Amelogenesis imperfecta (AI) comprises a clinically and genetically heterogeneous group of conditions that affect the dental enamel, occasionally in conjunction with other dental, oral, and extraoral tissues. The aim of this case report is to describe an interdisciplinary treatment of hypoplastic AI associated with a severe open bite. The treatment consisted of surgical, orthodontic, periodontal, prosthetic and restorative management, establishing good chewing function, dental esthetics and facial harmony.
Amelogenesis imperfecta (AI) represents a group of conditions that affect the structure and clinical appearance of the enamel of all or nearly all the teeth; it might also be associated with morphological or biochemical changes elsewhere in the body. The incidence of AI varies from 1 in 700 to 1 in 14,000 people, depending on the population studied and the diagnostic criteria used. Oral complications associated with AI include tooth sensitivity, poor dental esthetics, and decreased vertical dimension.
Some published surveys report the importance of treating the AI patient not only from a functional standpoint but also from a psychosocial standpoint. Results of the survey found that patients with AI experience higher levels of social avoidance combined with a perceived reduced quality of life compared with those without AI and that treatment has a positive psychosocial impact. The aim of this case report is to present a multidisciplinary approach to a patient with AI and a severe open bite.
Diagnosis and etiology
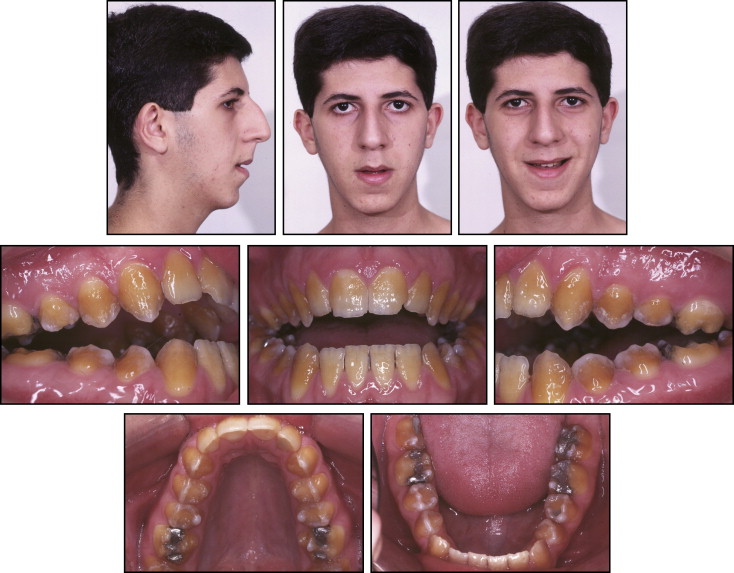
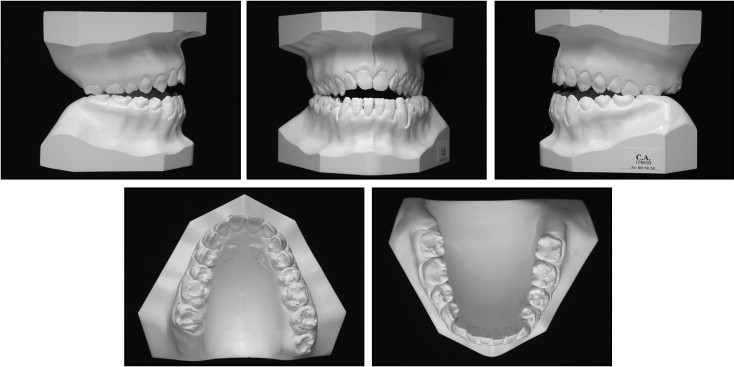
A 15-year-old boy with an angle Class I malocclusion, anterior open bite, and narrow maxilla (with posterior bilateral crossbite), as well as a long face, was referred for orthodontic treatment ( Figs 1 and 2 ). The patient was dissatisfied with the discoloration of his teeth, which was caused by hypoplastic AI.
