Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Explain why apprehension and anxiety, fatigue, and tissue inflammation create difficulties in obtaining profound anesthesia.
- 2.
Define the pain threshold and the factors affecting it.
- 3.
Describe patient management techniques that facilitate obtaining adequate anesthesia.
- 4.
List techniques that are helpful in reducing the pain of injections.
- 5.
Describe the “routine” approach to conventional local anesthesia: when and how to anesthetize.
- 6.
Describe circumstances that create difficulties in obtaining profound anesthesia using conventional techniques.
- 7.
Describe when to use supplemental methods of obtaining pulpal anesthesia if standard block or infiltration methods fail.
- 8.
Review techniques of infiltration intraosseous, periodontal ligament, and intrapulpal injections.
- 9.
Discuss how to obtain anesthesia for specific pulpal and periapical pathoses: symptomatic irreversible pulpitis, symptomatic teeth with pulpal necrosis, asymptomatic teeth with pulpal necrosis, and surgical procedures.
When a tooth which is loose or painful is to be extracted, the nose of the patient should be rubbed with brown sugar, ivy and green oil; he is advised to hold his breath, a stone is then placed between his teeth, and he is made to close his mouth. The fluid which causes the pain is then seen to flow from the mouth in such quantity as frequently to fill three pots; after having cleansed the nose with pure oil, rinsed the mouth with wine, the tooth is no longer painful, and may easily be extracted. Scribonius, AD 47
This quotation sets forth Scribonius’ method of obtaining “anesthesia” almost 2,000 years ago. He was convinced that he could perform painless extractions using what was apparently a rather crude technique of pressure anesthesia. Even in modern times, this concern remains for dentists—how can they attain adequate levels of anesthesia to keep their patients relatively comfortable during endodontic procedures? Obtaining profound anesthesia for the endodontic patient is difficult and challenging. Many patients recount vivid (and often valid) accounts of painful experiences. Although routine anesthetic techniques are usually effective for restorative dentistry, endodontic procedures present special situations that require additional techniques and special approaches.
Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Explain why apprehension and anxiety, fatigue, and tissue inflammation create difficulties in obtaining profound anesthesia.
- 2.
Define the pain threshold and the factors affecting it.
- 3.
Describe patient management techniques that facilitate obtaining adequate anesthesia.
- 4.
List techniques that are helpful in reducing the pain of injections.
- 5.
Describe the “routine” approach to conventional local anesthesia: when and how to anesthetize.
- 6.
Describe circumstances that create difficulties in obtaining profound anesthesia using conventional techniques.
- 7.
Describe when to use supplemental methods of obtaining pulpal anesthesia if standard block or infiltration methods fail.
- 8.
Review techniques of infiltration intraosseous, periodontal ligament, and intrapulpal injections.
- 9.
Discuss how to obtain anesthesia for specific pulpal and periapical pathoses: symptomatic irreversible pulpitis, symptomatic teeth with pulpal necrosis, asymptomatic teeth with pulpal necrosis, and surgical procedures.
When a tooth which is loose or painful is to be extracted, the nose of the patient should be rubbed with brown sugar, ivy and green oil; he is advised to hold his breath, a stone is then placed between his teeth, and he is made to close his mouth. The fluid which causes the pain is then seen to flow from the mouth in such quantity as frequently to fill three pots; after having cleansed the nose with pure oil, rinsed the mouth with wine, the tooth is no longer painful, and may easily be extracted. Scribonius, AD 47
This quotation sets forth Scribonius’ method of obtaining “anesthesia” almost 2,000 years ago. He was convinced that he could perform painless extractions using what was apparently a rather crude technique of pressure anesthesia. Even in modern times, this concern remains for dentists—how can they attain adequate levels of anesthesia to keep their patients relatively comfortable during endodontic procedures? Obtaining profound anesthesia for the endodontic patient is difficult and challenging. Many patients recount vivid (and often valid) accounts of painful experiences. Although routine anesthetic techniques are usually effective for restorative dentistry, endodontic procedures present special situations that require additional techniques and special approaches.
Factors Affecting Endodontic Anesthesia
Emotional considerations, in addition to tissue changes, impair the effectiveness of local anesthesia. A patient who is psychologically distraught and has an inflamed pulp or periapex has a lower pain threshold (i.e., less stimulus is required to produce pain). In addition, the trigeminal nerve, which supplies primary sensory innervation to oral structures, is a complex entity. Knowledge of its more common anatomic features aids the clinician in successfully obtaining anesthesia.
Apprehension and Anxiety
Many endodontic patients have heard horror stories about root canal treatment. The cause may not be the treatment but the experience of a painful or “infected” tooth. They vividly recall the pain, swelling, and sleepless nights associated with the tooth before treatment. The procedure itself is generally less threatening; a survey of endodontic patients completing therapy indicated that 96% would agree to have future root canal treatment. Therefore, because they fear the unknown and have heard unfavorable stories, patients are apprehensive or anxious. This emotion plays a role in their perceptions and also affects how they react to pain. Many patients can effectively mask this apprehension!
