A young man, age 18 years 4 months, with a concave profile, a skeletal maxillary deficiency, and a severe alveolar cleft with an unesthetic appearance of the maxillary anterior teeth was referred for orthodontic treatment. After a detailed review of his pretreatment records, both surgical and nonsurgical treatment plans were presented to the patient, who opted for a nonsurgical interdisciplinary approach. His complex 3-dimensional malocclusion required palatal expansion, dental extractions, and periodontal and prosthodontic consultations and treatment, in addition to comprehensive orthodontic therapy. MBT (Xinya, HangZhou, China) 0.022 × 0.028-in appliances combined with a mini-implant to enhance the orthodontic anchorage were used to level, align, and establish a Class I relationship. After the orthodontic treatment, a combined restorative and periodontal approach was used to enhance the patient’s esthetic and functional outcomes. Both the final result and the 1-year follow-up records demonstrate that the treatment goals of establishing proper occlusion, normal function, a balanced profile, better esthetics, and a stable outcome were achieved. The purpose of this case report is to demonstrate that an interdisciplinary treatment protocol can significantly improve the transverse discrepancies and achieve a satisfactory occlusion with a balanced profile in patients with cleft lip and palate.
Cleft lip and palate (CLP) is the most frequent congenital facial abnormality. Compared with the incidence rate reported from other countries, the frequency of all forms of clefts is highest among Asians. The etiology is related to both hereditary and environmental factors. Patients with CLP can also have other features such as deficient midface development resulting in a Class III tendency, severe maxillary transverse deficiency, alveolar cleft, and hypodontia. CLP patients might also have decreased facial and dental esthetics, resulting in low self-confidence and difficulties in social interactions. Interdisciplinary treatment plans for patients with CLP frequently extend over many years, starting with primary surgeries during infancy, at least 1 stage of orthodontic treatment, and possible jaw surgery near the end of adolescence or early adulthood. Treatment frequently includes nasoalveolar molding, labial repair (about 3-6 months of age), palatoplasty (10-12 months of age), orthodontic expansion, primary or secondary alveolar bone graft, surgery, and comprehensive orthodontic treatment to reestablish facial esthetics and proper function.
One important aspect of orthodontic treatment includes transverse expansion of the maxilla to correct the transverse deficiency of the palatal segments. This can be achieved using one of several different types of expanders, including traditional screw-type rapid palatal expansion, spring-type, magnetic, and shape memory alloy. The magnetic palatal expander (MPE) with repelling magnets to increase the width of maxilla has been previously reported by Darendeliler et al. Magnets produce a suitable force without requiring additional adjustment by the patient and are more rigid than spring-type expanders, potentially resulting in fewer undesirable effects; however, there are few reports of MPE treatment in CLP patients.
This case report describes an interdisciplinary treatment approach for a young man with unilateral CLP. MPE, comprehensive orthodontics, periodontics, and nasoalveolar molding were used to obtain proper occlusion and normal function; a balanced profile and better esthetics were achieved.
Diagnosis and etiology
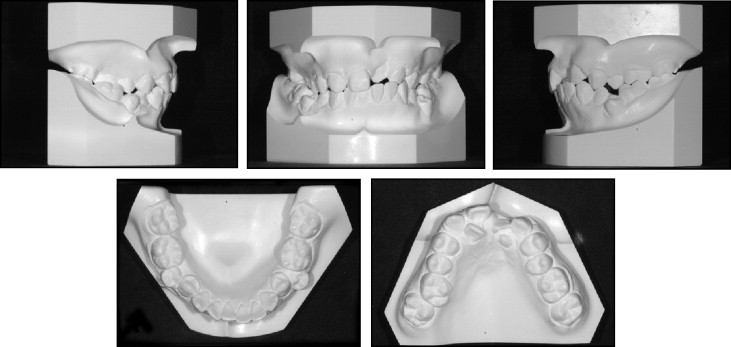
A young Chinese man (age 18 years 4 months) came to the Orthodontic Department of Nanjing University for orthodontic evaluation of his severe crowding and posterior crossbite. His chief complaint was the unesthetic appearance of his face and maxillary anterior teeth. He was born with nonsyndromic unilateral left CLP. The lip was repaired at the age of 6 months (primary cheiloplasty), and the palate (palatoplasty) was repaired at 4 years of age, with no further orthodontic treatment or alveolar bone-grafting procedures. The patient had a concave profile with a retrusive upper lip and an everted lower lip. He showed good vertical balance among the facial thirds and good symmetry except for the nose and upper lip resulting from both the cleft and the scarring from the previous surgical repair. The maxillary and mandibular dental midlines were coincident but both were deviated to the left by 2 mm ( Fig 1 ).
