The mainstay of periodontal assessment is clinical probing. Radiographic assessment provides quantitative information on the status of tooth-supporting bone. This article reviews methods to assess periodontal structures, including basic radiograph acquisition, assessment of alveolar crest levels, and typical patterns of bone loss. Computer technology to objectively assess loss of alveolar crest from radiographs is reviewed. Developments in computer-assisted quantitation of alveolar crest height are described. Although probing measurements continue to be viewed as more practical than radiographic measurements, radiographic assessment can be made quantitative and is likely easier and more precise than probing for routine assessment of periodontal disease activity.
Key points
- •
Although the mainstay of periodontal assessment is clinical probing, radiographic assessment also has the potential to provide facile quantitative information on the status of tooth-supporting bone.
- •
Although probing measurements are viewed as more practical than radiographic measurements, radiographic assessment can be made quantitative and may prove to be more precise for routine assessment of periodontal disease activity.
- •
Intraoral radiographs are indispensable for assessment of periodontal disease status.
- •
Systems are now under development that will enable the practitioner to measure alveolar bone levels for longitudinal assessment of disease activity and could provide more objective criteria to manage patients.
Introduction
Periodontitis, which is caused by inflammatory processes initiated by bacteria that colonize as oral biofilms (dental plaque) on teeth, results in tissue destruction that manifests as gingival pockets, periodontal ligament destruction, and loss of tooth-supporting alveolar bone. A variety of methods are used to evaluate the periodontium to assess periodontal status. These methods include visual description of the gingival tissues, periodontal probing, and radiographic assessment of underlying bone.
Tissue destruction resulting from periodontitis has been found to follow an irregular time course, and may occur as episodic “bursts.” The disease can remain stable and then progress rapidly, often at individual tooth sites. For some individuals, tissue destruction can be minimal, even in the presence of poor bacterial biofilm control, whereas for others tissue destruction can be extensive and result in tooth loss. The cause for this difference in susceptibility may be related to systemic, environmental or genetic risk factors (eg, smoking, diabetes mellitus, human immunodeficiency virus infection, and stress).
Clinical examination, including periodontal probing and assessment of gingival inflammation (bleeding on probing), is the mainstay of periodontal diagnosis and disease assessment. A variety of clinical assessment indices can be used, each with its own advantages and limitations. These include the periodontal index, periodontal disease index, gingival index, and sulcus bleeding index. The periodontal index is designed to give more attention to periodontal tissue destruction compared with gingival inflammatory status, and it follows a scoring system ranging from 0 to 8, where a 0 score reflects the absence of both gingival inflammation and supporting tissue destruction, and a score of 8 reflects advanced periodontal destruction with tooth mobility and/or migration. On the other hand, the periodontal disease index is designed to measure the periodontal status of 6 preselected teeth, known as the “Ramfjord teeth,” which are the maxillary right first molar, maxillary left central incisor, maxillary left first premolar, mandibular left first molar, mandibular right central incisor, and mandibular right first premolar.
The gingival index system provides an overall assessment of gingival inflammatory status that can be used clinically to compare the efficiency of phase I treatment and to compare results before and after surgical therapy, as well as establishing good interexaminer and intraexaminer calibration between dentists. The sulcus bleeding index system is designed to give reproducible assessment of the gingival status, which is characterized by early detection of inflammatory changes at the base of the pocket or gingival crevice that are not easily detectable or visible with ordinary clinical examination. In addition, this index can be used to motivate the patient to perform better oral hygiene measures, because gingival bleeding is an early sign of disease development.
Comprehensive clinical periodontal examination requires periodontal charting of all teeth. It is known, however, that probing is not precise because a good deal of variation is inherent to the procedure. To provide periodontal care that provides timely intervention to prevent progression of disease, there is a need for a more precise method to monitor tissue destruction.
Introduction
Periodontitis, which is caused by inflammatory processes initiated by bacteria that colonize as oral biofilms (dental plaque) on teeth, results in tissue destruction that manifests as gingival pockets, periodontal ligament destruction, and loss of tooth-supporting alveolar bone. A variety of methods are used to evaluate the periodontium to assess periodontal status. These methods include visual description of the gingival tissues, periodontal probing, and radiographic assessment of underlying bone.
