Introduction
Dental caries, specifically decalcified white-spot lesions (WSL), is a well-known side-effect of orthodontic treatment. The incidence of labial incipient caries lesions and its relationship with various patient and treatment variables was investigated in patients treated with comprehensive orthodontics.
Methods
Randomly selected orthodontic patient records (n = 350) were examined to determine incipient caries lesion development. Labial surfaces on pretreatment and posttreatment photographs were scored with a standardized scoring system. Independent variables were collected by chart abstraction.
Results
The incidence of patients who developed at least 1 new WSL during treatment was 72.9%, and this incidence was 2.3% for cavitated lesions. Treatment duration was significantly associated with new WSL development ( P = 0.03). Development of WSL and cavitated lesions increased (both, P <0.00) despite increased attention to oral hygiene during treatment. Sex, age, extraction therapy, and various fluoridation sources were not associated with WSL development, but initial oral-hygiene score was moderately associated ( P <0.06).
Conclusions
The incidence of WSL in patients treated with comprehensive orthodontics was significantly high, and the preventive therapy provided appeared to be ineffective. This widespread problem is alarming and warrants significant attention from both patients and providers that should result in greatly increased emphasis on effective caries prevention.
Orthodontic patients can find it difficult to maintain adequate oral hygiene around fixed appliances. The decline in oral hygiene that often accompanies orthodontic treatment might lead to an increased risk for development of caries lesions. The severity of the resultant dental caries can range from development of opaque white-spot lesions (WSL), or decalcification, to loss of surface integrity of enamel and cavitation.
A classic WSL study demonstrated that 49.6% of orthodontic patients exhibited enamel opacities on at least 1 tooth after orthodontic treatment. Prevalence values of individual teeth with posttreatment white spots were 10.8% for bonded teeth and 12.0% for banded teeth. Significant increases in both prevalence and severity of enamel opacities following orthodontic treatment were reported. The prevalence of posttreatment WSL in orthodontic patients was reported to be 84%, compared with 72.3% at pretreatment. This increased prevalence of enamel lesions caused by orthodontic treatment lasted for 5 years or more after appliance removal. More recently, 95.3% of a group of orthodontically treated patients experienced development of at least 1 new WSL or an increase in severity of an existing lesion.
Orthodontic appliances physically alter the microbial environment. Increased proliferation of the facultative bacterial population, including Streptococcus mutans , leads to a decrease in pH that tips the demineralization-remineralization balance toward mineral loss (demineralization), which in turn can lead to WSL development and eventually to cavitation and caries extending into the dentin.
The need for a systematic method of caries recording in epidemiologic studies led to the development of a visually ranked caries scoring system that was reproducible and accurate: International Caries Detection and Assessment System II (ICDAS II). Various stages of coronal caries are recorded in a reliable and reproducible way through clinical visual inspection. Compared with later-stage caries detection by radiographs, the ICDAS II allows for ready detection of small differences in caries lesions. The ability to detect early stages of enamel caries with high validity makes the ICDAS II the system of choice for clinical detection of WSL in orthodontic patients. In the absence of clinical observation, however, color photographs can be used instead as a proper alternative. Color photography as a means of recording enamel opacity is a powerful method. Assessment of enamel demineralization from color images appeared to be more reproducible than direct clinical observation with only the naked eye.
Since intraoral photographs are routinely taken of orthodontic patients before and after treatment, we created a scoring system tailored for use with photographic images. Such a system can be a useful method for longitudinal assessment of caries status from photographic records. In this study, we used intraoral photographs and a specifically designed system to determine the incidence of new coronal caries development on labial surfaces of teeth before and after orthodontic treatment.
