Introduction
The purpose of this study was to evaluate craniocervical posture and hyoid bone position in orthodontic patients with temporomandibular joint (TMJ) disc displacement.
Methods
The subjects consisted of 170 female orthodontic patients who consented to bilateral magnetic resonance imaging of their TMJs. They were divided into 3 groups based on the results of magnetic resonance imaging of their TMJs: bilateral normal disc position, bilateral disc displacement with reduction, and bilateral disc displacement without reduction. Twenty-five variables from lateral cephalograms were analyzed with 1-way analysis of variance to investigate differences in craniocervical posture and hyoid bone position with respect to TMJ disc displacement status. Pearson correlation coefficients were calculated to analyze the relationships between craniofacial morphology and craniocervical posture or hyoid bone position.
Results
Subjects with TMJ disc displacement were more likely to have an extended craniocervical posture with Class II hyperdivergent patterns. The most significant differences were found between patients with bilateral normal disc position and bilateral disc displacement without reduction. However, hyoid bone position in relation to craniofacial references was not significantly different among the TMJ disc displacement groups, except for variables related to the mandible. Pearson correlation coefficients indicated that extended craniocervical posture was significantly correlated with backward positioning and clockwise rotation of the mandible.
Conclusions
This suggests that craniocervical posture is significantly influenced by TMJ disc displacement, which may be associated with hyperdivergent skeletal patterns with a retrognathic mandible.
Highlights
- •
Temporomandibular joint disc displacement is associated with extended craniocervical posture.
- •
Hyoid bone position was relatively stable regardless of temporomandibular disc displacement.
- •
Extended craniocervical posture was correlated with Class II hyperdivergent patterns in patients with temporomandibular disc displacement.
Disc displacement of the temporomandibular joint (TMJ) is a common temporomandibular disorder (TMD) and refers to an abnormal positional relationship between the articular disc and the condyle, fossa, and articular eminence. TMJ disc displacement generally progresses from a reducing to a nonreducing state and may lead to TMJ clicking, crepitus, and in some cases, pain and jaw movement limitations. Common causes of TMJ disc displacement include trauma and parafunctional habits, such as clenching and bruxism.
Various imaging techniques are available for evaluation of the TMJ, such as transcranial radiography, arthrography, tomography, computed tomography, and magnetic resonance imaging (MRI). Among them, MRI is the only modality that directly depicts the disc and is the gold standard in determining articular disc position relative to the condyle and articular eminence because of its high diagnostic accuracy. In addition, it also offers other advantages, such as noninvasiveness, lack of soft tissue distortion, minimal pain, minimal risk potential, and lack of ionizing radiation exposure. Approximately 30% of asymptomatic adults and 82% of symptomatic patients have some form of TMJ disc displacement, as determined by MRI.
Previous studies have investigated the relationship between TMJ disc displacement and dentofacial characteristics in orthodontic patients, reporting that patients with TMJ disc displacement have decreased posterior facial height as well as backward positioning and clockwise rotation of the mandible. Since craniocervical posture and hyoid bone position can be associated with dentofacial morphology, both of these features could be significantly influenced by TMJ disc displacement. However, the associations between TMJ disc displacement and craniocervical posture or hyoid bone position have not yet been fully investigated. Although the effects of TMD on craniocervical posture and hyoid bone position have been investigated, the results remain controversial. Several studies have reported an association between TMD and craniocervical posture, but others do not support the connection between TMD and craniocervical posture or hyoid bone position. The purpose of this study was to investigate the relationships between TMJ disc displacement and craniocervical posture, and between TMJ disc displacement and hyoid bone position, using MRI. The null hypothesis was that no significant relationships would be found between TMJ disc displacement and craniocervical posture, or between TMJ disc displacement and hyoid bone position.
