Within the last 30 years, the role of dental hygienists has expanded to include the administration of local anesthesia. Several studies have been performed to assess practice characteristics and effectiveness of these changes in state licensure regulations. Findings indicate an acceptance of this expansion in dental hygiene practice; however, the delegation of this pain control procedures remains controversial. To address this controversy, the authors have reviewed of current literature to assess the practice of local anesthesia administration by dental hygienists.
Within the last 30 years, many states have expanded the scope of practice for dental hygienists to include the administration of local anesthesia. Several studies have been performed to assess practice characteristics and effectiveness of these changes in state licensure regulations. Findings indicate an acceptance of this expansion in dental hygiene practice, with prominent rates of employer delegation of local anesthesia administration to dental hygienists, successful injection administration, and positive benefits to dental practice. Although these various outcomes support the use of this modality by dental hygienists, the delegation of these pain control procedures remains controversial. To address this controversy, the authors have reviewed of current literature to assess the practice of local anesthesia administration by dental hygienists.
Scope of practice
Regulations permitting the administration of local anesthesia by dental hygienist have been slowly implemented into the scope of dental hygiene practice since Washington approved regulations in 1971. As of the writing of this article, 42 US dental boards allow dental hygienists to deliver local anesthetic injections, and two additional states (Indiana and Maryland) have regulations pending for the implementation of this modality. New York and South Carolina are the only states in which dental hygienists are limited to local infiltration injections (Maryland’s proposed regulations will also limit use to infiltration injections). Texas, Mississippi, Alabama, Georgia, North Carolina, and Florida have not included a provision for the administration of local anesthesia injections within the scope of practice of dental hygienists.
As shown in Fig. 1 , most state dental boards require dental hygienists to administer local anesthesia under the direct supervision of a dentist. Under direct supervision, the dentist responsible for the procedure must be present in the dental office or facility, personally diagnose the condition to be treated, personally authorize the procedure and, before dismissal of the patient, personally examine the condition after treatment is completed. It does not require the dentist to be physically present in the operatory as the injection is being administered.
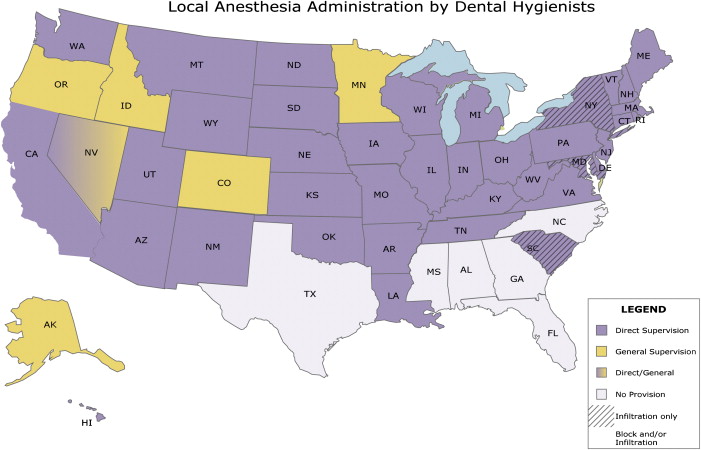
It should be noted, however, that within the jurisdictions of 6 dental boards (Alaska, Colorado, Idaho, Minnesota, Nevada, and Oregon), the dental hygienist is permitted to administer local anesthetics under general supervision. General supervision means that the dentist has authorized the procedures to be performed for a patient but does not require that a dentist is physically present within the office or facility when the procedures are performed.
In the 2007 Survey of Dental Hygienists in the United States, dental hygienists were asked not only to describe the clinical services provided at their worksites, but also to indicate the amount of time spent weekly providing each service and the level of required supervision for each task. An analysis of required supervision for specific dental hygiene clinical services revealed that there were differences across states in the supervision required for many of the tasks. Mean supervision scores were computed based on a scale in which direct supervision for a task was scored as 4, indirect supervision was scored as 3, general supervision was scored as 2, and no supervision was scored as 1. According to the survey, the mean national supervision scores for administration of local anesthesia (3.06) were among the highest for any dental hygiene service. The range in mean supervision scores for local anesthesia (2.0 to 4.0) was greater than for prophylaxis.
Education and training requirements
In the United States, professional licensure regulations establishing the policies of oral health personnel are the responsibility of individual state governments. Each state’s governing body operates with a specific board or committee that oversees dental professionals and the statutes that govern the dental profession. Of the 42 states that allow dental hygienists to administer local anesthesia, most require the successful completion of a state board-approved continuing education course or competency training via a Commission on Dental Accreditation (CODA)-recognized dental hygiene program. However, a significant variation exists between the individual state dental boards on specific education requirements and the prerequisite of examination before certification.