Treatment objectives
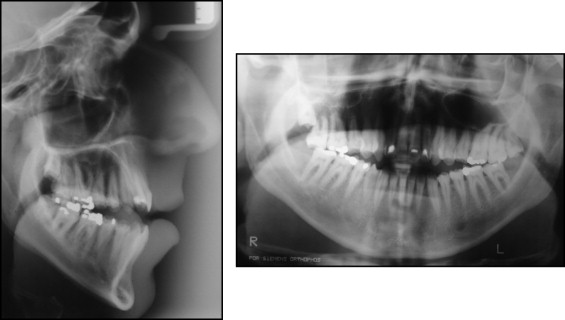
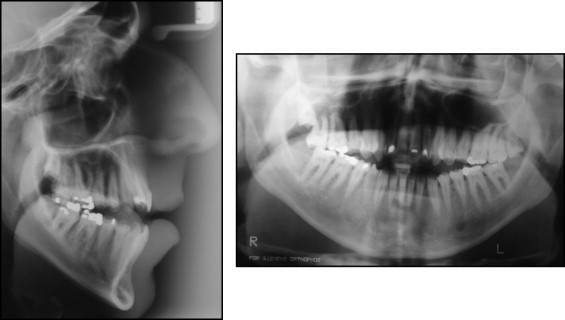
After clinical and radiograph evaluation ( Figs 2 and 3 ) it was decided that orthognathic surgery would be necessary to accomplish both orthodontic and facial goals, and the need for a dental restorative approach was also evident.
Treatment objectives
After clinical and radiograph evaluation ( Figs 2 and 3 ) it was decided that orthognathic surgery would be necessary to accomplish both orthodontic and facial goals, and the need for a dental restorative approach was also evident.
Treatment alternatives
The first orthodontic treatment alternative was edgewise arch wire therapy and anterior intermaxillary elastics, preceded by maxillary expansion. The effects of this treatment would cause extrusion of anterior teeth, correcting malocclusion by vertical compensation of the skeletal problem. Because facial disharmony was the patient’s complaint and the potential for significant relapse, this treatment option was not chosen.
The second treatment option was to use miniscrew or miniplate anchorage to intrude the posterior teeth in both arches, and to extrude the maxillary anterior teeth in order to close the anterior open bite. However, facial improvement could not be predicted accurately, and the potential change was not considered adequate enough with this treatment. Furthermore, the potential for relapse would be significant, so this treatment was also discarded.
The third alternative, and that which was chosen, involved mandibular and maxillary surgery combined with orthodontic treatment. This plan involved maxillary forward positioning and mandibular forward counterclockwise rotation along with a genioplasty. This treatment option could improve facial retrusion and correct the malocclusion with more predictability, as well as overcome the patient’s chief complaints.
Whichever orthodontic treatment was chosen, extensive restorative dentistry would be necessary after orthodontic treatment.
Treatment progress
Since the patient was still growing, treatment was delayed until facial growth was completed. Thus, the orthognathic surgery would be performed after puberty. During this interval, the patient underwent a rhinoplasty procedure, to improve nasal contour ( Fig 4 ). Prior to orthodontic treatment, the patient did not show a sufficient amount of his maxillary incisors. In addition, he had large buccal corridors when smiling and the tooth color was compromised by the AI. The facial proportions showed a vertical excess, and the lateral profile photograph revealed both maxillary and mandibular retrusion.

Orthodontic preparation involved maxillary arch expansion (Hyrax expander followed by transpalatal bar), as well as alignment and leveling, in order to achieve better arch coordination prior to orthognathic surgery.
Despite the enamel dysplasia, no bracket/bond failures were observed during treatment. Conventional enamel conditioning and bonding procedures were used (37% phosphoric acid for 30 seconds followed by rinsing and drying and the use of Rely-a-Bond adhesive (Reliance Orthodontic Products, Inc, Itasca, Ill).
After 14 months of preoperative orthodontics, hooks were attached to both arch wires ( Fig 5 ). Orthognathic surgery was performed and the maxilla and mandible were moved forward. The mandible was rotated in a counterclockwise direction and a genioplasty was also performed (pre- and postoperative radiographs shown in Fig 6 ). After 3 months of healing, the finishing phase of orthodontic treatment was accomplished ( Figs 7 and 8 ). The overall orthodontic treatment time was 29 months.