Fatigue
Over a course of days, many patients with a toothache have not slept well, not eaten properly, or otherwise have not functioned normally. In addition, many are apprehensive or anxious about the appointment. The end result is a patient with a decreased ability to manage stress and less tolerance for pain.
Tissue Inflammation
Inflamed tissues have a lower threshold of pain perception ; this is called the allodynia phenomenon. In other words, a tissue that is inflamed is much more sensitive and reactive to a mild stimulus. Therefore, an inflamed tissue responds painfully to a stimulus that otherwise would be unnoticed or perceived only mildly. Because root canal treatment procedures generally involve inflamed pulpal or periradicular tissues, this phenomenon has obvious importance. A related complication is that inflamed tissues are more difficult to anesthetize.
A good example of the phenomenon of increased sensitivity is sunburn. Exposed tissues that have been sunburned are irritated and inflamed. The skin has now become quite sensitive (lower pain threshold) to contact and is painful. This same principle applies to inflamed pulpal and periapical tissues.
Previous Unsuccessful Anesthesia
Unfortunately, profound pulpal anesthesia is not always obtained with conventional techniques. Previous difficulty with teeth becoming anesthetized is associated with a likelihood of subsequent unsuccessful anesthesia. These patients are likely to be apprehensive (lower pain threshold) and generally identify themselves by comments such as, “Novocain never seems to work very well on me” or “A lot of shots are always necessary to deaden my teeth.” The practitioner should anticipate difficulties in obtaining anesthesia in such patients. Often, psychological management and supplemental local anesthesia techniques are required.
Initial Management
The early phase of treatment is most important. If the patient is managed properly and anesthetic techniques are performed smoothly, the pain threshold elevates. The result is more predictable anesthesia and a less apprehensive, more cooperative patient.
Psychological Approach
The psychological approach involves the four Cs: control, communication, concern, and confidence. Control is important and is achieved by obtaining and maintaining the upper hand. Communication is accomplished by listening to the patient and explaining what is to be done and what the patient should expect. Concern is shown by verbalizing awareness of the patient’s apprehensions. Confidence is expressed in body language and in a professional approach and communication style, giving the patient confidence in the management, diagnostic, and treatment skills of the dentist. Management of the four Cs effectively calms and reassures the patient, thereby raising the pain threshold.
Topics Related to Injection Pain
Obtaining the Patient’s Confidence
Obtaining the patient’s confidence is critical. Before any injection is given, establishing communication, exhibiting empathy, and informing patients of an awareness of their apprehension, in addition to their dental problem, markedly increases the patient’s confidence levels. Most important, having the patient’s confidence gives control of the situation to the dentist; this is a requisite!
Topical Anesthetic
Use of a topical anesthetic is popular as an adjunct to painless injections. Some investigators have shown topical anesthetics to be effective, whereas others have not. The most important aspect of using topical anesthesia is not primarily the actual decrease in mucosal sensitivity, but rather the demonstrated concern that everything possible is being done to prevent pain. Another aspect is the power of suggestion that the topical anesthetic will reduce the pain of injection. When a topical anesthetic gel is used, a small amount on a cotton-tipped applicator is placed on the dried mucosa for 1 to 2 minutes before the injection.
Solution Warming
A common belief is that an anesthetic solution warmed to or above body temperature is better tolerated and results in less pain during injection. Although some studies have shown that warming anesthetic solutions did not reduce the pain of injection, other studies have found that warming did reduce this pain. Further research is needed to determine whether warming anesthetic solutions is beneficial.
Needle Insertion
Initially, the needle is inserted gently into the mucosal tissue.
Small-Gauge Needles
A common misconception is that smaller needles cause less pain; this is not true for dental needles. Patients cannot differentiate between 25-, 27-, and 30-gauge needles during injections. These sizes have similar deflection patterns and resistance to breakage. However, to prevent broken needles when administering inferior alveolar nerve blocks, do not use 30-gauge needles, bury the needle to the hub, or bend needles at the hub. As a recommendation, a 27-gauge needle is suitable for most conventional dental injections.
Slow Injection
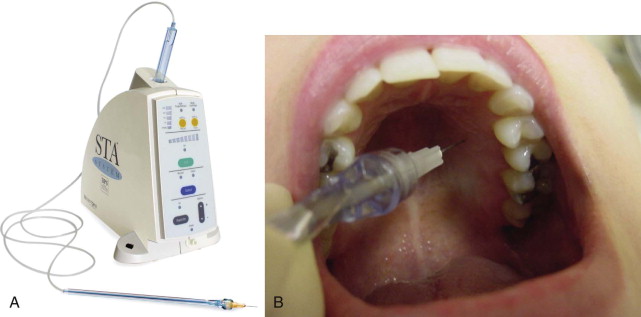
A slow injection decreases both pressure and the patient’s discomfort. A slow inferior alveolar nerve block is more comfortable than a rapid injection. A technique for slow injection is to use a computer-controlled anesthetic delivery system (CCLAD)( Fig. 9.1 ). Most studies on CCLADs compared the pain of injection with the delivery system to that with standard syringe injections, generally with favorable results. Therefore, although the CCLAD reduces the pain of the injection, the system does not produce a painless injection.
