• Figure 9-1 Epulis reduction. A, Large epulis fissuratum consisting of elongated mass of flabby hyperplastic tissue in mucolabial fold. B, Complete bilateral excision of the hyperplastic tissue along a supraperiosteal plane with excellent hemostasis. C, At 1-week postoperative visit, a fibrous coagulum is present and functioning as a natural protective dressing during healing. D, At 3-month postoperative visit, complete healing is achieved, and the area of supraperiosteal dissection has granulated with attached keratinized tissue.
Vestibuloplasty
A common condition involves alveolar bone resorption with shallow vestibular depth, resulting in the patient’s inability to wear a denture with the desired comfort and function. Although traditionally this condition has been treated surgically using a scalpel, the CO2 laser is ideal in this situation for performing a bloodless supraperiosteal vestibuloplasty, with excellent results. Neckel20 treated 40 patients requiring vestibuloplasty with either traditional scalpel surgery or a laser procedure. Results showed equivocal gain in vestibular height between the two groups, but with less postoperative pain and discomfort in the laser group.
Beer and Beer21 performed CO2 laser maxillary vestibuloplasty in 10 patients in whom vestibular height ranged from 3 to 7 mm. A laser incision was performed from the second molar region of one side all the way to the second molar region of the contralateral side. After laser treatment, the patients’ old prostheses were adjusted with denture material to support the new vestibular heights. At the conclusion of the study, all of the vestibules were increased a minimum of 3 to 8 mm. Many of the patients showed increases of 10 to 12 mm, with no relapse. No complications were seen at follow-up evaluation 6 to 10 months postoperatively.
Laser Technique
Figure 9-2 illustrates a technique for laser vestibuloplasty in a patient requiring excision of an epulis and a vestibuloplasty. After administration of local anesthetic, the anterior vestibule is placed under tension by pulling the lower or upper lip outward. The laser is then used to create a supraperiosteal dissection.22 The tension maintained on the lip allows effortless establishment of an adequate plane of dissection. The tissue margin is then retained in place with sutures or a stent. If desired, an autogenous or allogeneic soft tissue graft can be used to cover the denuded area. Immobilization of the graft is key to its survival, which can be accomplished with suturing or placement of a stent.23
In patients not undergoing soft tissue grafting, postoperative discomfort is minimized and may be further reduced by initial continuous wear of a soft-relined denture or a tissue-conditioned denture, although this is not mandatory. In patients with significant resorption of the mandible, the genioglossus and mylohyoid muscle attachments often preclude adequate extension of the lingual flange of the denture.24 In such cases, a floor-of-mouth lowering procedure can be performed to increase lingual vestibular height. This operation can be done with a laser as previously described, again using supraperiosteal dissection and either sutures or a stent to fix the lowered tissue in place. At least half the musculature attached to the genial tubercles should remain, to ensure adequate functioning of the tongue and oropharyngeal muscles.
Tuberosity Reduction
During treatment planning for a full or partial upper denture, significant diagnostic criteria include the size and shape of the maxillary tuberosity. The tuberosity may be small and inconsequential in treatment planning. Alternatively, however, the tuberosity also may be large, flabby, and pendulous, with bilateral undercuts that would prevent fabrication of a properly fitting prosthesis. If the tuberosity is a concern, a radiographic series must be taken to evaluate the type of tissue; palpation alone will not necessarily provide the clinician with sufficient information to determine its consistency. The tuberosity may consist solely of hypertrophied soft tissue, requiring a surgical procedure to reduce the soft tissue, or it may consist of a thin layer of fibrotic tissue and mucosa overlying a thick, prominent mass of osseous tissue, requiring a hard tissue tuberosity reduction. Occasionally, the tuberosity may consist of a thin layer of fibrotic tissue and mucosa overlying a pneumatized sinus, and a sinus lift procedure may be performed (see Chapter 7).
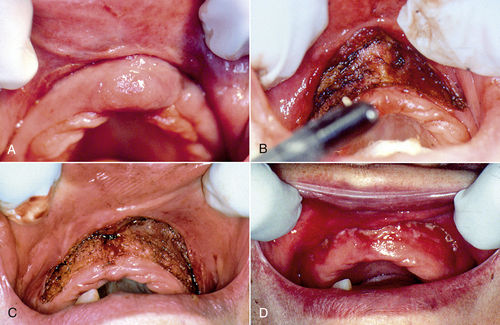
• Figure 9-2 Vestibuloplasty with epulis excision. A, Preoperative view of maxillary ridge epulis fissuratum. B, Epulis excision with a CO2 laser in continuous-wave mode. Note residual muscle on the periosteum. The laser is used to incise the muscle attachments, which subsequently migrate vertically. As the muscle is being dissected superiorly, tension is applied to the lip. C, Supraperiosteal dissection and vestibuloplasty completed. Note clean periosteum. D, Postoperative appearance at 10 days, with excellent vestibular depth and reepithelialization.
As summarized by Terry and Hillenbrand,25 soft tissue tuberosity reductions are performed to provide enough maxillomandibular clearance to allow sufficient space for the denture base and denture teeth. These investigators suggested a minimum of 5 mm of clearance between the tuberosity and the mandibular mucosa.