Tissue destruction resulting from periodontitis has been found to follow an irregular time course, and may occur as episodic “bursts.” The disease can remain stable and then progress rapidly, often at individual tooth sites. For some individuals, tissue destruction can be minimal, even in the presence of poor bacterial biofilm control, whereas for others tissue destruction can be extensive and result in tooth loss. The cause for this difference in susceptibility may be related to systemic, environmental or genetic risk factors (eg, smoking, diabetes mellitus, human immunodeficiency virus infection, and stress).
Clinical examination, including periodontal probing and assessment of gingival inflammation (bleeding on probing), is the mainstay of periodontal diagnosis and disease assessment. A variety of clinical assessment indices can be used, each with its own advantages and limitations. These include the periodontal index, periodontal disease index, gingival index, and sulcus bleeding index. The periodontal index is designed to give more attention to periodontal tissue destruction compared with gingival inflammatory status, and it follows a scoring system ranging from 0 to 8, where a 0 score reflects the absence of both gingival inflammation and supporting tissue destruction, and a score of 8 reflects advanced periodontal destruction with tooth mobility and/or migration. On the other hand, the periodontal disease index is designed to measure the periodontal status of 6 preselected teeth, known as the “Ramfjord teeth,” which are the maxillary right first molar, maxillary left central incisor, maxillary left first premolar, mandibular left first molar, mandibular right central incisor, and mandibular right first premolar.
The gingival index system provides an overall assessment of gingival inflammatory status that can be used clinically to compare the efficiency of phase I treatment and to compare results before and after surgical therapy, as well as establishing good interexaminer and intraexaminer calibration between dentists. The sulcus bleeding index system is designed to give reproducible assessment of the gingival status, which is characterized by early detection of inflammatory changes at the base of the pocket or gingival crevice that are not easily detectable or visible with ordinary clinical examination. In addition, this index can be used to motivate the patient to perform better oral hygiene measures, because gingival bleeding is an early sign of disease development.
Comprehensive clinical periodontal examination requires periodontal charting of all teeth. It is known, however, that probing is not precise because a good deal of variation is inherent to the procedure. To provide periodontal care that provides timely intervention to prevent progression of disease, there is a need for a more precise method to monitor tissue destruction.
Radiographic assessment of alveolar crest level
In most cases, clinical examination is supplemented with radiographic assessment. Radiographic examination and assessment of alveolar crest levels around individual teeth is a useful diagnostic adjunct to clinical periodontal examination. In general, radiographic examination allows for the accurate evaluation of crestal bone architecture, crown–root ratios, the presence of vertical or horizontal bone defects, furcation involvements, and the overall morphology of bone. Ideal radiographic imaging should satisfy the following criteria to achieve the most accurate diagnosis :
- 1.
The radiograph should record the complete area of interest, to allow assessment of alveolar crest height and the presence of furcation involvement or vertical bone defects.
- 2.
Radiographic distortion should be minimized by use of proper x-ray projection geometry.
- 3.
Radiographs should have the optimal contrast and density.
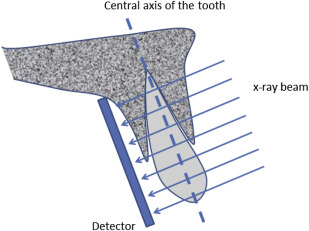
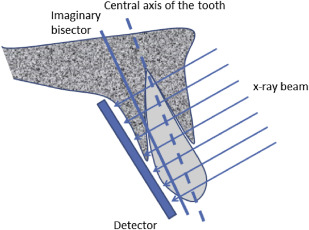
Periapical or bitewing radiographs are the most common types of radiographs used for the evaluation of periodontal bone loss. Periapical radiographs use 2 different types of projection techniques —the parallel projection technique (or right angle-long cone technique), or the bisecting angle technique. The goal of the parallel projection technique is to position the x-ray film parallel to the tooth so that the beam hits both the tooth and the x-ray film at right angles ( Fig. 1 ), resulting in minimal geometric distortion. The bisecting angle technique ( Fig. 2 ) is best described by Cieszynski’s rule of isometry, which states that 2 triangles are equal when they share 1 complete side and 2 equal angles. The clinical application of this is achieved by placing the film as close as possible to the lingual surface of the teeth, because the plane of the film and the long axis of the teeth will form an angle with its apex at the point where the tooth and film come in contact. An imaginary line is formed that bisects the triangle, and the x-ray beam is directed along this line and called the bisector. This results in 2 triangles with equal angles and a common side. When this technique is performed accurately, the resulting tooth image has a length equal to the tooth itself, which is an advantage compared with the parallel technique. However, the bisected angle technique has 2 limitations. The first regards multirooted teeth, where the central bisecting beam must be angled differently for each root. The second limitation is related to the alveolar ridge, which is usually projected more coronally than its true position when compared with the parallel projection technique. In general, periapical radiographs are preferred to bitewing radiographs when there is the need to accurately assess important anatomic structures, such as the mandibular nerve, the mental foramen, and the floor of the maxillary sinus. In addition, the periapical film can also be used to evaluate the presence or absence of periapical pathology.