Two-Stage Injection
A two-stage injection consists of initial very slow administration of approximately a quarter-cartridge of anesthetic just under the mucosal surface. After regional numbness has been obtained, the remainder of the cartridge is deposited to the full depth at the target site. The two-stage injection decreases the pain of needle placement for females in the inferior alveolar nerve block. This injection technique is indicated for apprehensive and anxious patients or pediatric patients, but it may be used on anyone. It is also effective for any injection, including the inferior alveolar nerve block.
Gender Differences in Pain
Women try to avoid pain more than men, accept it less, and fear it more. Anxiety may also modulate differences in pain responses between males and females. Apparently, women react differently to pain than men do and are more likely to present anesthesia challenges.
When to Anesthetize
Preferably, anesthesia should be given at each appointment. There is a common belief that instruments may be used in canals with necrotic pulps and periapical lesions painlessly without anesthesia. Occasionally there may be vital tissue in the apical few millimeters of the canal. This inflamed tissue contains nerves and is sensitive. Not only is this vital tissue contacted during instrumentation, but also pressure is created. These factors may cause discomfort if the patient is not anesthetized.
There is an antiquated notion that canal length can be determined in a nonanesthetized patient by passing an instrument into a necrotic canal until the patient shows an “eye-blink response.” Unfortunately, patient perceptions and responses are too variable for accuracy. Pain may be felt when the instrument is far short of the apex, or some patients may have no sensation even when the instrument is several millimeters beyond the apex. Not using anesthesia to aid in length determination cannot replace radiographs or an electronic apex locator for accuracy. Another misconception is that after the canals have been cleaned and shaped, it is not necessary to anesthetize the patient at the obturation appointment. Unfortunately, during obturation, pressure is created and small amounts of sealer may be extruded beyond the apex. This may be quite uncomfortable for the patient. Many patients (and the dentist) are more at ease if regional hard and soft tissue anesthesia is present.
Adjunctive Pharmacologic Therapy
Anxious patients may benefit from sedation (oral, inhalation, intravenous). However, even with conscious sedation, profound local anesthesia is required to eliminate pain during dental treatment. Nitrous oxide administration helps reduce pain during treatment in patients presenting with symptomatic irreversible pulpitis. A discussion on agents that control anxiety is included in Chapter 10 .
Conventional Pulpal Anesthesia for Restorative Dentistry
Success of local anesthesia is variable. Two surveys of patients and dentists indicated that inadequate anesthesia was common during restorative treatment. Several factors affect anesthesia, such as the type of procedure (endodontic, extraction, restorative, periodontal, and so on), arch location (maxillary or mandibular), the patient’s anxiety level, and the presence of inflamed tissue. This chapter emphasizes the evidence-based requirements for pulpal anesthesia, which differ from those for oral surgery, implant dentistry, periodontics, and pediatric dentistry.
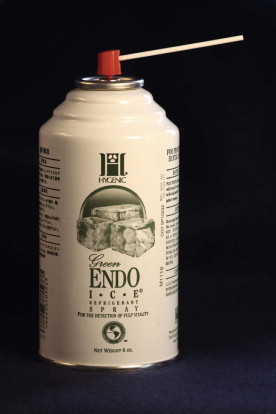
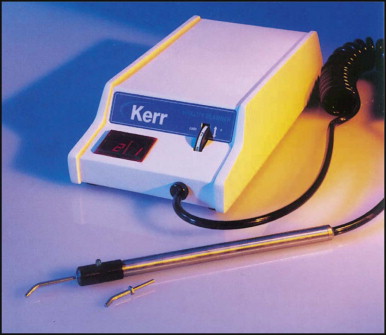
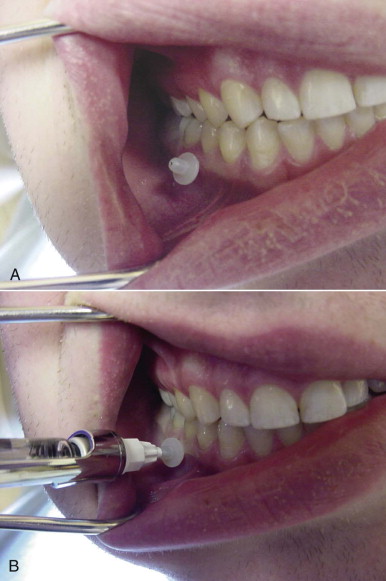
Many clinical studies have objectively evaluated local anesthetic agents and techniques. A measurement of pulpal anesthesia before beginning a clinical procedure is obtained with a cold spray refrigerant ( Fig. 9.2 ) or electric pulp tester ( Fig. 9.3 ). The cold spray refrigerant is the easiest to use clinically. The cold refrigerant is sprayed on a large cotton pellet held with cotton tweezers. The cold pellet is then placed on the tooth ( Fig. 9.4 ). No pulpal response to the stimuli after administration of anesthetic means probable profound pulpal anesthesia in asymptomatic teeth with vital pulps. Experimental studies that have investigated the use of local anesthesia are discussed in the following sections. Conventional injection techniques are detailed in other textbooks.

