Juvenile idiopathic arthritis is a childhood disease that causes joint swelling and pain, and limitation in the range of joint movements. It is characterized by progressive destruction of the joints. Juvenile idiopathic arthritis is the most frequent systemic inflammatory disease of the temporomandibular joint. When the temporomandibular joint is involved, orthodontic treatment becomes more challenging. This case report shows the treatment of a young patient with a Class II subdivision malocclusion and juvenile idiopathic arthritis. Excellent results were achieved and maintained at the 6-year follow-up, when neither clinical symptoms nor radiographic changes in the temporomandibular joint were seen.
Highlights
- •
Patients with juvenile idiopathic arthritis can receive orthodontic treatment.
- •
Juvenile idiopathic arthritis is a disease that challenges orthodontists.
- •
The TMJ could be affected by juvenile idiopathic arthritis.
- •
The 6-year follow-up shows that excellent outcomes were still observed.
- •
There were no clinical symptoms or radiographic changes in the TMJ during treatment.
Arthritis is a disease that causes swelling within a joint or limits the range of joint movements with joint pain or tenderness that persists for at least 6 weeks. It is not primarily due to mechanical disorders or to other identifiable causes. Juvenile idiopathic arthritis (JIA) is a type of arthritis of unknown etiology that begins before the sixteenth birthday. This pathology was previously called juvenile chronic arthritis or juvenile rheumatoid arthritis. The change of its name was aimed to more accurately identify homogeneous groups of children with distinct clinical features. The prevalence of JIA varies between 16 and 150 people per 100,000 worldwide. In the United States, 200,000 children are affected; this makes JIA the most common rheumatic disease in childhood. It affect girls more frequently than boys, in a ratio of 3:1.
The International League of Associations for Rheumatology classification of JIA established 7 subtypes: systemic arthritis, oligoarthritis, polyarthritis (rheumatoid factor negative), polyarthritis (rheumatoid factor positive), psoriatic arthritis, enthesitis related arthritis, and undifferentiated arthritis. Each subtype has a different prevalence due to location and ethnicity, and each is characterized by a distinct mode of presentation, disease course, and outcome.
The manifestations of JIA are chronic joint inflammation, perforation of joint epithelium, and destruction of cartilage and subchondral bone. General symptoms can include lethargy, reduced physical activity, poor appetite, and flu-like symptoms. The common feature of all JIA subtypes is arthritis. Joint inflammation results in pain, loss of function, and morning stiffness. The chronic inflammatory process arising from rheumatoid arthritis causes a progressive destruction of joints, affecting fingers, wrists, hands, ankles, feet, toes, elbows, shoulders, hips, and knees symmetrically. It can affect the temporomandibular joint (TMJ) and is the most frequent systemic inflammatory disease involving this area.
The major concern in the treatment of this disease for rheumatologists, pediatricians, oral surgeons, and especially orthodontists is involvement of the TMJ, which is considered the most important growth center of the mandible. The destruction of the chondral part of the condyle can severely impact mandibular development and growth, with alterations in size and form of the mandible, the lower third of the face, and positions of the mandibular teeth. Reports of TMJ involvement in JIA range from 17% to 87%. Radiographic changes in the TMJ vary between 17% and 63%. The diagnosis of JIA activity in the TMJ is more difficult than in other joints because clinical symptoms and signs in the TMJ are often missing or weak and do not seem to be clinically evident. When detected, in many cases, they are in such a severe stage of growth alteration that the treatment becomes more complicated.
The main skeletal and dentofacial issues related to JIA include mandibular micrognathia and retrognathia, a steep mandibular plane angle, and an increase in profile convexity. There is a marked tendency to a Class II Division 1 malocclusion, anterior open bite, and increased overjet. Increased lower facial height and vertical direction of the growth pattern are also observed.
In this article, we reviewed the relationship between JIA and orthodontics, and demonstrated the long-term successful outcome of conservative orthodontic treatment in a patient with a Class II malocclusion and small and thin condyles.
Diagnosis and etiology
A girl, age 12 years 7 months, came with the chief complaint of “protruded and apart teeth.” At 7 years of age, she had been diagnosed as having JIA, polyarthritis (rheumatoid factor negative), and she started therapy in the Pediatric Rheumatologic Clinic at São Lucas Hospital of Pontifical Catholic University of Rio Grande do Sul in Brazil. The family searched for medical care because she had signs of a significant deformity in her hands. She complained of cervical pain, daily morning joint stiffness, and edema in her ankles. No TMJ symptoms were reported.
