Aggressive periodontitis is a great challenge to clinicians when providing orthodontic treatment because of the potential for progression of periodontal disease. In this article, we report the successful comprehensive orthodontic treatment of bimaxillary protrusion and severe crowding in an adult with generalized aggressive periodontitis. A woman, aged 22 years 7 months, with a chief complaint of incisal crowding was diagnosed with a skeletal Class I malocclusion associated with severe anterior crowding, possibly worsened by generalized aggressive periodontitis. In addition to a periodontal examination, a blood IgG antibody titer analysis and microbiologic examination for periodontal pathogens were used to diagnose the type of periodontal disease and determine the proper timing to initiate orthodontic treatment. The total active treatment period was 28 months, followed by periodontal prostheses and regeneration therapy. Consequently, satisfactory facial profile, occlusion, and periodontal health were maintained for at least 36 months. These results indicate that efficient screening is important for providing successful orthodontic treatment in patients with advanced periodontal disease. This report also demonstrates the diagnostic importance of blood IgG antibody titer assays and microbiologic examinations to detect periodontal pathogens.
Highlights
- •
We report the successful orthodontic treatment of a patient with generalized aggressive periodontitis.
- •
IgG antibody titer and microbiota were used to monitor the periodontal condition.
- •
Efficient screening is important for patients with severe periodontitis.
Aggressive periodontitis (AgP), an uncommon and often severe destructive periodontal disease, is primarily characterized by the rapid loss of attachment and bone destruction, usually in relatively young patients. With regard to the pathogenesis of periodontitis, oral microorganisms present in biofilms are known to contribute to the onset of the disease. In particular, Aggregatibacter actinomycetemcomitans , a periodontal pathogen, is closely associated with AgP.
Advanced periodontal disease may result in pathologic extrusion, labial inclination of the incisors, or posterior bite collapse, subsequently causing esthetic and functional problems for the patient that often require orthodontic correction. The application of orthodontic treatment in patients with AgP demands special consideration because of the potential for advanced progression of periodontal disease. The key to treating affected patients is to ensure close cooperation among the multidisciplinary team, particularly the orthodontist and the periodontist, to address the patient’s periodontal status before treatment and to determine the optimal timing of therapy to treat both periodontal and orthodontic problems. Consequently, complete periodontal screening and recording should be carried out before the orthodontic treatment, and conducting a longitudinal evaluation of the patient’s periodontal condition is important for providing optimal treatment. This strategy also helps to avoid lawsuits for any periodontal problems that may arise during treatment.
Nevertheless, in spite of increasing recognition regarding the importance of the pathology of AgP and the need to evaluate functional aspects during diagnosis and treatment, no previous reports have described the clinical assessment of these factors in orthodontic patients with AgP. Our aim in this case report therefore was to describe the results of comprehensive orthodontic treatment in a patient with generalized AgP, with a longitudinal quantitative evaluation of her periodontal condition and underlying pathogens. We also demonstrate the stomatognathic improvements achieved with successful orthodontic treatment in this patient.
Diagnosis and etiology
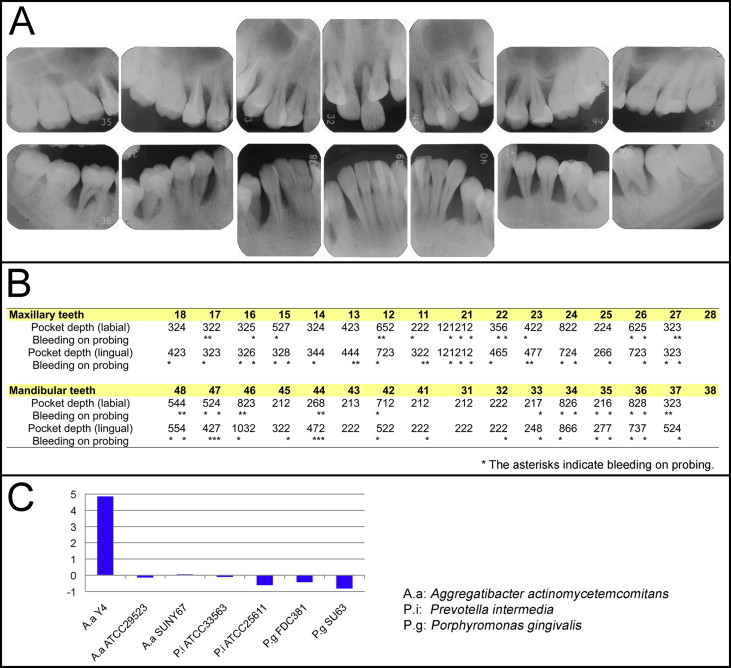
A 21-year-old woman was referred by her general dentist to the outpatient dental clinic of Okayama University Hospital in Japan for treatment of AgP. Her medical history was unremarkable. However, a full-mouth series of periapical radiographs showed severe vertical bone loss, and preserving her maxillary left central incisor was considered to be impossible because of the deep infrabony defects ( Fig 1 , A ). The initial periodontal examination showed a deep probing pocket depth with sulcus bleeding ( Fig 1 , B ). In addition to the periodontal examination, a blood IgG antibody titer assay for periodontal pathogens with an enzyme-linked immunosorbent assay (ELISA), as previously described, was used to assess the degree of periodontal disease based on the detection of humoral immunologic responses accompanying the elevation in the serum IgG antibody titers against periodontal pathogens. The results showed that the IgG antibody titer against A actinomycetemcomitans Y4, the B strain of A actinomycetemcomitans , which is frequently associated with AgP, was 4.85 times higher than the mean of 2 SD of the values observed in the healthy controls in a previous report ( Fig 1 , C ). The patient was therefore diagnosed with generalized AgP, possibly caused by A actinomycetemcomitans Y4.