Mandibular Anesthesia for Restorative Dentistry
Lidocaine with Epinephrine and Vasoconstrictors
The most commonly used local anesthetic agent is 2% lidocaine with 1 : 100,000 epinephrine, which is a safe and effective drug. This agent is indicated for procedures in this chapter unless specified otherwise.
Vasoconstrictors are also generally safe. It has been stated that vasoconstrictors should be avoided in patients who have high blood pressure (higher than 200 mmHg systolic or 115 mmHg diastolic), cardiac dysrhythmias, severe cardiovascular disease, or unstable angina or who are less than 6 months past a myocardial infarction or cerebrovascular accident. These conditions are contraindications to routine dental treatment. Patients taking antidepressants, nonselective beta-blocking agents, medicine for Parkinson disease, and cocaine are at risk for problems. In patients taking these medications, plain mepivacaine (3% Carbocaine) can be used for the inferior alveolar nerve block.
Anesthetic Factors Associated with the Inferior Alveolar Nerve Block
Although the most common method of mandibular anesthesia is the inferior alveolar nerve block, this injection also has the greatest number of failures. The following sections discuss the expected signs of successful (and unsuccessful) anesthesia after administration of one cartridge of 2% lidocaine with 1 : 100,000 epinephrine.
Lip Numbness
Lip numbness usually occurs in 4 to 6 minutes after injection. Lip numbness indicates only that the injection blocked the nerves to the soft tissues of the lip, not necessarily that pulpal anesthesia has been obtained. If lip numbness is not obtained, the block has been “missed.” If this occurs frequently, the injection technique should be reviewed.
Soft Tissue Anesthesia
Lack of mucosal or gingival response to a sharp explorer does not indicate pulpal anesthesia.
Onset of Pulpal Anesthesia
Pulpal anesthesia usually occurs in 5 to 9 minutes in the molars and premolars and 14 to 19 minutes in the anterior teeth. In some patients, onset occurs sooner, and in others it is delayed.
Duration
The duration of pulpal anesthesia in the mandible is very good. Therefore, if successful, anesthesia usually (but not always) persists for approximately ![]() hours.
hours.
Success
The incidence of successful mandibular pulpal anesthesia tends to be higher in molars and premolars and lower in anterior teeth. Pulpal anesthesia is not achieved in all patients after what appears to be a clinically successful inferior alveolar nerve block (i.e., numb lip and chin). In such cases other approaches are required.
Alternative Attempts to Increase Anesthetic Success
Increasing the Volume
Increasing the volume of anesthetic from one to two cartridges does not increase the success rate for obtaining pulpal anesthesia with the inferior alveolar nerve block.
Increasing the Epinephrine Concentration
There is no improvement in pulpal anesthesia with a higher concentration (1 : 50,000) of epinephrine in an inferior alveolar nerve block.
Alternative Solutions
2% Mepivacaine with 1 : 20,000 Levonordefrin, 4% Prilocaine with 1 : 200,000 Epinephrine, and Plain Solutions (3% Mepivacaine and 4% Prilocaine)
As alternative solutions, 2% mepivacaine with 1 : 20,000 levonordefrin; 4% prilocaine with 1 : 200,000 epinephrine; and plain solutions (3% mepivacaine and 4% prilocaine) are equivalent to 2% lidocaine with 1 : 100,000 epinephrine in providing pulpal anesthesia for at approximately 1 hour after an inferior alveolar nerve block.
4% Articaine with Epinephrine for Inferior Alveolar Nerve Blocks
Articaine is a safe and effective local anesthetic agent. Articaine has a reputation for providing an improved local anesthetic effect. However, clinical trials have failed to detect any superiority of articaine over lidocaine in inferior alveolar nerve block anesthesia.
Articaine, like prilocaine, has the potential to cause neuropathies. Some authors have found the incidence of paresthesia (involving the lip and/or tongue) associated with articaine and prilocaine to be higher than that found with either lidocaine or mepivacaine. Other authors have not found a higher incidence when using articaine. However, because there is no difference in success of pulpal anesthesia between articaine and lidocaine for inferior alveolar nerve blocks, and some attorneys are aware of the proposed association of articaine to paresthesia, it seems reasonable to use articaine for infiltrations but not for nerve blocks.
