Introduction
The aim of this longitudinal 32-year follow-up investigation was to analyze the very long-term effects of Herbst treatment on the dentoskeletal structures. We followed 14 patients from a sample of 22 with Class II Division 1 malocclusions who were consecutively treated with the banded Herbst appliance at ages 12 to 14 years. The subjects were reexamined after therapy at the ages of 20 years (when the radius epiphysis/diaphysis plate was closed) and 46 years.
Methods
Lateral head films were analyzed from before (T1) and after (T2) treatment, and at 6 years (T3) and 32 years (T4) after treatment.
Results
(1) In the standard analysis (angular measurements) during the T2 to T3 period of 6 years, significant skeletal changes were the following: increase of the SNB (1.0°; P <0.01), decrease of the ANB (0.9°; P <0.01), and decrease of the ML/NSL (2.5°; P <0.001). During the T3 to T4 period of 24 years, no further significant angular changes occurred. (2) In the analysis of the sagittal changes in the occlusion (linear measurements) during the T2 to T3 period of 6 years, the mandible (6.1 mm; P <0.001) and the maxilla (3.0 mm; P <0.01) grew forward. During the T3 to T4 period of 24 years, the mandible (2.8 mm; P <0.01) and the maxilla (3.1 mm; P <0.01) continued to grow forward. Thus, during the total posttreatment (T2-T4) period of 32 years, there was continuous forward growth of the mandible (8.9 mm; P <0.001) and the maxilla (6.1 mm; P <0.001). (3) The analysis of superimposed lateral head films showed in all 14 subjects large amounts of sagittal and vertical skeletofacial growth during T3 to T4.
Conclusions
In all 14 subjects, large amounts of sagittal and vertical skeletofacial growth occurred after the age of 20 years. However, the question of when, during the period from 20 to 46 years, growth had come to an end remains open. Closure of the radius epiphysis/diaphysis plate is not useful as an indicator for completed skeletofacial growth. Our findings indicate the importance of considering late adult skeletofacial growth in dentofacial orthopedics, orthognathic surgery, and tooth implantology with respect to treatment timing, posttreatment retention, and relapse.
Highlights
- •
Sagittal and vertical skeletofacial growth occurs after the age of 20 years.
- •
Closure of the radius epiphysis/diaphysis plate does not mean that skeletal growth has ended.
- •
Late adult skeletofacial growth should be considered when planning treatment.
In adolescent patients with Class II malocclusions treated with the Herbst appliance, to date there are only 6 roentgenographic cephalometric studies dealing with follow-up data after therapy exceeding 2 years. Because in those studies the follow-up periods ended in late adolescence or early adulthood (approximately age 20 years), any persisting dentoskeletal growth could affect the long-term outcome of treatment.
In a recent longitudinal biometric 32-year follow-up investigation using dental casts, the very long-term effects after Herbst therapy on tooth position and occlusion were analyzed in 14 adolescents with Class II Division 1 malocclusions who were followed to middle life (average, 46 years). After the total follow-up period of 32 years, 64% of the patients had results that were overall successful. A partial Class II relapse was noted in 29%, and a total relapse in 7% of the subjects. Thus, it would be of utmost interest to verify any possible posttreatment adult skeletofacial growth after age 20 and its possible impact on the long-term treatment outcome.
Therefore, the aim of this cephalometric roentgenographic follow-up investigation after Herbst therapy was to analyze the long-term (32 years) dentoskeletal changes in the these subjects investigated biometrically. The specific aims were to (1) assess the amounts of skeletal and dental components contributing to changes in the occlusion, (2) evaluate and compare early posttreatment changes of 6 years (ages,14-20 years) and late posttreatment changes of 26 years (ages, 20-46 years), and (3) visualize the long-term skeletofacial growth changes with superimposed lateral head films.
Material and methods
The subjects in this study were derived from a well-defined sample of 22 consecutive patients with Class II Division 1 malocclusions (bilateral Class II molar and canine occlusion, large overjet, and deep overbite) treated with the Herbst appliance at the University of Malmö in Sweden in 1977 and 1978. The subjects were originally presented in 2 articles from 1982.