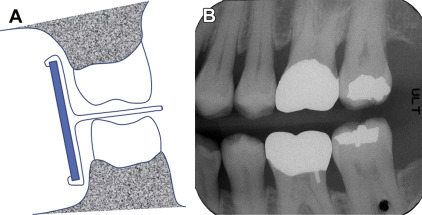
Bitewing radiographs differ from periapical radiographs in that they are usually limited to capturing the image of the crowns of both maxillary and mandibular posterior teeth along with the alveolar crest in the same radiographic film. Bitewings are used commonly in general practice for dental caries detection as well as for evaluation of alveolar crest height around teeth. The horizontal bitewing technique uses the x-ray beam aligned between the teeth and penetrates through the contact areas, while at the same time being parallel to the occlusal plane ( Fig. 3 A ). The ideal bitewing radiograph provides a clear view of the mandibular and maxillary alveolar bone and teeth with minimal overlap between the teeth. Vertical bitewings differ from horizontal bitewings in that the radiographic film has greater vertical dimension to allow for more complete evaluation of the alveolar bone in patients expected to have moderate to severe periodontal bone loss (see Fig. 3 B). Precise detection of proximal caries is considered an advantage of the horizontal bitewing technique, whereas the unobstructed view of the alveolar bone is the advantage of the vertical bitewing technique, which makes the latter a more valuable diagnostic tool for periodontal disease assessment.
Rapid developments in computer technology have allowed for the development of digital radiographic imaging procedures, which minimize processing errors inherent to conventional (analog) radiographic techniques. Among these technological innovations is digital subtraction radiography, which is based on subtraction of 2 images of the same object, recorded at different times. This technique is useful in detection of changes in tissue density between baseline and follow-up examinations. In general, the radiographic changes are either reflected as bright or dark areas. A bright area indicates gain in tissue density (mostly bone), whereas a darker area indicates tissue loss. The main disadvantage of subtraction radiography is that the geometry of the baseline image must be reproduced exactly in follow-up images or differences in geometry appropriately corrected for; otherwise, obfuscating artifacts appear in the image.
Another recent advance in diagnostic imaging is the computer-assisted densitometric image analysis system (CADIA). CADIA uses digitized radiographic information to measure the light transmitted through the radiograph, which is then converted into a gray-scale image that is then transferred to the computer where mathematic manipulations of the images take place that can be displayed, manipulated, and interpreted. This technique can also be used to assess alveolar bone density over time, similar to subtraction radiography. CADIA is more sensitive, accurate, and reproducible when compared with subtraction radiography. CADIA has been used in longitudinal clinical studies to follow the progression of periodontal bone loss and clinical attachment loss, and is shown to be more reliable compared with conventional radiographic techniques.
As used in most clinical settings, radiographic examination of periodontal disease does not permit accurate detection of minor destruction of alveolar bone. Rather, radiographs demonstrate bone loss only after a significant amount of bone destruction has already occurred. It has been reported that the difference between clinical alveolar crest height and radiographic crest height can range from 0 to 1.6 mm, with the radiographic measurements very much affected by radiographic beam angulation.