Long-Acting Agents
Clinical trials of bupivacaine and etidocaine have been conducted in oral surgery, endodontics, and periodontics. These agents provide a prolonged analgesic period and are indicated when postoperative pain is anticipated. However, not all patients want prolonged lip numbness. For those patients, analgesics may be prescribed. Compared with lidocaine, bupivacaine has a somewhat slower onset but almost double the duration of pulpal anesthesia in the mandible (approximately 4 hours).
Buffered Lidocaine
Buffering lidocaine with sodium bicarbonate raises the pH of the anesthetic solution. In medicine there is evidence that buffering lidocaine results in less pain during the injection. In dentistry, some studies found that buffered lidocaine produced less pain on injection and a faster onset of anesthesia. However, other dental studies did not find less pain on injection or a faster onset with buffered lidocaine for inferior alveolar nerve block. There is a commercial buffering system available (OnPharma, Los Gatos, California), but there are no peer-reviewed studies on this system. Further studies are needed.
Alternative Injections and Locations
Gow-Gates and Vizarani-Akinosi Techniques
Neither the Gow-Gates nor the Vizarani-Akinosi technique is superior to the standard inferior alveolar nerve block injection. These techniques are not replacements for the inferior alveolar nerve block, but rather are useful when standard approaches cannot be used; for example, with trismus the Vizarani-Akinosi closed mouth technique can be used.
Incisive Nerve Block/Infiltration at the Mental Foramen
The incisive nerve block is successful 80% to 83% of the time in anesthetizing the premolar teeth for about 20 to 30 minutes. It is not effective for the central and lateral incisors.
Lidocaine Infiltration Injections
Labial or lingual infiltration injections of a lidocaine solution alone are not effective for pulpal anesthesia in the mandible.
Articaine Infiltration Injections
Articaine is significantly better than lidocaine for buccal infiltration of the mandibular first molar. However, articaine alone does not predictably provide pulpal anesthesia of the first molar. There is no difference between 4% articaine with 1 : 100,000 and 1 : 200,000 epinephrine for buccal infiltration.
In anterior teeth, buccal and lingual infiltrations of articaine provide initial pulpal anesthesia, but anesthesia declines over 60 minutes.
Evaluating Mechanisms of Failure with the Inferior Alveolar Nerve Block
Accuracy of Needle Placement
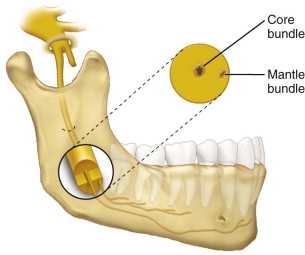
Accurate anatomic positioning of the needle is no guarantee of a successful block. Interestingly, even locating the inferior alveolar nerve with ultrasound or with a peripheral nerve stimulator before the injection did not improve success. The anesthetic solution may not completely diffuse into the nerve trunk ( Fig. 9.5 ) to reach and block all nerves, even if deposited at the correct site, thus resulting in failure.
Needle Deflection and Needle Bevel
Needle deflection has been theorized to be a cause of failure of the inferior alveolar nerve block. However, two studies have shown that needle bevel orientation (away or toward the mandibular foramen or ramus) does not affect the success of the inferior alveolar nerve block.
Accessory Innervation
Anatomic evidence suggests that accessory innervation exists from branches of the mylohyoid nerve. A study using a mylohyoid injection lingual and inferior to the retromolar fossa, in addition to an inferior alveolar nerve block, showed no enhancement of pulpal anesthesia. Therefore, the mylohyoid nerve is not a major factor in failure of the inferior alveolar nerve block.
Cross-Innervation
Cross-innervation from the contralateral inferior alveolar nerve has been implicated in failure to achieve anesthesia in anterior teeth after an inferior alveolar nerve block injection. Cross-innervation does occur in incisors but is not the major reason for failure in incisor teeth with the inferior alveolar nerve block.
Red Hair
In medicine, red-haired females have shown reduced subcutaneous efficacy of lidocaine and increased requirements for desflurane. However, in dentistry, red hair was unrelated to success rates for the inferior alveolar nerve block. Red hair was associated with higher levels of dental anxiety.
Methods to Increase Success of the Inferior Alveolar Nerve Block
Infiltrations of Articaine After an Inferior Alveolar Nerve Block
An important clinical finding is that an articaine infiltration of the first molar, premolars, and anterior teeth after an inferior alveolar nerve block should provide pulpal anesthesia for approximately 1 hour. The second molar may require a supplemental intraosseous or periodontal ligament injection to achieve success.
Intraosseous Anesthesia After an Inferior Alveolar Nerve Block
Supplemental intraosseous injections of lidocaine and mepivacaine with vasoconstrictors allow quick onset and increase the success of the inferior alveolar nerve block for approximately 60 minutes. Using 3% mepivacaine plain results in pulpal anesthesia for approximately 30 minutes.
Periodontal Ligament Anesthesia After an Inferior Alveolar Nerve Block
Supplemental periodontal ligament injections of 2% lidocaine with 1 : 100,000 epinephrine increase the success of the inferior alveolar nerve block, but the duration is approximately 23 minutes.
