Practice Note
Infectious diseases can be transmitted by a number of media during dental treatment, including blood, saliva, nasal discharge, dust, hands, clothing, and hair.
Types of Infections
Infections common to dental treatment generally can be divided into two categories: autogenous infections and cross-infections. Autogenous infections are infections for which the patient is the source. For example, a patient who undergoes dental treatment, such as an extensive scaling procedure, may subsequently develop endocarditis; this condition can result from the introduction of virulent organisms (e.g., staphylococci, pneumococci) that live in the mouth into the bloodstream during the scaling procedure.
Cross-infections are transferred from one patient or person to another. For example, when a child has an infection and coughs or sneezes, the caregiver may contract the infection through airborne or droplet transmission.
Routes of Infection Transmission
Microbial transmission through dental-related secretions and exudates occurs by three general routes: (1) direct contact with a lesion, organisms, or debris during an intraoral procedure; (2) indirect contact through contaminated dental instruments, equipment, or records; and (3) the inhalation of microorganisms aerosolized from a patient’s blood or saliva during the use of high-speed or ultrasonic equipment, such as a high-speed handpiece or an ultrasonic scaler.
In many dental practices, treatment providers may not realize the dissemination potential of saliva and blood by these routes. Potential dangers often are missed because much of the spatter from the patient’s mouth is not readily noticeable. For example, bioburden (i.e., blood, saliva, and exudate) may be transparent; it may dry as a clear film on contaminated surfaces. Consequently, the administrative assistant must understand the potential risk of handling contaminated items and touching contaminated surfaces.
Infection Control in the Dental Office
Because patient care actually begins in the business office, it is important to identify the role of the administrative assistant as it relates to infection control in the clinical area. Every dental healthcare worker is responsible for breaking the cycle of disease transmission (Figure 17-1). Safe practice is based on the following principles:
The administrative assistant is responsible for the first step in safe practice: obtaining complete and detailed information about the patient. The records discussed in Chapter 7 must be completed, dated, signed, and reviewed thoroughly by the dentist. During treatment procedures, the administrative assistant must make sure that protocols are followed and that the necessary barrier materials are available for use. Finally, the administrative assistant ensures that the records used during the treatment procedure are transferred safely from the clinical site to the business office without cross-contamination.
Table 17-2 presents several situations that the administrative assistant may encounter when attempting to maintain safe practice in the office. The administrative assistant must be able to distinguish between right actions and wrong actions, and he or she must understand the consequences of a wrong action in infection control. Box 17-1 presents a self-assessing list of points that the administrative assistant should live by when working in the dental office to make sure that disease transmission is not being promoted.
TABLE 17-2
Recognizing Wrong from Right in Infection Control
| Wrong | Effect | Right |
| Shaking hands while wearing contaminated gloves | Disease transmission may occur via cross-contamination. | Remove gloves and wash hands before leaving examination gloves in treatment room; nod and greet the individual. |
| Pulling mask on and off | Contact with the face with contaminated gloves can expose unprotected tissues to disease; if the mask is contaminated, contact with gloved or ungloved hands will also allow disease transmission. | Always leave mask in place; if movement for repositioning is necessary, do it with clean gloves; slight readjustment may be made by using the upper arm or shoulder. |
| Wearing the same mask for more than one patient | Masks become moist fields, which allow for the penetration of particles through the mask. | Always change masks between patients; use more than one mask if the treatment procedure is lengthy. |
| Reusing the same gloves | Most gloves have microscopic openings that allow for the penetration of microbes; washing gloves increases the potential for disease transmission. | Gloves are always changed between patients; gloves may need to be changed during a lengthy treatment procedure. |
| Placing patient records in the treatment room | Records may become exposed to aerosols or through handling; these records are transferred to the business office after treatment, thereby exposing the business personnel to the potential for disease. | Records other than radiographs should be kept outside of the treatment room to avoid contamination; if the records must be in the treatment room, they should be kept out of reach of aerosols and handled with clean hands or with overgloves rather than examination gloves. |
| Storing instruments in trays or drawers instead of sealed bags in treatment rooms | Instruments that are not individually bagged (if not part of a tray setup) may be exposed to aerosols or other contact during treatment and may become contaminated. | All instruments processed through sterilization should be bagged to ensure their sterility when they are used; even in closed drawers, instruments may not remain sterile. |
| Eating in the laboratory or in another contaminated site | Surfaces can become contaminated from instruments or materials exposed to patient aerosols or handling. | A staff lounge or eating area must be available in a site away from potentially contaminated materials. |
| Wearing a V-neck laboratory coat | Garments worn under the lab coat can become contaminated; if wearing a V-neck shirt underneath such a coat, the skin will be exposed. | Always wear high-neck lab coats when working with patients or in the laboratory; these coats should be removed before leaving the workplace. |
| Wearing dangling earrings, piercings, necklaces, bracelets, or ties | These items can become contaminated; they may hang in the patient’s face or catch on something. | Minimize jewelry; only wear wedding bands and small post earrings in the workplace. |
Occupational Health Protection Program for the Dental Staff
The administrative assistant plays a role in maintaining the health and safety of the patients and healthcare workers in the office. Although he or she is not usually assigned the task of infection control coordinator, he or she should be familiar with the aspects of this process. After all, the administrative assistant is responsible for managing the office and thus must be able to access all records.
The office’s personnel policy must include a health service program for the staff that covers the following:
The administrative assistant and the dentist must work together to maintain the safety of all staff members and patients. Attention to records maintenance and continual education and training can ensure safe practice.
Government Regulations
All dental professionals are expected to comply with the current guidelines and regulations that govern infection control, hazard communication, and medical waste disposal. Several agencies are responsible for providing the dental professional with the current regulations that affect each of these areas. The employer is primarily responsible for maintaining current copies of all state and federal regulations that relate to the dental office. These guidelines must be reviewed, and their implementation in the office must be documented.
OSHA established guidelines to protect workers from occupational exposure to blood-borne diseases. Regulations now require that employees who come in direct contact with blood or infectious materials and substances are required to use standard precautions. In other words, all patients must be treated as if they are potentially infectious with the human immunodeficiency virus (HIV), the hepatitis B virus (HBV), the hepatitis C virus (HCV), and other infectious organisms. An overview of the latest required OSHA standards is presented in Box 17-2.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Practice Note
Practice Note Practice Note
Practice Note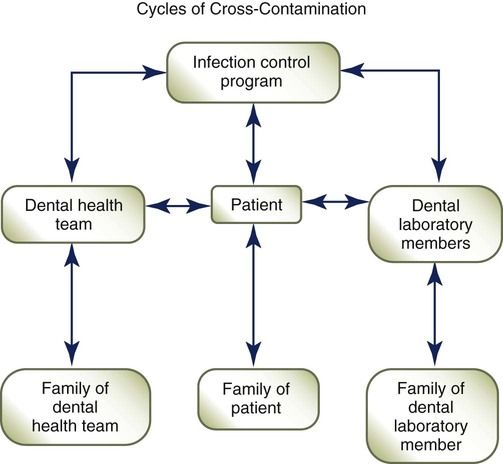
 Practice Note
Practice Note