Mandibular first molars are among the most frequently missing teeth in the adult dentition. As a result, the maxillary first molars are frequently overerupted. Conventional approaches to correct this undesirable molar position with skeletal anchorage usually include both buccal and palatal orthodontic mini-implants. Because palatal mini-implants have greater success rates than buccal ones, this article explains an intrusion method with only palatal mini-implants and limited fixed appliances to produce reliable intrusion of the overerupted molar while preventing undesirable side effects on the adjacent teeth.
Highlights
- ●
Bodily intrusion of a single overerupted maxillary molar is possible with only palatal mini-implants.
- ●
Combined use of direct and indirect anchorage increases the available insertion sites.
- ●
Bone levels around the extruded molar should be evaluated carefully before intrusion to avoid introducing vertical osseous defects.
Most orthodontic practitioners in the United States have gained at least a limited experience with orthodontic mini-implants. Some treatment approaches with mini-implants can be considered standard today in modern orthodontic practices because they treat conditions that are difficult to correct with conventional orthodontic mechanics. Molar protraction and single molar intrusion belong to this group and are among the most common indications for orthodontic mini-implants. This should come as no surprise, considering the prevalence of congenitally missing mandibular second premolars and the fact that first molars frequently fall victim to carious decay and are extracted as a result. This loss of first molars is the reason that orthodontists are often faced with the correction of overerupted maxillary molars in an adult patient.
Traditional approaches to correct this problem orthodontically use removable or fixed appliances with the adjacent teeth for anchorage and frequently require patient compliance, or run the risk of introducing an occlusal cant. More contemporary approaches use skeletal anchorage to avoid these shortcomings. Park et al introduced a widely used solution with a palatal mini-implant and a buccal mini-implant or bone plate and an elastomeric module stretched over the occlusal surface of the tooth or to buccal and lingual attachments. Although it is a simple approach, it provides the 2 essentials necessary to achieve this otherwise difficult orthodontic correction: rigid apical attachments as anchors for elastic modules, and bodily intrusion (force application through the center of resistance).
Although simple, this approach has several disadvantages that mainly relate to the buccal anchorage point. Use of a bone plate will drive up the cost and the invasiveness of installing skeletal anchorage. The procedure would have to be referred out of the orthodontic practice. This anchorage type would thus cause a greater financial and treatment burden to the patient and can be avoided by using a mini-implant on the buccal aspect also. However, buccal orthodontic mini-implants have lower success rates than do bone plates and also do not perform as well as palatal mini-implants.
Since any biomechanical setup with mini-implants is only as good as the anchorage provided by the screws, our goal in this article was to introduce a different approach to the intrusion of overerupted molars by using 2 palatal mini-implants and only limited fixed appliances, which can deliver reliable intrusion of the overerupted molar and prevent undesirable extrusive side effects on the adjacent teeth.
Treatment
A 29-year-old Asian woman came to the Department of Orthodontics at Case Western Reserve University, Cleveland, Ohio, with a desire for limited orthodontic treatment. Her goal was correction of the overerupted maxillary right first molar to allow placement and proper restoration of a dental implant at the site of her previously extracted mandibular right first molar. It had been missing for many years and allowed the antagonist to extrude over time ( Fig 1 ).

To avoid a full maxillary bonding and the associated side effects mentioned above, the treatment plan consisted of partial braces in the maxillary right quadrant supported by 2 orthodontic mini-implants for pure intrusion of the maxillary right first molar.
For this particular intrusion setup, the location of the mini-implants should be on the palatal slope of the alveolar process, ideally mesial and distal to the overerupted molar: in this case, the maxillary right first molar ( Fig 2 ). The implant site should be chosen based on the availability of sufficient cortical bone for anchorage of the mini-implant and adequate bone depth to prevent violation of the sinus, if possible. The mesial and distal interradicular areas of the maxillary first molar have on average uniformly good bone depth and cortical bone thickness, so that the exact distance from the crest can be determined by other factors such as accessibility, gingival thickness, and biomechanics. This was confirmed by 3-dimensional imaging of the patient ( Fig 3 ).

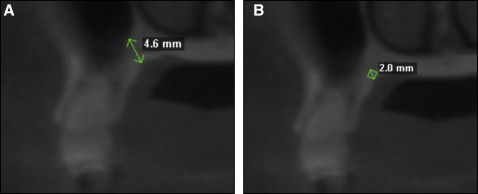
Baumgaertel and Pasold suggested that mini-implant length should generally be as short as possible. Since both cortical bone thickness and bone depth were sufficient, they were not a factor for the selection of the screw length. However, with gingival thickness of approximately 4 mm, the soft tissues were considerably greater at both sites than the 2-mm transmucosal collar of the mini-implant (TOMAS-PIN SD; Dentaurum, Ispringen, Germany). In addition, the site had only approximately 4.5 mm of total bone depth. Therefore, an 8-mm implant was chosen for both sites to ensure sufficient retention in the bone while preventing embedding of the implant head in the surrounding mucosa and violation of the sinus.
Implant diameter was not a consideration because the mini-implant used has but one choice of diameter, and the insertion site chosen had plenty of interradicular distance, so that proximity of the implant to the roots was not a concern.
With a self-drilling mini-implant at this site, ideal insertion torque levels can be expected in an average patient without implant-site preparation. This patient, however, had greater than average cortical bone thickness at both sites (2 mm); this necessitated a cortical bone perforation preceded by a tissue punch to achieve ideal insertion torque levels and clean peri-implant gingival margins. After the implant site preparation, the pins were seated with approximately 10 N·cm of final insertion torque.
With 2 palatal mini-implants securely in place on the palatal slope of the alveolar process, mesial and distal to the overerupted maxillary right first molar, the first criterion for a single molar intrusion setup was fulfilled: 2 rigid apical attachments for elastic modules were present. To fulfill the second criterion—intrusive force application through the center of resistance—it is necessary to create a force system equivalent to the system described by Park et al. They chose a setup consisting of 2 anchorage points, 1 buccal and 1 palatal, loaded with direct anchorage. Such a solution results in an apically directed intrusive force and 2 similar and, for discussion purposes, equally large moments acting in opposite directions, leading to bodily intrusion of the molar.
Because both of our rigid apical attachment points were on the palate, a pure direct anchorage approach with elastic modules from the implants to a lingual attachment on the molar would result in an intrusive force with a palatally directed moment. This would tip the molar toward the mini-implants. To counteract this palatal moment, we created an additional moment, equal in magnitude but opposite in direction, by expanding this setup with rigid indirect anchorage from the mini-implant to the teeth adjacent to the overerupted molar and partial braces (Smart Clip; 3M Unitek, Monrovia, Calif) on the buccal aspect, including the second premolar and the first and second molars, and engaging an 0.018-in nickel-titanium sectional wire (Nitinol heat-activated archwire; 3M Unitek) ( Fig 4 ). Bracket positioning should be slightly occlusal on the overerupted molar and slightly gingival on the adjacent teeth. Rigid indirect anchorage was established by bonding a 0.017 × 0.025-in stainless steel wire segment (Reimanium; Dentaurum) to the lingual surfaces of the second premolar and the second molar using a lingual retainer composite (FlowTain; Reliance Orthodontic Products, Itasca, Ill) and securing these wire segments in the cross-slot head of the mini-implant with bonding material (Heliosit; Ivoclar Vivadent, Schaan, Liechtenstein).