Periodontal disease shows radiographic changes that usually start as a “fuzziness” or discontinuity of the lamina dura on the mesial and distal aspects of the interdental septa. This will then transform into a wedge-shaped radiolucent area in the interdental septa. Afterward, bone destruction will seem to extend across the interdental septa and finally as a marked reduction in the height of interdental septum, resulting in a periodontal bone defect. However, there are several anatomic factors that can affect the morphology of periodontal bone defects those listed in Box 1 . Additional factors that can complicate interpretation of the morphology of periodontal bone include the presence of exostoses, trauma from occlusion, buttressing bone formation, and food impaction.
- 1.
The thickness, width, and angulation of the alveolar crest.
- 2.
Thickness of lingual and facial alveolar bone plates.
- 3.
Presence of fenestration and dehiscence.
- 4.
Tooth alignment in the jaw.
- 5.
Root and root trunk anatomy.
- 6.
Root position within the alveolar process.
- 7.
Proximity with another tooth surface.
There are several patterns that develop regarding the distribution and classification of bone loss in periodontal disease patients. Horizontal bone loss is the most common pattern of bone loss in chronic periodontitis. Generally, the overall bone height is reduced while the margins of the alveolar crest are perpendicular to the tooth surface. Horizontal bone loss usually affects the facial and lingual plates of the interdental septa of a group of teeth or even all teeth in the mouth. In contrast, osseous defects are common in patients with periodontal disease. Osseous defects can be detected on radiographs or more precisely evaluated during surgical procedures to know their exact morphology and extent, and to plan suitable treatment approaches for each type of defect. The most common osseous defects are vertical defects, defined as bone loss occurring in a vertical or oblique direction resulting in a hollowed-out trough within the bone alongside a root surface, while the base of the defect is located apical to the surrounding bone. These types of defects usually occur as intrabony (infrabony) defects. These unique defects are often classified according to the number of the osseous walls involved in the destructive process. So, for example, 1-wall defects, 2-wall defects, and 3-wall defects can be described. However, when the number of osseous walls differs between the apical and the occlusal portion of the defect, the defect is termed a combined osseous defect. Vertical defects are more likely to occur on the mesial and distal aspects of teeth, and the molar teeth are more commonly affected (the second and third maxillary and mandibular molars), especially in the case of 3-wall defects (also referred to intrabony [infrabony] defects). One-wall defects, also termed hemiseptal defects, offer great challenge to radiographic assessment because they can be obscured by radiopaque facial, palatal, and lingual plates of bone. In some cases, the only diagnostic option is surgical exploration to appropriately assess and manage such defects.
Reverse architecture is observed more commonly in the maxilla compared with the mandible. This occurs as a result of the loss of interdental bone of the facial, lingual, and palatal plates, whereas radicular bone is preserved. Thus, bone heights seem to be reversed from the normal architecture of alveolar bone.
Osseous craters appear as continuous concavities of bone that affect multiple surfaces of teeth, for example, interdental, facial, lingual, and/or palatal bone. These defects constitute more than one-third of all defects and are most commonly found to affect the posterior teeth. These types of defects tend to affect posterior teeth because bone around these teeth tends to have a flat interdental bone configuration when compared with anterior segments of teeth.
Furcation involvements are defined as the loss of bone in the bifurcation or trifurcation area of multirooted teeth. Furcation involvements are classified into four grades according to the amount of bone loss and tissue destruction (grade I, incipient bone loss; grade II, partial bone loss [or so-called CUL-DE-SAC defects]; grade III, total loss of radicular bone with a through-and-through opening of the furcation, but without gingival recession; grade IV, similar to grade III, but with gingival recession, which makes the furcation clinically visible). The radiographic assessment of furcation involvement is helpful and useful in evaluation of grade III and IV lesions. But, the angulation of the x-ray beam might result in the overlap of neighboring radiopaque structures to obscure this assessment.
Several other patterns of alveolar bone loss are encountered less commonly. A marginal gutter is defined as a shallow linear defect between the margin of a radicular cortical plate or interdental crest and along the length of 1 or more root surfaces. A dehiscence usually occurs in the form of a U-shaped or angular defect on the facial or lingual alveolar plates and also involving the marginal crest of bone of the tooth. A fenestration occurs in the form of circumscribed well-demarcated defect on the lingual or facial plate without the involvement of marginal crest of bone.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