As is true with dental sedation/anesthesia guidelines, the largest variation with dental hygienists wishing to achieve local anesthesia permit status relates to the amount and type of instructional hours needed. Depending on which state is being referenced, the legal requirements for instruction hours for dental hygiene local anesthesia courses are usually described in one of three categories: the general total course hours needed, specific course hours established by a set amount of didactic and clinical hours, or no specific hourly requirement.
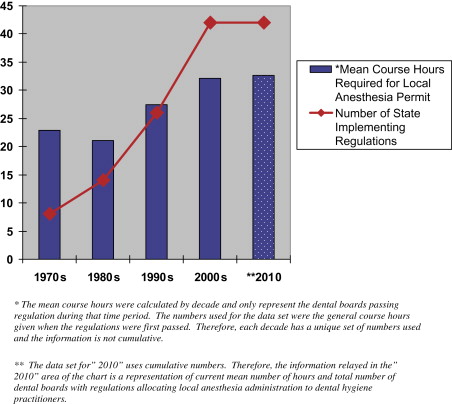
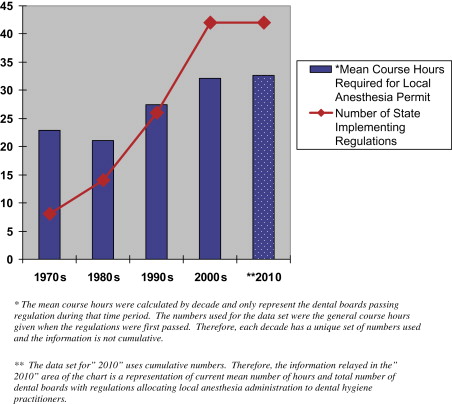
Twenty-eight states have general hourly requirements on local anesthesia instruction; 18 of those states specifically describe the amount of coursework to be dedicated didactically (mean = 15.4 hours) and clinically (mean = 11.5 hours). Currently, 14 states do not provide general instructional hour requirements in their regulation guidelines. However, all of these states require that the courses receive state board approval before granting permit status to students. As demonstrated in Fig. 2 , additional evaluation of the 28 states that have general instructional hour requirements reveals a mean of 32.7 total hours of instruction needed for permit status with the minimum number of hours of 12 (Kansas) and the maximum number of hours of 72 (Louisiana).
Twenty-seven of the 42 dental boards (63.4%) also require the successful completion of clinical or written examinations for certification. The type of examination varies between the individual dental boards. Fifteen dental boards require a board-approved examination given through the training course or accredited program; five dental boards only certify applicants through regional board examination (North East Regional Board [NERB] – 3 and Western Regional Examination Board [WREB] – 2). Two dental boards require both a regional board and state-approved examination, and four dental boards accept either regional board or state-approved examinations.
Education and training requirements
In the United States, professional licensure regulations establishing the policies of oral health personnel are the responsibility of individual state governments. Each state’s governing body operates with a specific board or committee that oversees dental professionals and the statutes that govern the dental profession. Of the 42 states that allow dental hygienists to administer local anesthesia, most require the successful completion of a state board-approved continuing education course or competency training via a Commission on Dental Accreditation (CODA)-recognized dental hygiene program. However, a significant variation exists between the individual state dental boards on specific education requirements and the prerequisite of examination before certification.
As is true with dental sedation/anesthesia guidelines, the largest variation with dental hygienists wishing to achieve local anesthesia permit status relates to the amount and type of instructional hours needed. Depending on which state is being referenced, the legal requirements for instruction hours for dental hygiene local anesthesia courses are usually described in one of three categories: the general total course hours needed, specific course hours established by a set amount of didactic and clinical hours, or no specific hourly requirement.
Twenty-eight states have general hourly requirements on local anesthesia instruction; 18 of those states specifically describe the amount of coursework to be dedicated didactically (mean = 15.4 hours) and clinically (mean = 11.5 hours). Currently, 14 states do not provide general instructional hour requirements in their regulation guidelines. However, all of these states require that the courses receive state board approval before granting permit status to students. As demonstrated in Fig. 2 , additional evaluation of the 28 states that have general instructional hour requirements reveals a mean of 32.7 total hours of instruction needed for permit status with the minimum number of hours of 12 (Kansas) and the maximum number of hours of 72 (Louisiana).
Twenty-seven of the 42 dental boards (63.4%) also require the successful completion of clinical or written examinations for certification. The type of examination varies between the individual dental boards. Fifteen dental boards require a board-approved examination given through the training course or accredited program; five dental boards only certify applicants through regional board examination (North East Regional Board [NERB] – 3 and Western Regional Examination Board [WREB] – 2). Two dental boards require both a regional board and state-approved examination, and four dental boards accept either regional board or state-approved examinations.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