Material and methods
Female subjects were recruited from patients who consented to bilateral MRI of their TMJs. All subjects had a primary complaint of malocclusion, and routine lateral cephalograms were taken in natural head position with an Asahi CX-90SP II (Asahi Roentgen, Kyoto, Japan). Natural head position was determined by having the subjects look straight into a mirror in a standing position. A chain plumb line was suspended in front of the cassette to indicate a true vertical line. The MRI images were taken to evaluate TMJ status mainly because of TMJ symptoms including TMJ sounds, pain, masticatory muscle tenderness, limited mandibular movement, and locking. Exclusion criteria were (1) age less than 17 years, (2) any systemic disease, (3) history of orthodontic treatment, (4) history of facial cosmetic or orthognathic surgery, (5) history of trauma involving the TMJ, (6) juvenile rheumatoid arthritis, (7) history of TMJ treatment, (8) airway obstruction, (9) oral habits, (10) TMJ disc displacement of a greater severity on the unilateral side, and (11) partial TMJ disc displacement or TMJ disc displacement with partial reduction. This research protocol was approved by the institutional review board of the Seoul National University Dental Hospital (CRI11040).
Radiologists with MRI experience with the TMJ interpreted the images blinded to the clinical information. According to disc position, TMJ disc status was divided into 3 categories as follows.
- 1
Normal disc position. In the closed-mouth position, the intermediate zone of the disc was interposed between the condyle and the posterior slope of the articular eminence, with the anterior and posterior bands equally spaced on either side of the condylar load point.
- 2
Disc displacement with reduction. The disc was anteriorly displaced relative to the posterior slope of the articular eminence and the head of the condyle in the closed-mouth position, but the disc was reduced on mouth opening.
- 3
Disc displacement without reduction. The disc was anteriorly displaced relative to the posterior slope of the articular eminence and the head of the condyle, and the disc was not reduced on mouth opening.
The position and shape of the articular disc of the TMJ were carefully evaluated according to the classification criteria. We excluded patients with a unilaterally different disc displacement status because the possible skeletal morphologies associated with unilateral disc displacement would be obscured by averaging of the right and left landmarks used to determine their location, and unilaterally different disc displacement status may asymmetrically influence craniocervical posture or hyoid bone position, which is difficult to measure in lateral cephalometric analysis. From the originally selected patients, only those with bilateral normal disc status (BN), bilateral disc displacement with reduction (DDR), and bilateral disc displacement without reduction (DDNR) were included in this study.
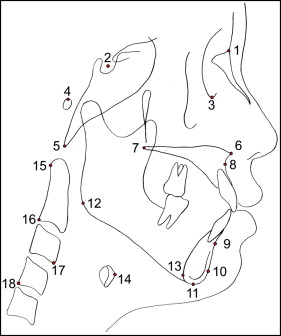
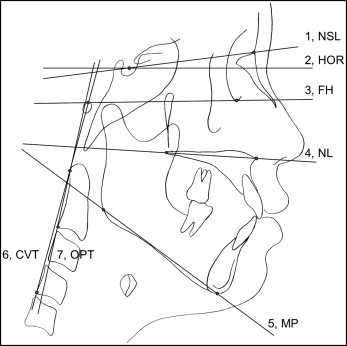
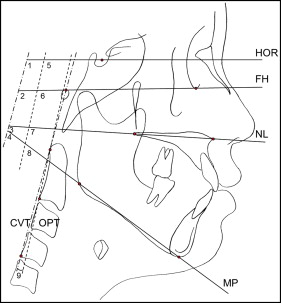
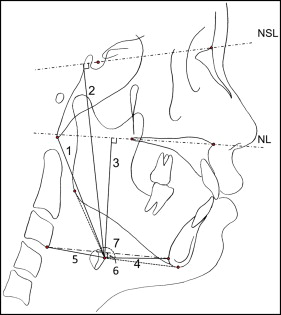
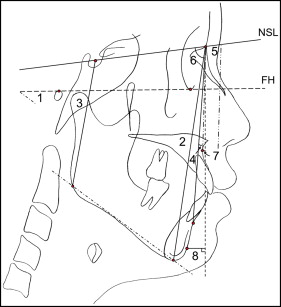
One investigator (S-J.A.), who was blinded to the clinical information and the disc position, traced all lateral cephalograms. Eighteen landmarks were recorded on each radiograph using a digitizer with a desktop computer, and 25 variables were calculated from these landmarks: 9 variables for craniocervical posture, 7 for hyoid bone position, and 9 for craniofacial morphology (4 for vertical and 5 for sagittal craniofacial morphologies). The positions and definitions of the landmarks are shown in Figure 1 , and the locations of the reference planes are shown in Figure 2 . Measurements for craniocervical posture, hyoid bone position, and craniofacial morphology are shown in Figures 3, 4 , and 5 , respectively.
