autotransplanted teeth with complete root formation.
Material and methods
We recalled 56 patients who had undergone autotransplantation of 67 teeth at least 6 years earlier. All patients had orthodontic treatment with an edgewise appliance at the orthodontic department of Niigata University Medical and Dental Hospital and tooth autotransplantation with complete root formation at the oral surgery department of our hospital in Niigata, Japan, from 1993 to 2000. Teeth diagnosed with ankylosis before the operation and teeth preserved frozen were excluded ( Fig 1 ).
The attendance rate was 57.1%, and the prognoses of 38 teeth in 32 patients were examined. Of those, 5 patients had already lost 1 transplanted tooth. In this study, therefore, 27 patients (17 women, 10 men) with 33 surviving autotransplanted teeth were examined. The mean age at the time of surgery was 24.1 years (female subjects, 25.8 years; range, 10.8-43.2 years; male subjects, 20.7 years; range, 14.0-33.7 years). The mean postoperative period was 9.2 years (range, 6.1-14.5 years) ( Fig 1 ). The donor teeth and recipient sites are shown in Table I .
| Donor teeth | Recipient site | |
|---|---|---|
| UI | 3 | 8 |
| UP | 10 | 3 |
| UM | 2 | 3 |
| LI | 2 | – |
| LP | 12 | 10 |
| LM | 4 | 19 |
For 31 teeth, transplantation was performed to compensate for agenesis, congenital missing teeth, or tooth absence due to decay and periodontitis. Two teeth were transplanted for surgical correction of transposition.
All transplantations were performed according to the procedure described by Andreasen et al. An important feature of this procedure includes the preservation of the periodontal membrane to the maximum extent, tight sutures, rests of transplanted teeth with sufficient clearance between opposite teeth, and so on. Root canal treatment and temporary root filling with calcium hydroxide of the transplanted teeth were done within 3 weeks after the operation. Postoperative fixation was carried out with composites, and wire splints were removed after 3 weeks.
The survival rate was calculated as the percentage of transplanted teeth that were still present at the examination relative to the total number of transplanted teeth. The success rate was represented as the percentage of transplanted teeth that showed no abnormal findings: no progressive root resorption, and normal hard and soft periodontal condition relative to the total number of transplanted teeth.
The assessments were conducted clinically by an author (Y.W.). The transplanted teeth were compared with the contralateral donor teeth as the control teeth. The radiographs were analyzed independently by 2 observers, an author and another dentist (T.M.). In case of disagreement, the observers discussed their observations to obtain consensus.
The plaque index (4 sites) was measured according to the method of Silness and Löe, and the gingival index (4 sites) was measured according to the method of Löe and Silness. The probing depth was recorded at 6 sites with a periodontal probe (CPITN-C, YDM, Tokyo, Japan).
Depending on the condition of restoration, the materials were categorized into the full-restoration group (FRG: crown or bridge) or the partial-restoration group (PRG: composite filling or inlay).
With radiography, replacement resorption (ankylosis) was defined as the disappearance of the periodontal space and root resorption without radiolucency in relation to the resorpton area. Inflammatory resorption was defined as resorption cavities on the root surface associated with similar resorption activity in the adjacent alveolar bone. Furcation or periapical lesions were recorded as abnormal findings. The quality of root filling was considered to be suitable when the root filling material appeared to end 2 mm or less from the radiographic apex, without a visible apical lumen. Root filling was inadequate under all other circumstances.
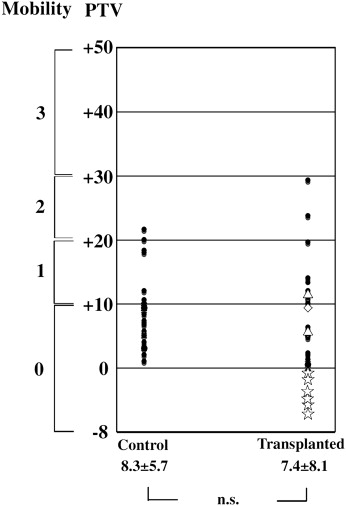
The mobility of the teeth was assessed by using Periotest (Gulden-Medizintechnki, Bensheim, Germany). The measurements were made 3 times, and the average values were used, after confirming the absence of significant differences among premeasurements made 3 times. The Periotest values (PTV) were converted into numeric scales ranging from –8 to +50. The PTV was correlated with Millar’s index as follows: –8 to +9, no noticeable movement (0); 10 to 19, first distinguishable sign of mobility (1); 20 to 29, deviation of the crown to within 1 mm of its normal position (2); and 30 to 50, easily noticeable mobility (3).
Study models were prepared to determine the presence or the absence of occlusal contacts and to measure the level of gingival margins. The level of the gingival margin was measured as the distance between the most apical point of the soft-tissue margin at the facial aspect of the crown and a line connecting the midfacial level of the soft-tissue margin of 2 adjacent teeth. Transplanted teeth located in the most distal position in the dental arch were excluded. The measurement was conducted with digital calipers (ABS Digimatic Caliper CD-20C, Mitutoyo, Tokyo, Japan) on study models.
Orthodontic movement was checked from the orthodontic treatment records.
Statistical analysis
The t test was used for statistical comparisons between the transplanted and control teeth for probing depth, PTV, and level of the gingival margin. The Wilcoxon signed rank test was performed for comparisons of the plaque index and the gingival index. The correlations between independent variables were determined by calculating Spearman correlation coefficients. Multiple regression analysis was used to determine the independent influence of variables on the prognosis of the transplanted teeth. All statistical analyses were performed with a statistical software package (JMP version 5.1.2, SAS Institute, Cary, NC). The significance level was set at P <0.05.