Injection Speed and Success
A slow inferior alveolar nerve block increases success over a fast injection but not for patients diagnosed with irreversible pulpitis.
Pain and Inflammation
Most studies have evaluated anesthesia in the absence of symptoms and inflammation; results differ if these conditions are present. As discussed later, patients who have symptomatic pulpal or periapical pathosis (and/or who are anxious) present significant anesthesia problems.
Maxillary Anesthesia for Restorative Dentistry
Unless otherwise specified, the conventional solution used is 2% lidocaine with 1 : 100,000 epinephrine.
Anesthesia-Related Factors
Anesthesia is more successful in the maxilla than in the mandible. The most common injection for the maxillary teeth is infiltration. Several events can be expected with this technique when one cartridge of anesthetic is used.
Lip/Cheek Numbness or Dead Feeling of the Teeth
Lip/cheek numbness usually occurs within a few minutes. Lip or cheek numbness or a dead feeling when tapping the teeth together does not always indicate pulpal anesthesia. Additionally, lip or cheek numbness does not correspond to the duration of pulpal anesthesia, because the pulp does not remain anesthetized as long as the soft tissues.
Success
Infiltration results in a fairly high incidence of successful pulpal anesthesia (around 87% to 92%). However, some patients may not be anesthetized due to individual variations in response to the drug administered, operator differences, and variations of anatomy, in addition to tooth position.
Onset of Pulpal Anesthesia
Pulpal anesthesia usually occurs in 3 to 5 minutes.
Duration of Pulpal Anesthesia
A problem with maxillary infiltration is the duration of pulpal anesthesia. Pulpal anesthesia of the anterior teeth declines after about 30 minutes, with most losing anesthesia by 60 minutes. In premolars and first molars, pulpal anesthesia is good until about 40 to 45 minutes and then it starts to decline. Additional local anesthetic must be administered, depending on the duration of the procedure and the tooth group affected.
Alternative Anesthetic Solutions
Plain Solutions of Mepivacaine and Prilocaine
Anesthesia duration is shorter with plain solutions of mepivacaine and prilocaine. Therefore, these anesthetics are used for procedures of short duration (10 to 15 minutes).
4% Prilocaine with 1 : 200,000 Epinephrine, 2% Mepivacaine with 1 : 20,000 Levonordefrin, and 4% Articaine with 1 : 100,000 Epinephrine
The duration of anesthesia with 4% prilocaine with 1 : 200,000 epinephrine; 2% mepivacaine with 1 : 20,000 levonordefrin; and 4% articaine with 1 : 100,000 epinephrine is similar to that for 2% lidocaine with 1 : 100,000 epinephrine.
Bupivacaine with Epinephrine
Bupivacaine has a lower success rate than a lidocaine formulation in anterior teeth. There is no difference in the first molar between the two formulations. Neither agent provides pulpal anesthesia for an hour.
Increasing the Duration of Pulpal Anesthesia
Increasing the Volume of Solution
A two-cartridge volume of 2% lidocaine with epinephrine extends the duration of pulpal anesthesia but not for 60 minutes.
Increasing the Epinephrine Concentration
Increasing the epinephrine concentration to 1 : 50,000 epinephrine increases duration for the lateral incisor but not for the first molar. Neither tooth achieved a duration of 60 minutes.
Repeating an Infiltration after 30 Minutes
Adding a cartridge of 2% lidocaine with epinephrine at 30 minutes in anterior teeth and 45 minutes in posterior teeth significantly improves the duration of pulpal anesthesia and may be the best way to extend the duration of pulpal anesthesia.
Alternative Injection Techniques
The posterior superior alveolar (PSA) nerve block anesthetizes the second molars and about 80% of first molars. An additional mesial infiltration injection may be necessary to anesthetize the first molar. Generally, the PSA block injection is not advocated for routine restorative procedures. An infiltration of the molars is preferred.
The infraorbital block results in lip numbness but does not predictably anesthetize incisor pulps. It usually anesthetizes the canines and premolars, but duration is less than 1 hour. Generally, the infraorbital injection is not advocated for routine restorative procedures. An infiltration of the individual teeth is preferred.
The second division block usually anesthetizes pulps of molars and some second premolars but does not predictably anesthetize first premolars, canines, or lateral and central incisors. The high tuberosity technique is preferred to the greater palatine approach, because it is easier and less painful. Generally, the second division nerve block is not advocated for routine restorative procedures. An infiltration of the individual teeth is preferred.
The palatal anterior superior alveolar (P-ASA) nerve block has been advocated for anesthetizing all the maxillary incisors with a single palatal injection into the incisive canal. However, this injection technique does not provide predictable pulpal anesthesia for the incisors and canines and is often painful.