Material and methods
Before patient record selection, this study received approval from the University of Michigan Institutional Review Board for Health Sciences (#HUM00015033, 8/10/2007, exempt). From 2296 patients treated in the graduate orthodontic clinic at the University of Michigan School of Dentistry between 1997 and 2004, 350 patient records were randomly selected by using a random number sequence generated at www.random.org Inclusion criteria for record selection consisted of patients who (1) underwent comprehensive orthodontic treatment with full fixed appliances on labial tooth surfaces; (2) had both complete initial and final series of intraoral photographs; and (3) had complete treatment log information in their charts. Patients whose appliances were removed prematurely before completion of orthodontic treatment were excluded.
Data collection from deidentified patient charts included sex and age at initiation of orthodontic treatment, and treatment variables such as extraction therapy and comprehensive treatment time. Comprehensive treatment time was defined as the period between the start of full fixed appliance therapy and the removal of all active fixed appliances. A limited phase 1 treatment before comprehensive treatment was not included in treatment-time calculation. Initial oral-hygiene score, frequency of oral-hygiene discussions, oral-hygiene instructions, and fluoride application or rinse were recorded from progress notes in the chart. Fluoridation of the patient’s primary water source was reported by the patient or guardian.
Intraoral pretreatment (initial) and posttreatment (final) photographs of each patient were taken as part of standard orthodontic record-keeping procedures. The posttreatment photographs were taken soon after debonding. All photographs, stored as 35-mm slides, were taken in the Clinical Photography Department at the University of Michigan School of Dentistry by 2 professional photographers using a standardized intraoral photography procedure. Mouth mirrors were rinsed with warm water, and the patient was asked to swallow before each photograph was taken. The position of the camera was in the occlusal plane and perpendicular to the maxillary incisors (frontal). The lateral photographs were taken by using a front-surface mirror. The shot was taken in the occlusal plane and perpendicular to the surface of the mirror, and an exposure compensation of 0.5 f-stop was used. The photographs were taken with a ring flash (virtually eliminating light reflections) at a fixed magnification of 1:1.2.
Initial and final photographs used for this study included a frontal view and right and left lateral views. Individual slides were scanned into digital format by using a Nikon Slide Feeder SF-200 (S) and Super Coolscan 4000 ED scanner (Nikon Corporation, Tokyo, Japan). Each 24-bit image with 4000 × 4000 dpi resolution was saved as a jpeg file. A total of 6 intraoral images per patient were scanned (3 pretreatment and 3 posttreatment slides).
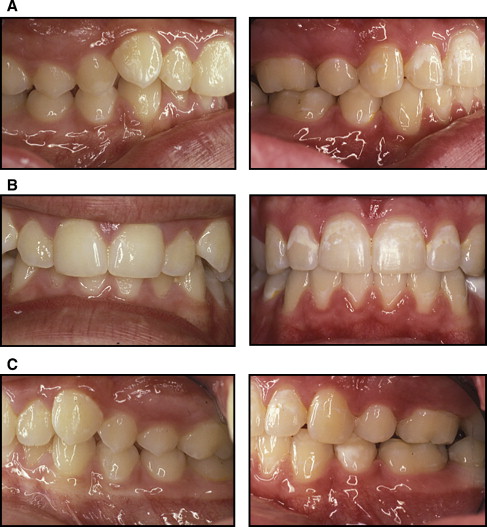
Scanned images were imported into an individual PowerPoint (Microsoft, Redmond, Wash) presentation for each patient. Each presentation consisted of 3 slides with a solid black background. The images of each patient were paired, displaying both the pretreatment and the posttreatment image of each view together on 1 slide, and enlarged to 325% of their original size. A typical example of the side-by-side arranged images is shown in Figure 1 . Investigators (A.E.R., A.O.A, and W.S.) could move back and forth in the image sequence while evaluating each patient.