Lateral cephalograms of 20 randomly selected subjects were measured again to test the magnitude of measurement errors. The intraclass correlation coefficients for the reliability of tracing, landmark identification, and analytic measurements were greater than 0.98.
Descriptive statistics were calculated for all variables. The differences in the cephalometric variables for craniocervical posture, hyoid bone position, and craniofacial morphology with respect to the TMJ disc displacement status (BN, DDR, and DDNR) were tested with 1-way analysis of variance. Scheffé multiple comparisons were performed at a significance level of 0.05 to analyze between-group relationships. To investigate the correlations between craniofacial morphology and craniocervical posture or hyoid bone position, Pearson correlation coefficients were calculated.
Results
A total of 170 female subjects were included in this study ( Table I ). Their age range was 17.0 to 50.8 years (mean age, 24.5 ± 5.7 years). There were no significant differences in age distribution among the 3 study groups (data not shown).
| Group | BN | DDR | DDNR | Total |
|---|---|---|---|---|
| Subjects, n (%) | 53 (31.2) | 55 (32.4) | 62 (36.5) | 170 (100) |
| Age (y) | ||||
| Mean | 23.7 ± 6.6 | 25.1 ± 5.4 | 24.6 ± 5.3 | 24.5 ± 5.7 |
| Range | 18.3-50.8 | 17.3-42.0 | 17.0-41.0 | 17.0-50.8 |
Table II presents the differences in craniocervical posture, hyoid bone position, and craniofacial morphology with respect to TMJ disc displacement status (BN, DDR, and DDNR). Significant differences were found in craniocervical posture between the BN and DDNR groups ( Table II ). Subjects with DDNR had larger angles between the craniofacial reference planes and the cervical vertebrae (FH/CVT, NL/CVT, FH/OPT, and NL/OPT) than did the subjects with BN, indicating that subjects with DDNR had extended craniocervical posture compared with those with BN. Although the subjects with DDR demonstrated intermediate values, there was no significant difference in craniocervical posture between the BN and DDR groups, or between the DDR and DDNR groups. Angles between the cervical vertebrae and the true horizontal plane (HOR/CVT and HOR/OPT) or the mandibular plane (MP/CVT and MP/OPT) were not significantly different among the 3 groups. Cervical curvature (OPT/CVT) also did not vary significantly among the different TMJ disc displacement groups.