The anterior middle superior alveolar (AMSA) nerve block has been advocated for unilaterally anesthetizing the maxillary central and lateral incisors, canines, and first and second premolars with a single palatal injection in the premolar region. However, this injection technique does not provide predictable pulpal anesthesia for these maxillary teeth and is often painful.
Pain, Inflammation, and Anxiety
As mentioned, results differ from normal when an anesthetic is given to patients with either pain or inflammation (or both) or to those with anxiety.
Supplemental Anesthesia for Restorative Dentistry in the Mandible and Maxilla
Indications
A supplemental injection is used if the standard injection is not effective. It is useful to repeat an initial injection only if the patient is not exhibiting the “classic” signs of soft tissue anesthesia. Generally, if the classic signs are present, reinjection is not very effective. For example, after the inferior alveolar nerve block, the patient develops lip, chin, and tongue numbness and quadrant “deadness” of the teeth. A useful procedure is to test the pulp of the tooth with cold (cold refrigerant) or an electric pulp tester before the cavity preparation is begun. If the patient feels pain to cold, a supplemental injection is indicated. Assuming that reinjection using the inferior alveolar nerve block approach will be successful is wishful thinking; failure the first time is usually followed by failure on the second attempt. The dentist should go directly to a supplemental technique. Three such injections are the (1) infiltration injection, (2) intraosseous (IO) injection, and (3) periodontal ligament (PDL) injection.
Infiltration
Additional Infiltration of Lidocaine in the Maxilla
Because the duration of pulpal anesthesia for infiltration in the maxilla is less than 60 minutes, adding a cartridge of 2% lidocaine with epinephrine at 30 minutes in the anterior teeth and at about 45 minutes in premolar and molar teeth significantly improves the duration of pulpal anesthesia and may be the best way to extend the duration of pulpal anesthesia in maxillary teeth.
Infiltration of Articaine in the Mandible
An important clinical finding is that a buccal articaine infiltration of the first molar and premolars and a labial infiltration of the anterior teeth, after an inferior alveolar nerve block, should provide pulpal anesthesia for approximately 1 hour. The second molar may require a supplemental intraosseous or periodontal ligament injection.
Intraosseous Anesthesia
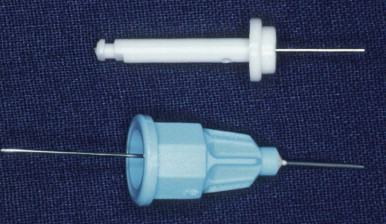
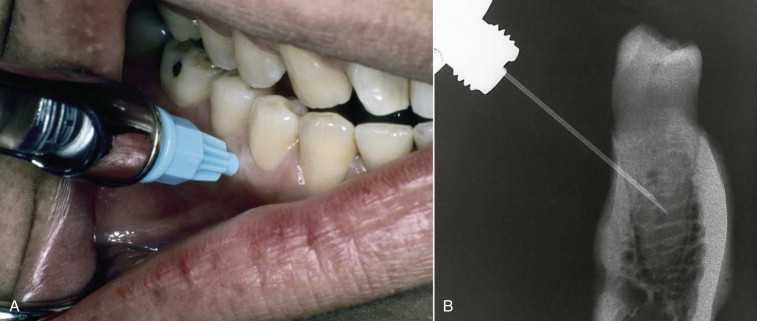
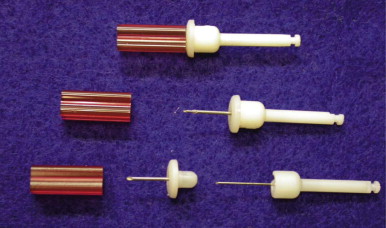
The IO injection has been shown to be effective by substantial research and clinical usage. It is particularly useful in conjunction with a conventional injection when it is likely that supplemental anesthesia will be necessary (e.g., in mandibular second molar teeth). The IO injection allows placement of a local anesthetic directly into the cancellous bone adjacent to the tooth. There is an IO system with two components (Stabident; Fairfax Dental, Miami, Florida; Fig. 9.6 ). One part is a slow-speed handpiece–driven perforator, which drills a small hole through the cortical plate ( Fig. 9.7 ). The anesthetic solution is delivered into cancellous bone through a matching 27-gauge, ultrashort injector needle ( Fig. 9.8 ). Another IO system uses a guide sleeve (X-tip; Dentsply, York, Pennsylvania; Fig. 9.9 ) that remains in the perforation ( Fig. 9.10 ). This serves as a guide for the needle, and it may remain in place throughout the procedure in case reinjection is necessary. The perforation may be made in attached gingiva or alveolar mucosa with this system.