The images were evaluated by trained investigators using a specifically adapted scoring system ( Table I ). Visible labial surfaces examined included maxillary and mandibular central and lateral incisors, canines, first and second premolars, and first molars. For the purpose of this study, the criteria for caries detection were based on 2-dimensional photographs. The chief investigator (A.E.R.) scored each visible labial tooth surface before and after orthodontic treatment. The scores were combined to determine the labial caries incidence for each patient.
| Score | Surface characteristic |
|---|---|
| 0 | Sound enamel |
| 1 | WSL |
| 2 | Cavitation |
| M | Missing due to caries, orthodontic extraction, unerupted, ∗ or congenitally missing |
| R | Restored † |
| 9 | Excluded because of inadequate photographic view |
∗ Unerupted surface at the initial record received a score of 0
The three investigators were calibrated in the use of the scoring system. They independently evaluated photographs of 35 randomly selected patients from the sample to determine interexaminer reliability. Fifteen days later, the same photographs were reexamined (A.E.R.) to determine intraexaminer reliability.
Statistical analysis
The overall incidence of labial caries development was determined from comparison of the pretreatment and posttreatment scores for each tooth. Lesion development was broken down into WSL and new cavitations. Means, standard deviations, and ranges were determined for surfaces affected by new lesions, and the incidence of new lesions was calculated. Incidence was defined as the number of new events: new cases of disease in the population, within a specified period of time. Teeth that could not be evaluated (score 9), on either initial or final records, were not included in the calculations.
The dependent variables (WSL and cavitation or caries) were compared with the independent variables (sex, age at start of treatment, extraction vs nonextraction, treatment duration, initial oral hygiene, frequency of oral-hygiene discussions, fluoride rinses or topical application, and fluoridation of patients’ water source and their interactions). The number of teeth developing new lesions was compared with the independent variables and analyzed with the Satterthwaite t test and analysis of variance (ANOVA). Multiple regression analysis was used to determine relationships between the dependent and independent variables mentioned above. Intraexaminer and interexaminer reliabilities were determined by using kappa statistics. All analyses were performed with software (version 9.1, SAS Institute, Cary, NC).
Results
Evaluation of examiner reliability demonstrated excellent agreement between initial assessments for both intraexaminer (kappa = 0.95) and interexaminer (kappa = 0.77, 0.85, and 0.85) agreement for lesion assessment.
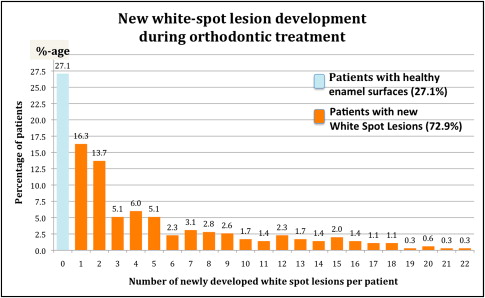
A histogram of the incidence of new WSL between the initial and final records is shown in Figure 2 . The overall incidence of patients who developed at least 1 WSL during orthodontic treatment was 72.9% (n = 255). The incidence of newly developed cavitated lesions that were unrestored on the final record was 2.3%. Of the 8 patients who developed cavitated lesions during orthodontic treatment, 4 (1.1%) developed 1 new cavitated lesion, 3 (0.9%) developed 2 new cavitated lesions, and 1 (0.3%) developed 4 new cavitated lesions. The overall number of patients exhibiting at least 1 new labial restoration (filling or full coverage) at the final records was 16 (4.6%). Of these 16 patients, 13 (3.7%) had 1 new restoration, and 3 (0.9%) had 2 new restorations.
The various changes in tooth status per patient (mean percentages and standard deviations) are summarized in Table II . Of the maximum of 24 surfaces investigated per patient, on average, 4.2 surfaces showed new WSL. There were only a few new cavitations (0.04) and restorations (0.05). Even though it happens infrequently, some early WSL regressed to sound enamel (reversals, 0.07).