| Variable | BN | DDR | DDNR | Significance ‡ | Multiple comparisons |
|---|---|---|---|---|---|
| Craniocervical posture | |||||
| HOR/CVT (°) | 98.7 ± 6.9 | 99.5 ± 5.8 | 99.6 ± 5.9 | NS | |
| FH/CVT (°) | 96.6 ± 8.2 | 98.3 ± 6.3 | 100.3 ± 7.1 | ∗ | BN <DDNR |
| NL/CVT (°) | 96.1 ± 8.7 | 98.3 ± 6.4 | 99.6 ± 6.9 | ∗ | BN <DDNR |
| MP/CVT (°) | 67.3 ± 8.8 | 67.6 ± 7.0 | 64.7 ± 8.5 | NS | |
| HOR/OPT (°) | 93.6 ± 7.4 | 94.9 ± 7.1 | 94.7 ± 6.4 | NS | |
| FH/OPT (°) | 91.5 ± 8.5 | 93.7 ± 7.3 | 95.4 ± 7.4 | ∗ | BN <DDNR |
| NL/OPT (°) | 91.0 ± 8.8 | 93.7 ± 7.2 | 94.7 ± 7.1 | ∗ | BN <DDNR |
| MP/OPT (°) | 62.2 ± 8.6 | 63.0 ± 7.9 | 59.8 ± 8.5 | NS | |
| OPT/CVT (°) | 5.1 ± 2.8 | 4.6 ± 2.9 | 4.9 ± 2.5 | NS | |
| Hyoid bone position | |||||
| Hy-Ba (mm) | 76.3 ± 5.6 | 77.0 ± 6.0 | 75.1 ± 6.1 | NS | |
| Hy to NSL (mm) | 107.0 ± 6.4 | 108.2 ± 7.6 | 108.4 ± 6.4 | NS | |
| Hy to NL (mm) | 60.7 ± 5.2 | 61.8 ± 6.0 | 62.6 ± 5.7 | NS | |
| Hy-RGn (mm) | 38.4 ± 5.7 | 35.5 ± 5.5 | 32.3 ± 5.5 | † | BN >DDR >DDNR |
| Hy-cv3ia (mm) | 36.2 ± 3.8 | 36.5 ± 3.0 | 35.2 ± 3.4 | NS | |
| Hy to cv3ia-RGn (mm) | −1.5 ± 6.1 | 0.0 ± 5.0 | 0.5 ± 5.9 | NS | |
| Go/Hy/Me (°) | 154.3 ± 18.0 | 151.0 ± 14.8 | 143.4 ± 15.1 | ∗ | BN = DDR >DDNR |
| Vertical craniofacial morphology | |||||
| FMA (°) | 28.9 ± 7.0 | 30.6 ± 6.7 | 35.5 ± 7.0 | † | BN = DDR <DDNR |
| FHR (ratio) | 0.63 ± 0.06 | 0.62 ± 0.05 | 0.59 ± 0.06 | † | BN = DDR >DDNR |
| AFH (mm) | 132.8 ± 5.5 | 133.7 ± 6.5 | 133.3 ± 6.0 | NS | |
| PFH (mm) | 83.7 ± 7.6 | 82.6 ± 6.6 | 77.9 ± 6.7 | † | BN = DDR >DDNR |
| Sagittal craniofacial morphology | |||||
| ANB (°) | 2.4 ± 4.5 | 5.1 ± 2.4 | 7.7 ± 2.8 | † | BN <DDR <DDNR |
| SNA (°) | 81.1 ± 3.1 | 81.6 ± 3.2 | 81.4 ± 2.8 | NS | |
| SNB (°) | 78.7 ± 4.9 | 76.5 ± 2.9 | 73.8 ± 3.6 | † | BN >DDR >DDNR |
| ANP (mm) | 1.7 ± 3.0 | 2.3 ± 2.8 | 1.5 ± 3.2 | NS | |
| PNP (mm) | −1.32 ± 10.43 | −6.32 ± 6.65 | −14.05 ± 7.73 | † | BN >DDR >DDNR |
‡ Scheffé multiple comparisons were used to analyze the intergroup difference at the level of α = 0.05.
Among the variables for hyoid bone position, only measurements related to the mandible were significantly influenced by TMJ disc displacement status. Subjects with DDNR had a decreased hyoid angle (Go/Hy/Me) compared with those with BN or DDR (BN = DDR > DDNR). In addition, the hyoidale to the most protrusive point of retrognathion distance (Hy-RGn) decreased as TMJ disc displacement status increased in severity from BN to DDNR (BN > DDR > DDNR). However, distances between craniocervical landmarks or reference planes and the hyoid bone (Hy-Ba, Hy to NSL, Hy to NL, Hy-cv3ia, and Hy to cv3ia-RGn) did not show significant differences according to TMJ disc displacement status ( Table II ).