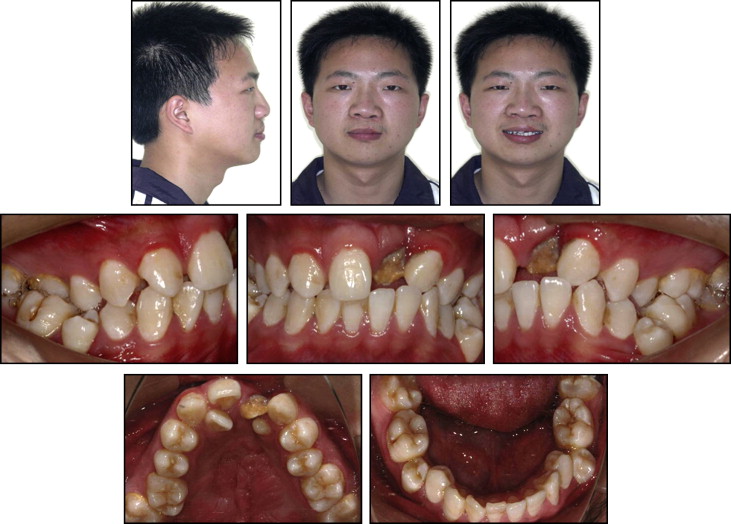
The maxillary arch was collapsed and constricted resulting from a combination of the initial cleft, the previous surgical scarring in the palate, the lack of previous expansion, and lack of alveolar bone graft, all of which contributed to the unilateral right posterior crossbite. The maxillary basal arch width was extremely narrow, as demonstrated by the width between the maxillary left and right first premolars (43 mm, measured with an electronic vernier caliper) compared with the 49.5-mm Chinese mean value. The maxillary width between the first molars was also narrow at 42 mm. The maxillary left central incisor was hypomineralized, and the left lateral incisor was both undersized and erupting ectopically into the palate. The mandibular arch had a deep curve of Spee and severe crowding with both second premolars erupting in buccally ectopic positions. The molar relationships were a mild Class III on the right and Class I on the left side ( Fig 2 ). Oral hygiene was poor, and bleeding was observed while brushing.
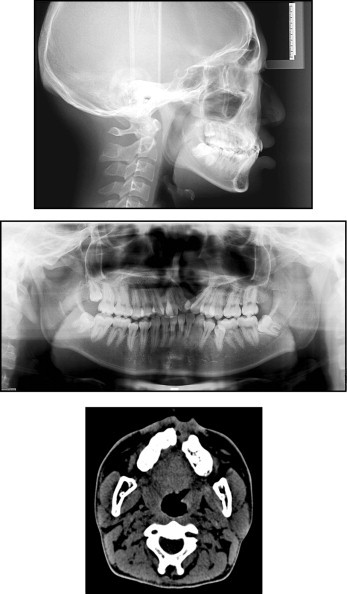
The panoramic radiograph ( Fig 3 ) showed a wide alveolar cleft between the maxillary left central incisor and the canine. The undersized maxillary lateral incisor was distal to the cleft, palatally ectopic, and severely malpositioned. The crown of the mandibular left third molar overlapped the distal aspect of the mandibular left second molar. The cephalometric analysis indicated a mild skeletal Class III tendency (ANB, −0.1°; Wits appraisal, −2 mm) with a normal facial growth pattern (SN-MP, 33.6°). The maxillary incisors were well positioned (1-NA, 25.7°; 1-NA, 6.2 mm), whereas the mandibular incisors were slightly proclined (L1-MP, 99°) ( Fig 3 , Table I ).
| Measurement | Chinese norm | Pretreatment | Posttreatment | Difference |
|---|---|---|---|---|
| SNA (°) | 82.8 | 76.8 | 77.2 | 0.4 |
| SNB (°) | 80.1 | 76.9 | 76.3 | −0.6 |
| ANB (°) | 2.7 | −0.1 | 0.9 | 1.0 |
| Wits (mm) | −1 | −2 | 0 | 2 |
| FH-NP (°) | 85.4 | 86.9 | 86.1 | −0.8 |
| SN-MP (°) | 32.5 | 33.6 | 34.5 | 0.9 |
| FMA (°) | 27.3 | 28.5 | 29.6 | 1.1 |
| U1 to SN (°) | 105.7 | 107.7 | 106.5 | −1.2 |
| U1 to NA (°) | 22.8 | 25.7 | 25.2 | −0.5 |
| U1 to NA (mm) | 5.1 | 6.2 | 5.8 | −0.4 |
| L1 to NB (°) | 30.3 | 37.6 | 35.4 | −2.2 |
| L1 to NB (mm) | 6.7 | 9.1 | 7.2 | −1.9 |
| L1 to MP (°) | 92.6 | 98.8 | 95.2 | −3.6 |
| U1/L1 (°) | 125.4 | 120.6 | 126.5 | 5.9 |
| Upper lip (mm) | 0.4 | −0.2 | 0.5 | 0.7 |
| Lower lip (mm) | 0.9 | 4.8 | 1.0 | −3.8 |
Treatment objectives
The facial goals of the treatment were to obtain a more balanced profile. Dentally, the goals were to expand the maxillary arch to resolve the maxillary transverse deficiency and correct the unilateral right posterior crossbite, level and align the dental arches, and establish a Class I molar relationship with enhanced intercuspation. The maxilla was carefully observed during expansion because of the wide alveolar cleft and the previous soft-tissue palatal repair. Restoratively, the goal was to provide an ideal space to restore the hypomineralized maxillary left central incisor to enhance the patient’s dental esthetics. To achieve these objectives, the following treatment plan was adopted.