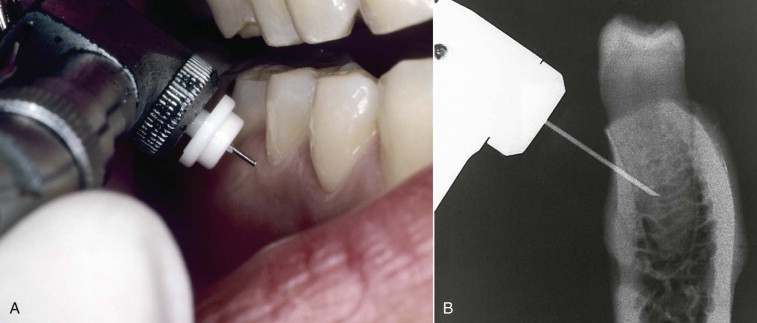
Technique for the Stabident System
The area of perforation and injection is on a horizontal line of the buccal gingival margins of the adjacent teeth and a vertical line that passes through the interdental papilla distal to the tooth to be injected. A point approximately 2 mm below the intersection of these lines is selected as the perforation site. This site must be in attached gingiva. The soft tissue is first anesthetized by infiltration. The perforator is placed through the gingiva perpendicular to the cortical plate. With the point gently resting against bone, the clinician activates the handpiece at full speed while pushing the perforator, with light pressure, against bone and then slightly withdrawing the perforator and pushing it again against the bone (pecking motion). This action is continued until a “break through” into the cancellous bone is achieved (this takes approximately 2 to 5 seconds).
The standard syringe is held in a “pen-gripping” fashion, and the needle is precisely aligned with and inserted into the perforation. A full cartridge of anesthetic solution is slowly delivered over 1 to 2 minutes with light pressure. If back-pressure is encountered, the needle is rotated approximately a quarter turn and deposition is reattempted. If this attempt is unsuccessful, the needle should be removed and checked for blockage. If the needle is not blocked, it is reinserted or the site is opened with a new perforator and the injection is repeated.
Perforator “Breakage”
Rarely, the metal perforator “separates” from the plastic hub. If this occurs, the perforator is easily removed with a hemostat; there are no reports of a perforator breaking into parts.
Injection Discomfort
When the IO injection is used as a primary injection, pain is experienced about one fourth of the time. When the IO injection is used as a supplemental injection, fewer patients experience pain.
Selection of Perforation Site
With IO injections, distal perforation and injection to the tooth result in the best anesthesia. The second molars are an exception; in these teeth, a mesial site is preferred.
Anesthetic Agents
When the IO injection is used as a supplemental injection after the inferior alveolar nerve block in patients without pain, excellent success has been reported for 2% lidocaine with 1 : 100,000 epinephrine and 2% mepivacaine with 1 : 20,000 levonordefrin. However, because of the adverse cardiovascular reactions with a long-acting anesthetic (0.5% bupivacaine with 1 : 200,000 epinephrine) and the lack of a prolonged duration of pulpal anesthesia, this agent does not offer any advantage over lidocaine. Three percent mepivacaine plain is successful, but the duration of pulpal anesthesia is shorter.
Onset of Anesthesia
Onset of anesthesia is rapid with the IO injection. There is no waiting period for anesthesia.
Success
When the IO injection is used as a supplemental injection after an inferior alveolar nerve block in pain-free patients, success rates are very good.
Failure
If the anesthetic solution squirts out of the perforation (backflow) with an IO injection, anesthesia will not be obtained. Reperforation or choosing another perforation site is then necessary.
Duration
With a primary IO injection, the duration of pulpal anesthesia declines steadily over 1 hour. There is an even shorter duration with 3% mepivacaine, compared with 2% lidocaine with 1 : 100,000 epinephrine. With a supplemental IO injection of lidocaine after the inferior alveolar nerve block in patients without pain, the duration of pulpal anesthesia is very good for 1 hour. A solution of 3% mepivacaine, when used as a supplemental IO injection, results in a shorter anesthetic duration.
Postoperative Pain and Problems
With primary and supplemental IO injection techniques, the majority of patients report no pain or mild pain postoperatively. Fewer than 5% develop exudate and/or localized swelling at the perforation site, possibly from overheating of the bone during perforation.
Systemic Effects
With both primary and supplemental IO injection techniques using anesthetics with a vasoconstrictor (epinephrine or levonordefrin), most patients perceive an increased heart rate. When these agents are used, the patient should be informed before the injection of this tachycardia to lessen his or her anxiety. No significant heart rate increase occurs with 3% mepivacaine plain. The venous plasma levels of lidocaine are the same for an IO injection as for infiltration injection. Therefore, the same precautions for the maximum amount of lidocaine given for an infiltration injection apply to an IO injection.
Medical Contraindications
Patients taking antidepressants, nonselective beta-blocking agents, medicine for Parkinson disease, and cocaine should not receive IO injections of solutions containing epinephrine or levonordefrin ; 3% mepivacaine plain is preferred.
Precautions
An IO injection should not be used with painful necrotic teeth with periapical radiolucencies or with teeth exhibiting cellulitis or abscess formation. This injection would be very painful and would likely not provide profound anesthesia.
Periodontal Ligament Injection
The PDL injection is also a useful technique if a conventional injection is unsuccessful. The technique is clinically less effective than the IO injection but still has its clinical place.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