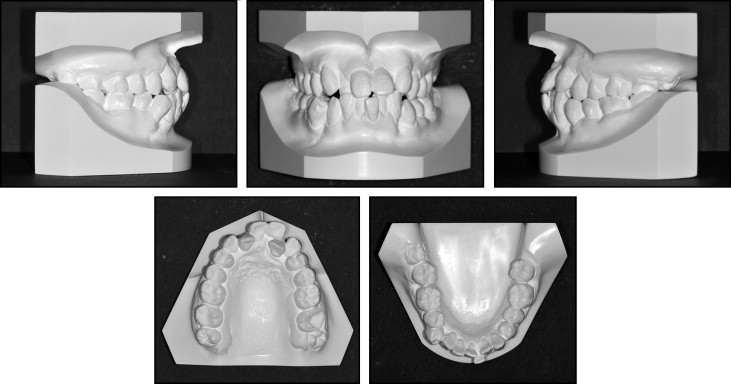
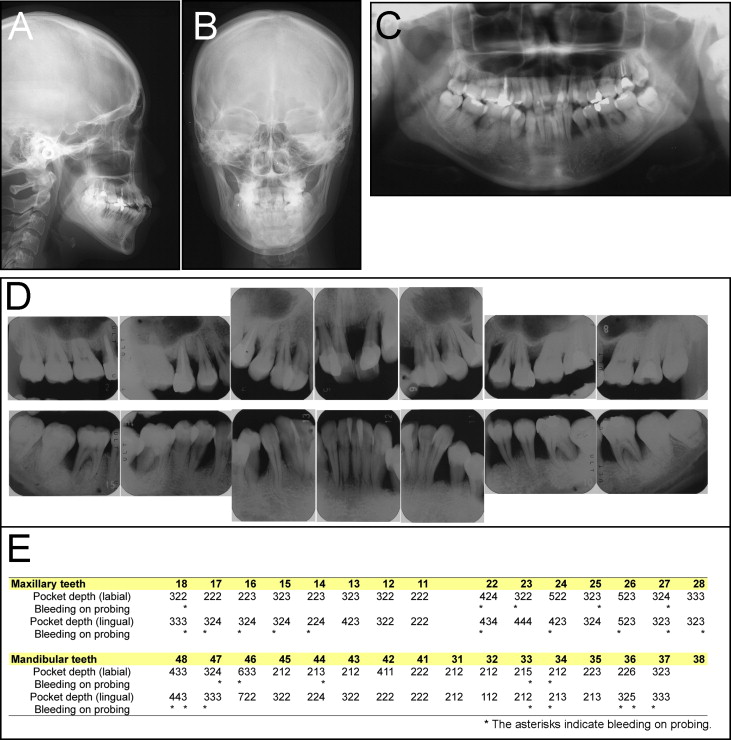
The patient was referred to our orthodontic department 1 year later at 22 years 7 months of age to discuss the possibility of orthodontic treatment. Her chief complaint was crooked teeth and difficulty in controlling dental plaque. Her facial photographs showed a symmetrical face, a convex profile, and an acute nasolabial angle ( Fig 2 ). Severe crowding was observed in both sets of incisors, and an anterior crossbite in both lateral incisors with Class II canine and Angle Class I molar relationships on both sides were also noted ( Figs 2 and 3 ). The maxillary dental midline was deviated 2.0 mm to the left on the facial side relative to the mandibular dental midline. The patient was instructed regarding oral hygiene techniques and received initial periodontal debridement therapy to assess her periodontal tissue response. The initial periodontal preparation included instructions in oral hygiene, supragingival scaling, and root planning with professional tooth cleaning and antibiotic therapy. Periodontal pocket irrigation was also performed after those procedures. At the 6-month reevaluation visit, the radiographs and measurements demonstrated distinct clinical improvements and a reduction in bleeding on probing ( Fig 4 ), although significant areas of vertical bone loss in the mandibular first molars remained evident ( Fig 4 , D ).