With the diagnosis of JIA, she immediately began therapy with methotrexate until complete reversal of joint stiffness and normalization of inflammatory markers. Physical therapy was prescribed once a week, but after 1 year her symptoms recurred. After laboratory results, chloroquine diphosphate was substituted for the previously prescribed methotrexate. At 11 years of age, she underwent a tenoplasty in the left hand extensors. At 12 years of age, tenolysis of the left hand and a dorsal capsulectomy of the right hand were performed. Several years later, based on subsequent changes in the results of the laboratory tests, the medication was changed to hydroxychloroquine; the clinical response was excellent, and hepatic functions were normalized and have remained normal ever since.
The pretreatment facial photographs ( Fig 1 ) show that her facial profile was convex with a retrognathic mandible. An obtuse nasolabial angle, a slightly increased anterior lower facial height, and hypotonic lips without a passive seal were observed. She had good incisor exposure at rest and a high smile line. Mandibular and facial symmetry could be seen. Involvement of the joints of her fingers, hands, and wrists can be seen in the hand and wrist photographs ( Fig 1 ).
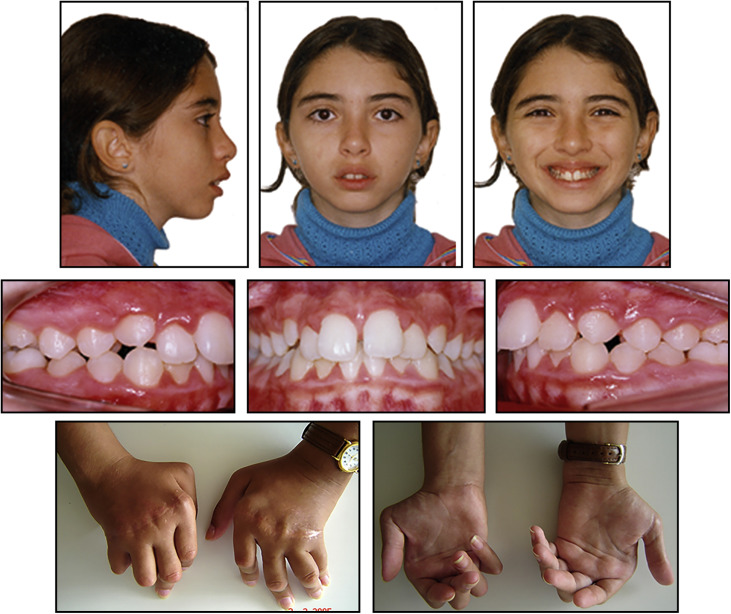
The intraoral photographs ( Fig 1 ) and digital models ( Fig 2 ) show that she had a Class II subdivision right malocclusion. The molars and canines on the right side were in a Class II relationship. Overjet and overbite were 6.0 and 4.0 mm, respectively.
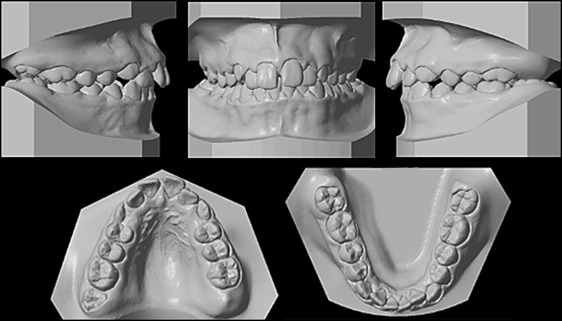
Crowding was minimal in both arches. There was coincidence between the maxillary and mandibular dental midlines, and they were aligned with the facial midline. A maxillary median diastema was present. The patient’s hygiene was extremely deficient because of the marked motor difficulty of her affected joints (hands, fingers, and wrists).