The study was approved by the ethical committee of the Faculty of Dentistry of Niigata University (approval number 102).
Results
The survival rate was 86.8%, because 5 teeth in 5 patients of the 38 teeth in 33 patients had been lost. Of those, 3 showed replacement resorption, 1 had inflammatory resorption, and 1 showed periodontal disease. The success rate was calculated to be 63.1%, since there were abnormal findings in 9 autotransplanted teeth including the 5 lost teeth, as mentioned above.
The plaque and gingival indexes tended to be higher in the transplanted teeth than in the control teeth. The transplanted teeth tended to show slightly increased pocket depths compared with the control teeth. On the status of restoration, 21 transplanted teeth were classified as FRG and 12 teeth as PRG. The results of the periodontal assessment were suspected to be influenced by the condition of restoration, because FRG accounted for about 60% of the materials between the 2 groups. The probing depth tended to be greater in the FRG group than that in the PRG group ( Table II ). In addition, the plaque and gingival indexes also tended to be higher in the FRG group than in the PRG group, but the difference was not significant.
| Site | FRG Mean ± SD | PRG Mean ± SD | Significance |
|---|---|---|---|
| BM | 2.5 ± 0.9 | 2.3 ± 0.8 | NS |
| BC | 2.1 ± 1.1 | 1.2 ± 0.5 | ∗ |
| BD | 2.5 ± 0.8 | 2.4 ± 0.8 | NS |
| LM | 2.5 ± 0.8 | 2.5 ± 0.9 | NS |
| LC | 2.2 ± 1.1 | 1.8 ± 0.5 | NS |
| LD | 2.4 ± 0.6 | 2.4 ± 0.6 | NS |
No evidence of pathology was detected in 24 of the transplanted teeth ( Fig 2 , A ). Six showed replacement resorption ( Fig 2 , B ), 1 had inflammatory resorption ( Fig 2 , C ), and 2 showed a furcation-periapical lesion ( Fig 2 , D ). The quality of root filling was considered to be adequate for 23 transplanted teeth ( Fig 2 , E ). However, the remaining 10 were inadequate because the root filling in these subjects was not homogeneous, and there was a visible space ( Fig 2 , F ). In the 10 transplanted teeth with inadequate root filling, 3 showed replacement resorption, 1 showed inflammatory resorption, and 2 showed a furcation-periapical lesion. In addition, the root filling was inadequate in 4 of the 5 transplanted lost teeth.
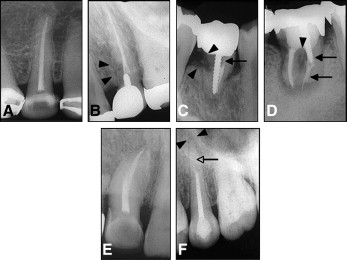
Tooth mobility (PTV) had a low tendency in the transplanted teeth compared with the control teeth, but the difference was not significant ( Fig 3 ). On the other hand, 6 of the transplanted teeth showed a negative PTV, which was considered to be attributable to the replacement resorption observed in the radiography ( Fig 2 , B ).
Five teeth showed infraocclusion; 3 had replacement resorption, 1 showed inflammatory resorption, and another 1 had no sign of pathology in the maxillary anterior region.
There was no significant difference between the transplanted and the control teeth in the level of gingival margin ( Table III ).
| Transplanted | Control | ||
|---|---|---|---|
| Site | Mean ± SD | Mean ± SD | Significance |
| BC | 0.5 ± 1.8 | 0.5 ± 1.1 | NS |
Orthodontic movement was undertaken for 32 teeth after a mean postoperative period of 5 months. This proved to be impossible in the treatment records for 5 transplanted teeth; this was attributed to the replacement resorption found by radiograph.
The quality of root filling, PTV, occlusal contact, and course of orthodontic movement were significantly associated with the success of transplant ( Table IV ).
| Successful transplant | Sex | Age | Years after procedure | Plaque index | Gingival index | Probing depth ≥4 mm | Restoration | Root filling | PTV | Occlusal contact | Orthodontic movement | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Successful transplant | 1 | |||||||||||
| Sex | −0.04 | 1 | ||||||||||
| Age | 0.13 | −0.38 ∗ | 1 | |||||||||
| Years after procedure | −0.18 | −0.15 | −0.40 ∗ | 1 | ||||||||
| Plaque index | 0.09 | 0.36 ∗ | −0.31 | 0.06 | 1 | |||||||
| Gingival index | 0.02 | 0.15 | −0.52 ∗ | 0.4 ∗ | 0.68 ∗ | 1 | ||||||
| Probing depth ≥4 mm | 0.18 | 0.18 | −0.22 | −0.22 | −0.04 | −0.14 | 1 | |||||
| Restoration | 0.18 | 0.05 | −0.10 | −0.09 | −0.02 | −0.16 | 0.24 | 1 | ||||
| Root filling | 0.69 ∗ | 0.11 | 0.05 | −0.04 | 0.19 | 0.11 | 0.18 | 0.18 | 1 | |||
| PTV | 0.50 ∗ | −0.08 | 0.20 | −0.18 | −0.07 | −0.11 | 0.01 | 0.20 | 0.33 | 1 | ||
| Occlusal contact | 0.35 ∗ | −0.30 | 0.13 | −0.05 | −0.15 | −0.08 | −0.09 | −0.22 | 0.18 | 0.14 | 1 | |
| Orthodontic movement | 0.51 ∗ | −0.30 | 0.04 | 0.14 | −0.15 | 0.06 | 0.09 | 0.08 | 0.18 | 0.35 ∗ | 0.27 | 1 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


