Introduction
The objective of this 2-arm parallel single-center trial was to compare placement time and numbers of failures of mandibular lingual retainers bonded with an indirect procedure vs a direct bonding procedure.
Methods
Sixty-four consecutive patients at the postgraduate orthodontic clinic of the University of Geneva in Switzerland scheduled for debonding and mandibular fixed retainer placement were randomly allocated to either an indirect bonding procedure or a traditional direct bonding procedure. Eligibility criteria were the presence of the 4 mandibular incisors and the 2 mandibular canines, and no active caries, restorations, fractures, or periodontal disease of these teeth. The patients were randomized in blocks of 4; the randomization sequence was generated using an online randomization service ( www.randomization.com ). Allocation concealment was secured by contacting the sequence generator for treatment assignment; blinding was possible for outcome assessment only. Bonding time was measured for each procedure. Unpaired t tests were used to assess differences in time. Patients were recalled at 1, 2, 4, and 6 months after bonding. Mandibular fixed retainers having at least 1 composite pad debonded were considered as failures. The log-rank test was used to compare the Kaplan-Meier survival curves of both procedures. A test of proportion was applied to compare the failures at 6 months between the treatment groups.
Results
Sixty-four patients were randomized in a 1:1 ratio. One patient dropped out at baseline after the bonding procedure, and 3 patients did not attend the recalls at 4 and 6 months. Bonding time was significantly shorter for the indirect procedure (321 ± 31 seconds, mean ± SD) than for the direct procedure (401 ± 40 seconds) (per protocol analysis of 63 patients: mean difference = 80 seconds; 95% CI = 62.4-98.1; P <0.001). The 6-month numbers of failures were 10 of 31 (32%) with the indirect technique and 7 of 29 (24%) with the direct technique (log rank: P = 0.35; test of proportions: risk difference = 0.08; 95% CI = −0.15 to 0.31; P = 0.49). No serious harm was observed except for plaque accumulation.
Conclusions
Indirect bonding was statistically significantly faster than direct bonding, with both techniques showing similar risks of failure.
Registration
This trial was not registered.
Protocol
The protocol was not published before trial commencement.
Funding
No funding or conflict of interest to be declared.
Highlights
- •
Indirect bonding of lower fixed retainers is 20% faster than direct bonding.
- •
Both bonding techniques seem to have a similar failure risk.
- •
Failures are more frequent during the first month in both groups.
Long-term maintenance of orthodontic outcomes is important, and fixed retention is a common approach for preserving stability after treatment, especially in the mandibular anterior region. Undesirable tooth movement occurs in subjects with and without previous orthodontic treatment as a physiologic result of aging. Therefore, fixed retention seems to be a good means to ensure stability of the aligned anterior dentition after orthodontic treatment.
Bonding a stainless steel wire segment on the lingual surfaces of anterior teeth, generally from canine to canine in the mandibular arch, is an accepted method for long-term retention. If the patient has adequate oral hygiene, fixed retainers have the advantage of being an effective solution that requires minimum compliance. However, bonding a fixed retainer requires more chair time than placing a removable retainer, and bond failure or archwire fracture can have detrimental consequences. Chair time and reliability are therefore important parameters that weigh on the retention protocol decision.
There are different bonding techniques to place a fixed retainer. The most common technique is the direct bonding procedure where the composite pads are directly placed in the patient’s mouth, with or without prebending of the wire by a laboratory technician. The indirect bonding technique was proposed in the late 1990s as a faster alternative to the direct bonding procedure. Indirect bonding requires preparation of the composite pads on the cast of the patient.
Many studies have investigated the survival of lingual retainers. Previously reported failure risks correspond mainly to the direct bonding method and vary between 11% and 50%. Risks of failure differ in these studies according to the materials used to fabricate the lingual retainer, the bonding sites of the retainer (on the canines only or on all 6 anterior teeth), and the duration of the follow-up. Failures are more frequently observed during the first 6 months after bonding.
Indirect bonding is considered faster by many clinicians, although there is no evidence to support this belief. One study compared the numbers of failures with indirect and direct bonding of orthodontic retainers and concluded that there was no statistically significant difference. Moreover, no systematic review has evaluated this issue.