In 2011 and 2012, 30 to 33 years after Herbst therapy, these 22 subjects were recalled to the orthodontic department in Malmö, Sweden, for a follow-up investigation. At this time, they were 42 to 48 years old. Two persons were deceased, and 6 did not appear for several reasons. Thus, the final follow-up sample comprised 14 subjects (12 men, 2 women), shown in detail in Table I . The patients’ ages were, on average, 12 years at the start of treatment and 14 years after treatment. The patients were reexamined 6 years (age 20) and 32 years (age 46) after treatment.
| Patient | Sex | Treatment | Age (y) | Follow-up periods (y) | Retention | Class II correction | Growth pattern | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Herbst/Extraction | T1 | T2 | T3 | T4 | T2 -T3 | T3-T4 | T2-T4 | Fixed/Removable † | Stable/Relapse | Horizontal/Vertical ‡ | ||
| 1X | m | Herbst/extraction | 13 | 17 ∗ | 21 | 48 | 4 | 27 | 31 | F/R (2 y) | Stable | V |
| 2 | m | Herbst | 13 | 14.5 | 20.5 | 48 | 6 | 27.5 | 33.5 | No retention | Stable | H |
| 3 | m | Herbst | 11 | 12.5 | 19 | 45 | 6.5 | 26 | 32.5 | No retention | Stable | H |
| 4 | m | Herbst | 13 | 14.5 | 20.5 | 47.5 | 6 | 27 | 33 | R (4 y) | Stable | H |
| 5 | m | Herbst | 13.5 | 15 | 19 | 46.5 | 4 | 27.5 | 31.5 | R (3 y) | Relapse | H |
| 6 | m | Herbst | 13 | 14.5 | 20.5 | 47.5 | 6 | 27 | 33 | No retention | Relapse | H |
| 7 | f | Herbst | 13 | 14.5 | 20.5 | 48 | 6 | 27.5 | 33.5 | R (2 y) | Stable | H |
| 8X | m | Herbst/extraction | 13 | 15 | 22 | 48 | 7 | 26 | 33 | F/R (4 y) | Stable | H |
| 9 | m | Herbst | 12.5 | 14 | 20 | 45 | 6 | 25 | 31 | R (2 y) | Stable | V |
| 10 | m | Herbst | 12 | 14 | 20 | 44 | 6 | 24 | 30 | No retention | Stable | H |
| 11 | f | Herbst | 11 | 12.5 | 18.5 | 42.5 | 6 | 24 | 30 | R (2 y) | Stable | V |
| 12 | m | Herbst | 12.5 | 14 | 21 | 46 | 7 | 25 | 32 | F/R (3 y) | Relapse (1 side) | H |
| 13 | m | Herbst | 12.5 | 14 | 21 | 45 | 7 | 24 | 31 | R (2 y) | Relapse | H |
| 14 | m | Herbst | 12.5 | 14 | 22 | 45 | 8 | 23 | 31 | R (2 y) | Relapse (1 side) | H |
| Summary | 12 men | 12 Herbst | 12.5 | 14.3 | 20.4 | 46.1 | 6.1 | 25.7 | 31.8 | 4 no retention | 9 stable | 11 H |
| Mean | 2 women | 2 Herbst/extraction | 10 retention | 5 relapse | 3 V | |||||||
∗ Includes a 2-year break in treatment during the period T1-T2.
† F implies fixed retention with a mandibular lingual canine-to-canine retainer; R implies removable retention with an activator or a maxillary Hawley plate; F/R implies a fixed mandibular canine retainer in combination with a removable maxillary Hawley plate.
‡ H , Horizontal growth pattern that implies a reduction of the mandibular plane angle during T1-T4; V , vertical growth pattern that implies an increase of the mandibular plane angle during T1-T4.
All subjects were treated by an author (H.P.) using a banded type of Herbst appliance with a simple anchorage system that did not include brackets on any teeth. Since the treatment of the original 22-subject sample was designed as a clinical experimental study, no further fixed appliance treatment phase after the Herbst phase was planned. However, because of major tooth irregularities after Herbst therapy, extractions of 4 premolars were performed in 2 subjects (patients 1X and 8X), and maxillary and mandibular fixed multibracket appliances were placed for about 1 year. Furthermore, for tooth alignment in 1 nonextraction patient (12), a maxillary multibracket appliance treatment phase was instituted for 6 months after the Herbst phase. In these 3 patients, multibracket treatment after the Herbst phase aimed to align the teeth after the Class I dental arch and overjet corrections were achieved by the Herbst appliance.
Retention after Herbst treatment, performed in 10 of the 14 patients, was inconsistent and of short duration (2-4 years). No retainers were used in 4 subjects ( Table I ).