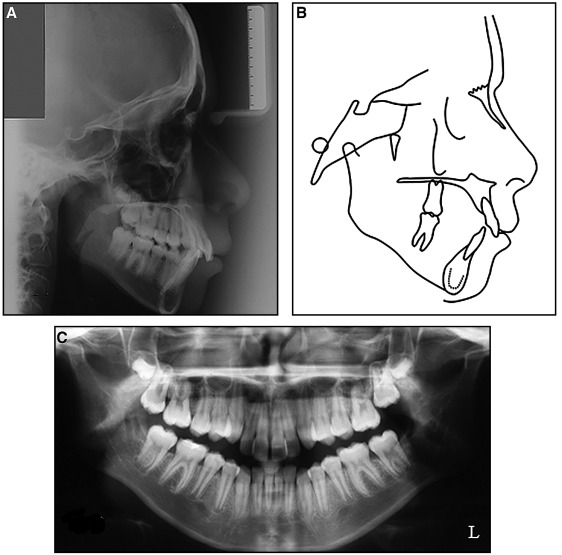
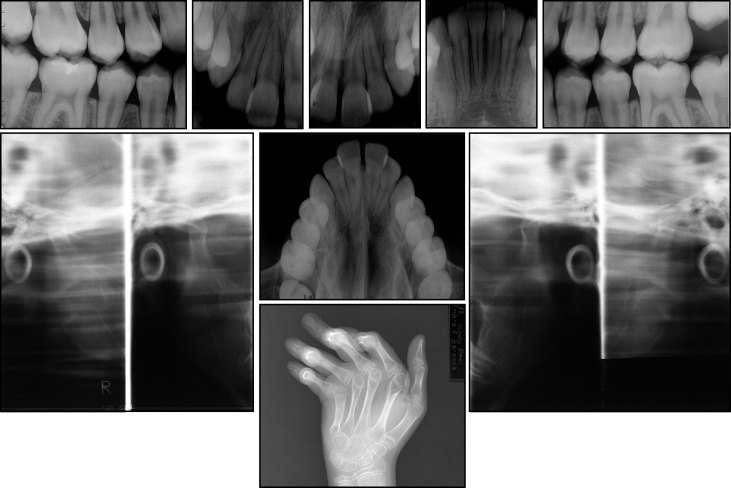
The radiographic examination ( Figs 3 and 4 ) showed the maxillary third molars, a thin condyle (but with no signs of resorption), a shallow glenoid cavity, and deformities in the bones of the hands and wrists. The cephalometric analysis ( Table ) shows a skeletal Class II relationship (ANB, 6.0°). The maxillary incisors were upright (1-NA, 4 mm; 1.NA, 17°), and the mandibular incisors were slightly protruded (1-NB, 5 mm; 1.NB, 26°). Considering the values of the occlusal plane angle (Occl.SN, 25°), the mandibular plane angle (GoGn.SN, 40°), the y-axis (y-axis to Frankfort horizontal, 63°), and the facial angle (NPog.Frankfort horizontal, 80°), a predominantly vertical growth pattern and a downward rotation of the mandible were visible. Her upper and lower lips were protruded (S-Ls, 3 mm; S-Li, 3 mm).
| Measurement | Pretreatment | Posttreatment | 6 years posttreatment |
|---|---|---|---|
| SNA (°) | 79 | 78 | 77 |
| SNB (°) | 73 | 73 | 73 |
| ANB (°) | 6 | 5 | 4 |
| 1-NA (mm) | 4 | 4 | 4 |
| 1.NA (°) | 17 | 19 | 18 |
| 1-NB (mm) | 5 | 6 | 6 |
| 1.NB (°) | 26 | 25 | 25 |
| U1.L1(°) | 129 | 130 | 132 |
| Occl.SN (°) | 25 | 26 | 29 |
| GoGn.SN (°) | 40 | 42 | 42 |
| S-Ls (mm) | 3 | 2 | 2 |
| S-Li (mm) | 3 | 2.5 | 2.5 |
| y-axis to FH (°) | 63 | 64 | 64 |
| NPog.FH (°) | 80 | 80 | 81 |
| Angle of convexity (°) | 15 | 9 | 9 |
| Wits appraisal (mm) | 2 | 2 | 2 |
| FMA (°) | 34 | 35 | 35 |
| FMIA (°) | 58 | 58 | 58 |
| IMPA (°) | 88 | 87 | 87 |
| Nasolabial angle (°) | 108 | 102 | 100 |
| A.N perp (°) | 1 | 1 | 0 |
| Co-A (mm) | 88 | 86 | 88 |
| Co-Gn (mm) | 108 | 108 | 110 |
| AIFH (mm) | 70 | 80 | 80 |
| Pog.N perp (°) | −8 | −7.5 | −7 |
Treatment objectives
The patient had a Class II subdivision right malocclusion (with a skeletal Class II relationship), convex profile without passive lip seal, and slight crowding in both arches. The treatment objectives were to (1) achieve a functional and normal occlusion with ideal overjet and overbite, (2) solve the maxillary and mandibular crowding, (3) achieve passive lip seal, (4) establish symmetric and coordinated arches, (5) improve the appearance of the facial profile, and (6) maintain the integrity without worsening the TMJ symptoms.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