Costello et al.26 described the procedure for a soft tissue tuberosity reduction as follows:
1. An elliptical incision is performed over the tuberosity.
2. The mucosa is undermined.
3. The fibrous tissue is removed.
4. Excessive mucosal tissue is removed.
5. Primary closure is obtained.
If the tuberosity is primarily osseous tissue, once the elliptical incision is made, the mucoperiosteum is reflected and the bone removed with a rongeur or bur. The area must be smoothed with a bone file, irrigated, and closed. Care must be taken to avoid perforating into the maxillary sinus.26 Guernsey27 warned that during conventional techniques, care must be taken to avoid the greater palatine artery and its branches.
Laser Tuberosity Reduction
Each step just outlined may be performed using a dental laser. Pick28 stated that laser tuberosity reduction offers numerous advantages over conventional techniques. Common problems arise after the elliptical incision is made and the fibrous wedge of tissue removed, because the flaps of tissue need to be thinned and trimmed. The flaps often are trimmed more than once to achieve the correct size for primary closure. Occasionally, the flaps may be trimmed so that they are too short to achieve primary closure. This area is also difficult to suture.
When a laser is used for a soft tissue tuberosity reduction, the procedure is performed without an incision, so no suturing is needed. The soft tissue of the tuberosity is simply vaporized layer by layer until the correct maxillomandibular space has been achieved. This procedure may be performed both in patients currently wearing full dentures and in patients with treatment plans to receive a full or partial denture.
Convissar and Gharemani29 described a soft tissue tuberosity reduction in a patient before making a final impression for an immediate insertion of a full upper denture. By using a laser, the treatment period was shortened by at least 3 to 6 weeks because of the accelerated healing and less traumatic technique. The final impression for the immediate-insertion prosthesis was taken only 3 weeks after the tuberosity reduction, with confidence that no further tissue shrinkage would occur, resulting in a poor fit of the prosthesis. With no incision or sutures, healing occurred quickly and uneventfully. Accidental sinus perforation is avoided because the bloodless surgical site is clearly visualized, permitting ready distinction between mucosa and periosteum and decreasing the potential for this mishap. Because lasers cauterize and coagulate, inadvertently severing a palatine artery or one of its lesser branches also is less of a risk.
Pogrel30 described laser tuberosity reduction on four patients (average treatment time, 6 minutes). There were no reports of bleeding, swelling, or recurrence of the excess tissue. One patient underwent a bilateral tuberosity reduction: one side done with a conventional (scalpel) technique and the other with a laser; the laser-operated side felt more comfortable to the patient. The laser side healed before the scalpel side, and laser reduction took less time. Pogrel concluded that the advantages of the CO2 laser appear to be applicable to soft tissue preprosthetic surgery.
Soft Tissue
The procedure for a soft tissue laser tuberosity reduction is relatively simple and straightforward (Figure 9-3). After diagnostic radiographs are obtained to determine the location of the sinus floor and mounted study casts to determine the amount of surgical reduction necessary, a local anesthetic of choice is administered to the tuberosity both buccally and palatally. After selection of a large spot size/fiber or handpiece, the laser of choice is used at a surgical setting to ablate the tissue of the tuberosity layer by layer until sufficient maxillomandibular space is created. The laser tip should be kept as parallel as possible to the tuberosity, to ensure maximum efficiency. The laser beam is then moved out of focus to ensure adequate hemostasis. At this time the tissue is evaluated for irregularities or tissue tags; any such tissue is ablated with the laser. The denture may then be relined with a tissue conditioner or soft reline material. The patient receives postoperative instructions (maintaining clean surgical site, stressing oral hygiene), and a follow-up appointment is scheduled.
Hard Tissue
Many options are available for hard tissue laser tuberosity reduction, depending on the wavelengths available. If only a soft tissue wavelength—CO2, diode, or neodymium-doped yttrium-aluminum-garnet (Nd:YAG)—is available, an elliptical incision is made into the tuberosity with the laser, exposing the osseous structure. The osseous tissue is then reduced with the clinician’s instrument of choice, which may be a rongeur, a round bur with copious water spray in a high-speed handpiece, or a bone file. All of the advantages of using a laser over a scalpel are apparent in using this technique, including the excellent visualization resulting from superior hemostasis and a dry surgical site. The surgical site is then closed with sutures.
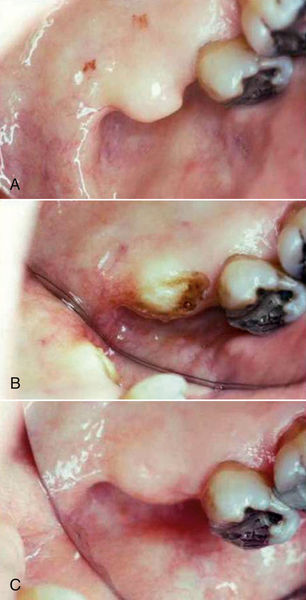
• Figure 9-3 Tuberosity reduction. A, Preoperative photograph of enlarged soft tissue tuberosity. B, Tuberosity reduction performed using a simple ablation technique, with no incision or sutures. C, Postoperative view of surgical site at 17 days. Note excellent healing and reepithelialization of surgical site. Excellent contours of site have been achieved without incisions or sutures. (Courtesy Dr. Stuart Coleton, Chappaqua, New York.)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