Therefore, the main aim of this randomized controlled trial was to investigate whether the time needed for indirect bonding of a mandibular fixed retainer is shorter than the time needed for direct bonding. A secondary outcome was to compare the risks of failure of both techniques after a 6-month period.
Specific hypotheses
Our hypotheses were thus the following: (1) the time needed for indirect bonding of a mandibular fixed retainer is shorter than the time needed for direct bonding, and (2) there is no difference in failures between the 2 bonding methods.
Methods
Trial design
This was a single-center 2-arm parallel randomized controlled trial with a 1:1 allocation ratio.
Participants, eligibility criteria, and settings
Consecutive patients who had completed their orthodontic treatment at the postgraduate orthodontic clinic of the University of Geneva from mid-September 2012 until the end of June 2013 were invited to participate. Data were collected from mid-September 2012 until the end of December 2013. The inclusion criteria were the presence of the 4 mandibular incisors and the 2 mandibular canines, and no active caries, restorations, fractures, or periodontal disease of these teeth. The patients were informed about the study both orally and with an information leaflet. Each patient (or a parent in case of a minor patient) was asked to sign an informed consent before the bonding of the mandibular fixed retainer. One operator (E.B.) bonded all the mandibular fixed retainers. This study was approved by the Ethical Committee of Research of the Human Being at the University of Geneva (reference number: 12-198/psy12-020).
Interventions
The terms “indirect” and “direct” used in this article refer to the bonding techniques and not to the chairside vs laboratory fabrications of the wires.
The intervention protocol was the following.
- 1.
Alginate impression of the mandibular arch.
- 2.
Construction, by the same laboratory technician, of the mandibular fixed retainer using a round 0.0215-in multistrand stainless steel wire (Penta One; Masel, Philadelphia, Pa) passively adapted to the lingual surfaces of the incisors and canines on the plaster model.
- a.
For the direct bonding group
-
A silicone key was constructed on the central incisors to ensure the correct position of the wire during bonding. No composite was applied at this stage ( Fig 1 ).
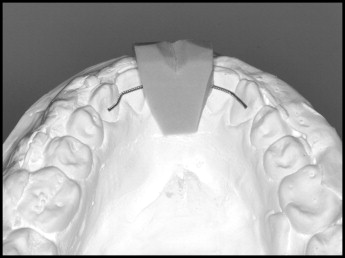
Fig 1 Plaster model with retention wire and silicon transfer key for direct bonding. - b.
For the indirect bonding group
-
Separation liquid was placed on the lingual surface of the mandibular teeth of the plaster model. The lower retainer, previously adapted on the model, was subsequently bonded in the predetermined position on each tooth with Transbond LR Light Cure Adhesive (3M, Monrovia, Calif) and polymerized for 12 seconds per tooth. Finally, a silicone tray was constructed from canine to canine, covering the retainer and the composite pads to allow for indirect bonding ( Fig 2 ).
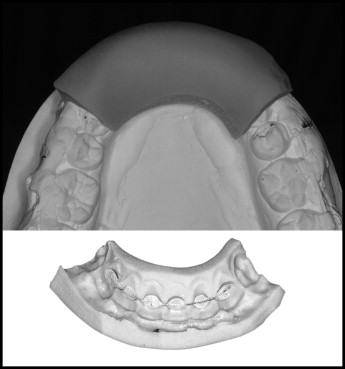
Fig 2 Silicon transfer tray containing retention wire and polymerized composite pads for indirect bonding.
- a.
- 3.
Bonding of the retainer.
-
A chronometer was used to calculate the time for every bonding procedure subsequently described. Lingual surfaces were pumiced and etched with 35% phosphoric acid for 30 seconds.
- a.
For the direct bonding group
-
The retainer was checked for passivity on the lateral incisors and canines. Transbond XT Primer (3M) was applied on the lingual surfaces of the canines and whiffed with the air syringe. The fixed retainer was transferred from the plaster model to the dental arch with the silicone key. The fixed retainer was bonded on both canines with Transbond LR Light Cure Adhesive. The silicone key was removed, and the central and lateral incisors were bonded with the same product. Light curing was performed for 12 seconds per tooth using a light-emitting diode curing light (Mini LED Ortho 2; Satelec, Merignac Cedex, France).