In comparison with Japanese norms, the results of the cephalometric analysis showed a skeletal Class I jaw relationship (ANB, 3.0°) and an average mandibular plane angle (FMA, 29.5°). In addition, the maxillary and mandibular incisors were labially inclined (U1-SN, 117.0°; IMPA, 101.0°), and the patient exhibited a decreased overjet of 0.5 mm and an overbite of −1.0 mm ( Table I ).
| Variables | Japanese norms (adult female) | SD | Pretreatment | Posttreatment | Postretention |
|---|---|---|---|---|---|
| Angular measurements (°) | |||||
| ANB | 2.8 | 2.44 | 3.0 | 3.0 | 3.0 |
| SNA | 80.8 | 3.61 | 81.0 | 81.0 | 81.0 |
| SNB | 77.9 | 4.54 | 78.0 | 78.0 | 78.0 |
| FMA | 30.5 | 3.60 | 29.5 | 29.5 | 29.5 |
| U1-SN | 105.9 | 8.79 | 117.0 | 106.5 | 108.5 |
| IMPA | 93.4 | 6.77 | 101.0 | 82.0 | 84.0 |
| FMIA | 56.0 | 8.09 | 49.5 | 68.5 | 66.5 |
| Interincisal angle | 123.6 | 10.64 | 102.5 | 132.0 | 128.5 |
| Occlusal plane to Frankfort horizontal | 16.9 | 4.40 | 17.0 | 14.5 | 14.5 |
| Gonial angle | 122.2 | 5.29 | 126.5 | 126.0 | 126.0 |
| Linear measurements (mm) | |||||
| S-N | 67.9 | 3.65 | 70.0 | 70.0 | 70.0 |
| N-Me | 125.8 | 5.04 | 130.5 | 131.0 | 131.0 |
| Me/PP | 68.6 | 3.71 | 71.5 | 71.5 | 71.5 |
| Overjet | 3.1 | 1.07 | 0.5 | 3.5 | 3.5 |
| Overbite | 3.3 | 1.89 | −1.0 | 3.0 | 2.5 |
| U1/PP | 31.0 | 2.34 | 25.5 | 26.5 | 26.0 |
| U6/PP | 24.6 | 2.00 | 23.0 | 23.5 | 23.5 |
| L1/Mp | 44.2 | 2.68 | 49.5 | 49.0 | 49.0 |
| L6/Mp | 32.9 | 2.50 | 36.5 | 37.5 | 37.5 |
| L1/AP | 5.5 | 3.00 | 10.5 | 3.0 | 3.5 |
| E-line to upper lip | −2.5 | 1.90 | 4.0 | 1.0 | 0.5 |
| E-line to lower lip | 0.9 | 1.90 | 7.0 | 4.0 | 4.0 |
Treatment objectives
Based on these findings, the patient was diagnosed with a Class I malocclusion with lip protrusion, severe incisor crowding, and advanced bone loss, possibly caused by A actinomycetemcomitans . The treatment objectives were to treat the malocclusion, provide better periodontal health, reduce the probing depths, improve the osseous topography, and establish better occlusal contacts, anterior guidance, and esthetics by leveling and retracting the incisors. We planned to extract, for orthodontic reasons, the patient’s maxillary right lateral incisor, mandibular left first premolar, and the distal root of the mandibular right first molar (hemisectioning) because of the extensive periodontal damage. We also designed interdisciplinary treatments involving orthodontic therapy, periodontal therapy with regenerative techniques, periodontal plastic surgery, prosthodontic rehabilitation, and a strictly supervised oral hygiene program. Screening of the periodontal pocket depth, bleeding on probing, blood IgG antibody titer, and microbiologic findings for periodontal disease with real-time polymerase chain reaction assays were performed by periodontists in the transition phase of each active treatment step.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