Lateral head films were analyzed at 4 times: T1, before Herbst treatment; T2, after treatment (12 months after the Herbst appliance was removed and the occlusion had settled); for the 2 extraction patients (1X and 8X), T2 implied that analyses were done after removal of the multibracket appliance; T3, 6 years after treatment at an average age of 20 years when the radius epiphysis/diaphysis plate was closed (hand-wrist stage R-J, according to Hägg and Taranger ); and T4, 32 years after treatment at an average age of 46 years.
The treatment and posttreatment changes of different variables were analyzed during the following observation periods: T1-T2, treatment changes; T2-T3, early posttreatment changes; T3-T4, late posttreatment changes; and T2-T4, total posttreatment changes.
All cephalometric roentgenograms were taken at the Department of Oral Radiology, Faculty of Dentistry, Malmö University, Malmö, Sweden. The lateral head films at T1, T2, and T3 were taken by the analog technique and the films at T4 by the digital technique. For each technique, the radiographic records were obtained using a standardized procedure with a fixed-focus midsagittal film distance. For accomplishing the same magnification of all head films, the printouts of the T4 images were reduced in size by 14% to match the T1, T2, and T3 images (7%). With the help of 1-mm metal indicators placed at intervals of 5 mm in the center of the cephalostat’s forehead rest, the final radiographic magnification could be checked.
The measurements from the roentgenograms were performed on matte acetate tracing film, on which the reference points were marked with a sharp pencil. The angular measurements were made to the nearest 0.5°, and the linear measurements to the nearest 0.5 mm. These values were not corrected for linear enlargement (7%) in the median plane.
The reference points and lines used in the cephalometric analysis were those defined by Björk and Pancherz.
To minimize the tracing and landmark identification errors in the analysis of the serial head films, the tracings of the 4 head films from each patient were done in a simultaneous parallel way at the same occasion.
The head film evaluations comprised a standard analysis and an analysis of the sagittal changes in the occlusion (SO).
The head film analysis comprised 7 angular measurements (variables 1-7) and 2 linear measurements, the latter of which were made on dental casts (variables 8 and 9).
- 1.
SNA, sagittal maxillary position to the cranial base.
- 2.
SNB, sagittal mandibular position to the cranial base.
- 3.
ANB, sagittal maxillomandibular relationship.
- 4.
ML/NSL, vertical mandibular position to the cranial base (mandibular plane angle).
- 5.
ILs/NSL, maxillary incisor inclination to the cranial base.
- 6.
ILi/ML, mandibular incisor inclination to the mandibular plane.
- 7.
ILs/ILi, interincisal inclination.
- 8.
Overjet, the horizontal distance between the incisal edge of the most prominent maxillary central incisor and the labial surface of the corresponding mandibular incisor parallel to the occlusal plane.
- 9.
Overbite, the vertical distance between the incisal edges of the maxillary central and mandibular central incisors.
The SO analysis has been described extensively in a previous article. The SO analysis allows a quantitative assessment of skeletal and dental changes in the maxilla and mandible that contribute to changes in the sagittal molar relationship and overjet.
The reference points and lines used are shown in Figure 1 . The occlusal line (OL) is defined by the incisal tip of the most prominent maxillary central incisor and the mesiobuccal cusp tip of the first maxillary molar. The OLp is a line perpendicular to OL through the tangent point of the anterior wall of sella turcica. The OL and the OLp from the first head film were used as a reference grid. The grid was transferred from the T1 tracing to the following tracings (T2, T3, and T4) by superimposition of the radiographs, using the stable skull structures in the anterior cranial base for orientation. The objective was to obtain the closest coincidence for the maximum number of the following structures: (1) the anterior wall of sella turcica, (2) the cribriform plate, (3) the trabecular pattern of the superior portion of the ethmoid bone, (4) the medial border of the orbital roof, (5) the anterior walls of the median cranial fossae, and (6) the anterior contours of the pterygopalatine fossae.