- b.
For the indirect bonding group
-
Before bonding the retainer, acetone was applied on the composite pads. Once these surfaces were dry, Maximum Cure A and B liquid adhesives (Reliance, Itasca, Ill) were mixed and applied on both the lingual surfaces of the teeth and the composite pads of the retainer. The silicone tray containing the retainer was subsequently placed in the mouth under light pressure. The silicone tray was removed after chemopolymerization was considered complete (90 seconds). If bonding failure of a composite pad occurred after removal of the tray, the composite pad was removed and replaced with the direct bonding technique after preparation of the enamel surface.
- a.
Outcomes and any changes after trial commencement
The primary outcome of this study was the time needed for bonding mandibular lingual retainers with either the indirect or the direct bonding technique. The secondary outcome was the number of failures at any time (including right after bonding at 0 days) of each technique.
The patients were followed-up at approximately 1, 2, 4, and 6 months after bonding to detect breakage or debonding of the mandibular fixed retainer. Retainers having at least 1 composite pad debonded were considered as failures.
Sample size calculation
The sample size was calculated for the primary outcome, bonding time. A pilot study was performed to estimate the average bonding times and standard deviations with both the direct (20 patients) and the indirect (16 patients) techniques. To detect a difference of 70 seconds between groups, corresponding to a 15% time saving for the direct technique (on average, 458 seconds during the pilot study) and with a standard deviation of 45 seconds, 29 patients were needed per group (α = 0.1%; power [1−β] = 99%). We decided to enroll 32 patients per group to compensate for possible dropouts.
Interim analyses and stopping guidelines
Not applicable.
Randomization
Enrolled patients were randomized in blocks of 4 (sequence generated on the Web site www.randomization.com by an author [M.A.C.]) to either the direct bonding technique group or the indirect bonding technique group. To ensure allocation concealment, the sequence generator communicated daily with the operator about which consecutive scheduled patients of the day should be assigned to either group.
Blinding
Blinding of neither patient nor operator was not possible in this study. Blinding of the outcome assessor (E.B.) was performed by assigning a number to each patient and evaluating the data without having access to the actual patients’ names.
Statistical analysis
Independent t tests were used to compare bonding times between the 2 groups. The log-rank test was used to compare the Kaplan-Meier survival curves of the 2 techniques. A test of proportion was applied to compare the failures at 6 months between the treatment groups. The data were analyzed using SPSS software (version 21; IBM, Armonk, NY).
Methods
Trial design
This was a single-center 2-arm parallel randomized controlled trial with a 1:1 allocation ratio.
Participants, eligibility criteria, and settings
Consecutive patients who had completed their orthodontic treatment at the postgraduate orthodontic clinic of the University of Geneva from mid-September 2012 until the end of June 2013 were invited to participate. Data were collected from mid-September 2012 until the end of December 2013. The inclusion criteria were the presence of the 4 mandibular incisors and the 2 mandibular canines, and no active caries, restorations, fractures, or periodontal disease of these teeth. The patients were informed about the study both orally and with an information leaflet. Each patient (or a parent in case of a minor patient) was asked to sign an informed consent before the bonding of the mandibular fixed retainer. One operator (E.B.) bonded all the mandibular fixed retainers. This study was approved by the Ethical Committee of Research of the Human Being at the University of Geneva (reference number: 12-198/psy12-020).
Interventions
The terms “indirect” and “direct” used in this article refer to the bonding techniques and not to the chairside vs laboratory fabrications of the wires.
The intervention protocol was the following.
- 1.
Alginate impression of the mandibular arch.
- 2.
Construction, by the same laboratory technician, of the mandibular fixed retainer using a round 0.0215-in multistrand stainless steel wire (Penta One; Masel, Philadelphia, Pa) passively adapted to the lingual surfaces of the incisors and canines on the plaster model.
- a.
For the direct bonding group
-
A silicone key was constructed on the central incisors to ensure the correct position of the wire during bonding. No composite was applied at this stage ( Fig 1 ).
- a.