As previously reported, subjects with TMJ disc displacement have a retrognathic mandible with a hyperdivergent skeletal pattern ( Table II ). Our study showed that increased ANB, and decreased SNB and N perpendicular to pogonion (PNP), are specific sagittal craniofacial morphologies in subjects with TMJ disc displacement. In addition, these skeletal characteristics became more severe as TMJ disc displacement progressed from BN to DDNR. However, variables representing maxillary position (SNA and N perpendicular to point A [ANP]) were not significantly different among the 3 groups. Subjects with DDNR had a hyperdivergent skeletal pattern: eg, increased Frankfort-mandibular plane angle (FMA), decreased posterior facial height (PFH), and decreased facial height ratio (FHR) compared with those with BN or DDR. In contrast to sagittal craniofacial morphology, vertical craniofacial morphology did not vary significantly between the BN and DDR groups ( Table II ).
Correlations between craniofacial morphology and craniocervical posture or hyoid bone position are presented in Table III . Generally, craniocervical posture (FH/CVT, NL/CVT, FH/OPT, and NL/OPT) was significantly correlated with variables representing sagittal (ANB, SNB, and PNP) and vertical (FMA and FHR) craniofacial morphologies, and subjects with extended craniocervical posture had a retrognathic mandible with a hyperdivergent skeletal pattern. However, cervical curvature (OPT/CVT) was not significantly correlated with craniofacial morphology.
| Variable | Correlation | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| FMA | FHR | AFH | PFH | ANB | SNA | SNB | ANP | PNP | |
| Craniocervical posture | |||||||||
| HOR/CVT (°) | 0.241 † | NS | 0.196 ∗ | NS | 0.240 † | −0.169* | −0.332 † | −0.153 ∗ | −0.334 † |
| FH/CVT (°) | 0.381 † | −0.247 † | 0.270 † | NS | 0.399 † | −0.205 † | −0.499 † | −0.316 † | −0.591 † |
| NL/CVT (°) | 0.256 † | −0.192 ∗ | 0.262 † | NS | 0.315 † | −0.248 † | −0.454 † | −0.193 ∗ | −0.416 † |
| MP/CVT (°) | −0.547 † | 0.556 † | NS | 0.512 † | NS | NS | NS | NS | NS |
| HOR/OPT (°) | 0.258 † | −0.154 ∗ | 0.153 ∗ | NS | 0.242 † | −0.168 ∗ | −0.333 † | NS | −0.325 † |
| FH/OPT (°) | 0.396 † | −0.256 † | 0.234 † | NS | 0.399 † | −0.207 † | −0.501 † | −0.290 † | −0.578 † |
| NL/OPT (°) | 0.283 † | −0.208 † | 0.231 † | NS | 0.326 † | −0.253 † | −0.467 † | −0.178 ∗ | −0.422 † |
| MP/OPT (°) | −0.498 † | 0.519 † | NS | 0.468 † | NS | NS | NS | NS | NS |
| OPT/CVT (°) | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Hyoid bone position | |||||||||
| Hy-Ba (mm) | NS | 0.152 ∗ | 0.247 † | 0.281 † | −0.162 ∗ | 0.162 ∗ | 0.257 † | NS | 0.174 ∗ |
| Hy to NSL (mm) | NS | NS | 0.341 † | 0.289 † | NS | 0.281 † | NS | NS | NS |
| Hy to NL (mm) | 0.237 † | NS | 0.247 † | NS | 0.236 † | NS | −0.161 ∗ | NS | −0.267 † |
| Hy-RGN (mm) | −0.519 † | 0.388 † | NS | 0.396 † | −0.584 † | NS | 0.421 † | NS | 0.562 † |
| Hy-cv3ia (mm) | −0.181 ∗ | 0.191 ∗ | 0.165 ∗ | 0.278 † | NS | NS | NS | NS | NS |
| Hy to cv3ia-RGn (mm) | NS | NS | NS | NS | 0.174 ∗ | NS | NS | NS | NS |
| Go/Hy/Me (°) | −0.385 † | 0.358 † | 0.168 ∗ | 0.447 † | −0.324 † | NS | 0.339 † | 0.151 ∗ | 0.367 † |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