| Changes per patient | Labial enamel surfaces | ||
|---|---|---|---|
| % | Mean | SD | |
| No change | 70.3 | 16.87 | 5.62 |
| New WSL | 17.3 | 4.15 | 5.11 |
| New cavitated lesions | 0.2 | 0.04 | 0.30 |
| New restorations | 0.2 | 0.05 | 0.26 |
| Reversals | 0.3 | 0.07 | 0.41 |
| Extracted teeth | 7.1 | 1.71 | 1.86 |
| Congenitally missing | 0.8 | 0.18 | 0.63 |
| Excluded (could not be judged) | 3.8 | ||
Table III presents the relationship between the development of WSL and cavitations and the independent variables. Demographic variables of sex and age at the start of treatment were not significantly related to the development of new decalcified or cavitated lesions. There was a significant relationship between increased treatment length and the number of newly developed decalcified lesions ( P = 0.03). The mean number of labial surfaces per patient who developed new WSL was 3.01 for those with a treatment length of less than 22 months. This increased to 5.28 teeth for patients with therapy longer than 33 months. The number of new cavitated lesions, however, showed only a nonsignificant trend ( P = 0.08) with increased treatment time. In addition, the number of newly developed lesions (both WSL and cavitations) showed no significant association with extraction or nonextraction treatment protocol.
| Independent variable | White-spot lesions | Cavitated lesions | |||||
|---|---|---|---|---|---|---|---|
| n | Mean † | SD | P value | Mean † | SD | P value | |
| Sex | 0.10 | 0 | 0.30 | ||||
| Female | 207 | 3.78 | 4.77 | 0.02 | 0.18 | ||
| Male | 143 | 4.70 | 5.53 | 0.06 | 0.41 | ||
| Age group (y) | 0.07 | 0.56 | |||||
| 9–12 | 59 | 5.15 | 5.62 | 0.02 | 0.13 | ||
| 12–13 | 79 | 4.53 | 5.31 | 0.13 | 0.11 | ||
| 13–16 | 147 | 4.14 | 4.91 | 0.05 | 0.38 | ||
| >16 | 65 | 2.82 | 4.61 | 0.08 | 0.37 | ||
| Treatment length (mo) | 0.03 ∗ | 0.08 | |||||
| <22 | 86 | 3.01 | 4.48 | 0 | 0 | ||
| 22–27 | 84 | 3.94 | 4.77 | 0.04 | 0.41 | ||
| 27–33 | 96 | 4.45 | 5.23 | 0.01 | 0.11 | ||
| >33 | 82 | 5.28 | 5.76 | 0.11 | 0.42 | ||
| Extraction vs nonextraction | 0.19 | 0.14 | |||||
| Extraction | 170 | 4.52 | 5.29 | 0.06 | 0.39 | ||
| Nonextraction | 180 | 3.80 | 4.92 | 0.02 | 0.17 | ||
| Initial oral-hygiene score | 0.06 | 0.31 | |||||
| Poor-fair (1-2) | 178 | 4.64 | 5.38 | 0.05 | 0.37 | ||
| Good-excellent (3-4) | 152 | 3.57 | 4.72 | 0.02 | 0.14 | ||
| Hygiene discussions (n) | <0.00 ∗ | <0.00 ∗ | |||||
| 0 | 212 | 3.08 | 4.15 | 0.01 | 0.12 | ||
| 1–2 | 93 | 4.84 | 5.63 | 0.02 | 0.21 | ||
| ≥3 | 45 | 7.78 | 6.16 | 0.20 | 0.73 | ||
| Primary water source | 0.55 | 0.15 | |||||
| Nonfluoridated | 120 | 4.23 | 4.93 | 0.02 | 0.13 | ||
| Fluoridated | 138 | 4.61 | 5.47 | 0.07 | 0.43 | ||
| Fluoride rinse recommended | 0.10 | 0.86 | |||||
| No | 308 | 3.95 | 4.93 | 0.04 | 0.30 | ||
| Yes | 42 | 5.60 | 6.12 | 0.05 | 0.31 | ||
| Topical fluoride treatment | 0.11 | 0.88 | |||||
| No | 307 | 3.96 | 4.94 | 0.04 | 0.30 | ||
| Yes | 43 | 5.53 | 6.06 | 0.05 | 0.31 | ||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