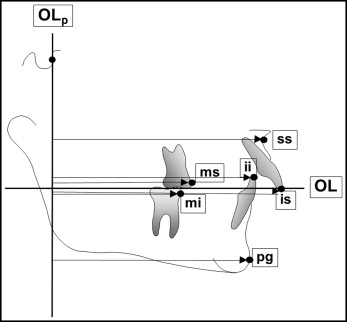
Perpendicular to the OLp line, the following changes in linear measurements ( Fig 1 ) were assessed (variables 1-8): (1) ms minus mi, molar relationship; (2) is minus ii, overjet; (3) ss, maxillary base position; (4) pg, mandibular base position; (5) ms minus ss, maxillary molar position; (6) mi minus pg, mandibular molar position; (7) is minus ss, maxillary incisor position; and (8) ii minus pg, mandibular incisor position.
To visualize the dentoskeletal growth changes during the different observation periods, the radiographs from T1, T2, T3, and T4 of each subject were superimposed using the stable anterior cranial base structures for orientation.
Statistical analysis
The data generated from the head film measurements were imported to the SPSS software package (version 20.0; IBM, Armonk, NY) for statistical analysis.
The arithmetic means and standard deviations were calculated. Because all variables were normally distributed, as shown by the Kolmogorov-Smirnov test, paired t tests were used to assess the statistical significance of changes during the different observation periods. The levels of significance used were P <0.001, P <0.01, and P <0.05. P ≥0.05 was considered not significant.
Because of the small sample size of 14 subjects, no correlation or multiple regression analysis was performed.
The study was approved by the ethical committee of the University of Malmö in Sweden (number 2012/44).
Results
All head film registrations from the 14 subjects were performed twice. The precision of the double registrations was tested with Dahlberg’s formula with a 2-week interval. For the angular measurements, the method error varied between 0.6° (SNA, SNB) and 1.1° (ILs/NSL). For the linear measurements, the error ranged between 0.2 mm (pg-OLp) and 0.5 mm (mi-OLp).
The final results were based on the first series of head film measurements.
For the standard cephalometric evaluation for each variable, the arithmetic mean and standard deviation at each examination as well as the statistical evaluation of changes during the different examination periods are given in Table II .
| Variable | T1 | T2 | T3 | T4 | T1-T2 | T2-T3 | T3-T4 | T2-T4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | t ∗ | P | t ∗ | P | t ∗ | P | t ∗ | P | |
| SN-maxillary position (°) | 82.8 | 4.15 | 82.2 | 4.56 | 82.3 | 4.58 | 81.5 | 5.25 | 0.97 | NS | −0.29 | NS | 1.15 | NS | 0.90 | NS |
| SNB-mandibular position (°) | 77.0 | 3.61 | 76.9 | 4.02 | 77.9 | 3.52 | 77.4 | 4.72 | 0.08 | NS | −3.61 | <0.01 | 0.87 | NS | −0.79 | NS |
| ANB-maxillomandibular relationship (°) | 5.9 | 2.02 | 5.3 | 1.85 | 4.4 | 2.39 | 4.4 | 1.86 | 2.18 | <0.05 | 3.10 | <0.01 | 0.00 | NS | 1.94 | NS |
| ML/NSL-mandibular plane angle (°) | 30.1 | 5.72 | 30.5 | 6.71 | 28.0 | 6.53 | 28.0 | 7.23 | −0.53 | NS | 6.15 | <0.001 | 0.06 | NS | 3.93 | <0.01 |
| ILs/NSL-maxillary incisor inclination (°) | 101.9 | 4.73 | 96.5 | 7.94 | 98.0 | 6.81 | 97.8 | 6.76 | 3.36 | <0.01 | −1.21 | NS | 0.22 | NS | −0.83 | NS |
| ILi/ML-mandibular incisor inclination (°) | 100.1 | 6.25 | 104.2 | 5.33 | 101.1 | 4.59 | 101.7 | 6.29 | −4.59 | <0.001 | 4.07 | <0.001 | −0.54 | NS | 1.98 | NS |
| ILs/Ili-interincisor inclination (°) | 128.0 | 8.13 | 131.1 | 7.15 | 133.3 | 9.72 | 132.9 | 9.40 | −1.88 | NS | −1.06 | NS | 0.20 | NS | −0.79 | NS |
| Overjet (mm) † | 8.1 | 1.62 | 3.9 | 0.89 | 4.0 | 1.13 | 4.2 | 1.67 | 7.23 | <0.001 | −0.31 | NS | −0.72 | NS | −0.67 | NS |
| Overbite (mm) † | 5.0 | 1.23 | 3.5 | 1.06 | 3.8 | 0.78 | 3.8 | 0.83 | 3.20 | <0.01 | −0.74 | NS | −1.00 | NS | −0.36 | NS |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