- 1.
A fixed MPE appliance would be used initially to expand the maxillary arch.
- 2.
The palatally ectopic and undersized maxillary lateral incisors and the buccally ectopic and infraoccluded mandibular second premolars would be extracted.
- 3.
A Class I molar relationship would be established, and the lower lip protrusion would be reduced by retracting the mandibular posterior teeth with mini-implants.
- 4.
Conventional fixed prostheses (2 splinted crowns) for the maxillary left central incisor and the canine would be placed after the orthodontic treatment.
- 5.
A revision rhinoplasty would be performed.
- 6.
Retention would be needed.
It was expected that both function and esthetics would improve, but less than with a combined orthognathic surgery and orthodontic treatment approach.
Treatment objectives
The facial goals of the treatment were to obtain a more balanced profile. Dentally, the goals were to expand the maxillary arch to resolve the maxillary transverse deficiency and correct the unilateral right posterior crossbite, level and align the dental arches, and establish a Class I molar relationship with enhanced intercuspation. The maxilla was carefully observed during expansion because of the wide alveolar cleft and the previous soft-tissue palatal repair. Restoratively, the goal was to provide an ideal space to restore the hypomineralized maxillary left central incisor to enhance the patient’s dental esthetics. To achieve these objectives, the following treatment plan was adopted.
- 1.
A fixed MPE appliance would be used initially to expand the maxillary arch.
- 2.
The palatally ectopic and undersized maxillary lateral incisors and the buccally ectopic and infraoccluded mandibular second premolars would be extracted.
- 3.
A Class I molar relationship would be established, and the lower lip protrusion would be reduced by retracting the mandibular posterior teeth with mini-implants.
- 4.
Conventional fixed prostheses (2 splinted crowns) for the maxillary left central incisor and the canine would be placed after the orthodontic treatment.
- 5.
A revision rhinoplasty would be performed.
- 6.
Retention would be needed.
It was expected that both function and esthetics would improve, but less than with a combined orthognathic surgery and orthodontic treatment approach.
Treatment alternatives
The ideal treatment of resolving the maxillary transverse deficiency with skeletal expansion and an alveolar bone graft followed by orthognathic surgery to better address the skeletal imbalance was presented to the patient, but he declined. The risks of a nonsurgical treatment, particularly the increased risk of loss of teeth adjacent to the alveolar cleft (maxillary left lateral incisor and canine), potentially unstable dental expansion, and recurrence of the posterior crossbite, were discussed with the patient to provide complete informed consent.
Treatment progress
Before we started the orthodontic treatment, the patient was referred for a prosthodontic consultation regarding the possible approaches to restore the hypomineralized maxillary left central incisor and how to replace the lateral incisors by reshaping the maxillary canines. The patient was also referred to a periodontist to evaluate his periodontal health, particularly the teeth adjacent to the alveolar cleft. Finally, the patient was referred to the oral surgeon to evaluate the mesioangular and impacted maxillary right and the mandibular right and left third molars.
After consultations with the other dental specialists, maxillary expansion, the first stage of orthodontic treatment, began. Because of the potential tissue damage that can result from rapid, heavy, intermittent forces produced by a screw type of rapid palatal expansion, a fixed MPE was constructed to create slow, suitable, continuous forces. The MPE appliance, consisting of right and left halves containing 8 × 5 × 3 mm 3 neodymium (Nd 2 Fe 14 B) repelling magnets ( Fig 4 ), was cemented to the maxillary first molars and the first premolars. The expansion force produced between the magnets is greatly affected by the distance separating them, with a maximum force of 550 g with a separation of 0.5 mm. As the distance increases, the expansive force declines, requiring periodic removal and adjustment by adding acrylic to reapproximate the repelling magnets. Pins and tubes were constructed to keep the magnets in line with one another and to guide the appliance separation.




