Table 8.1
Before evaluating all this we have to define what are ours expectations of reference regarding the characteristics that a laser must have or must not have to be utilizable in implantology, and thus we will say:
It should have the minimal possible risk to damage the soft tissues as well as the hard tissues because of the overheating and the lateral diffusion of the heat. In fact, different wavelengths could be applied on soft tissues, according to the laser-tissue interaction, using correct parameters and protocols. Erbium laser family is the only laser capable to interact securely on hard dental tissues.
It should not be able to modify the implant surface especially with the modern bioactive surfaces in that it would jeopardize irreparably the characteristics and therefore the disposition for osseointegration.
It should have the best characteristics of decontamination of the implant surfaces by the useful power density as low as possible, remembering that power output inferior to 2.5W are not resolutive over the spores; This concept is at the base of decontamination techniques for implant surfaces and for a higher predictable and efficient management in the peri-implantitis cases. (Figg. 8.1-8.15)
Case 1: Peri-Implantitis (Fig. 8.1-8.15)
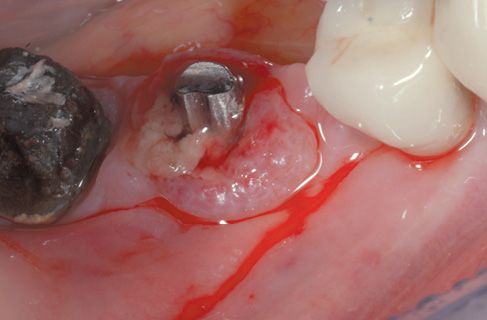
Figure 8.1 • Pre-operatory view of the surgical site.

Figure 8.2 • Pre-operatory x-ray.
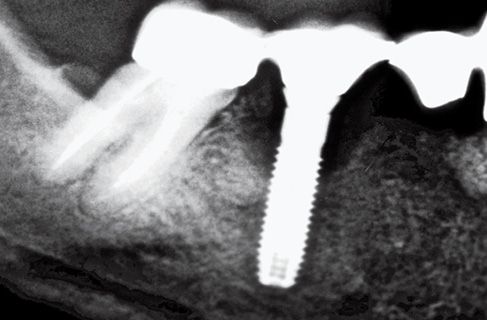
Figure 8.3 • Pre-operatory x-ray.
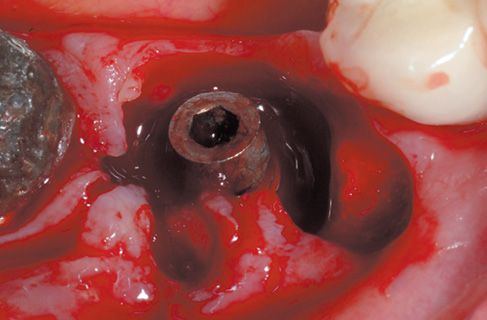
Figure 8.4 • View of perimplantary granulation tissue.
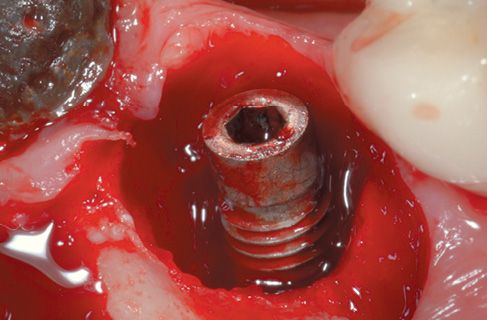
Figure 8.5 • View of the surgical site after diode laser decontamination.
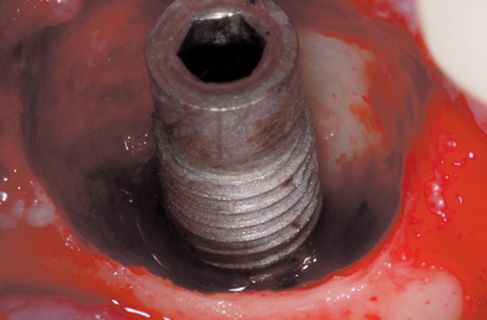
Figure 8.6 • View of the surgical site with granulation tissue perfectly removed.
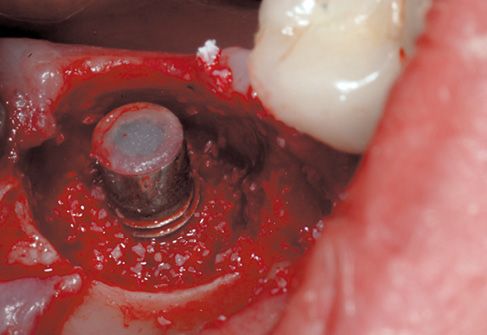
Figure 8.7 • Filling with biomaterial, first step.

Figure 8.8 • View of the surgical site, filling with biomaterial is completed.
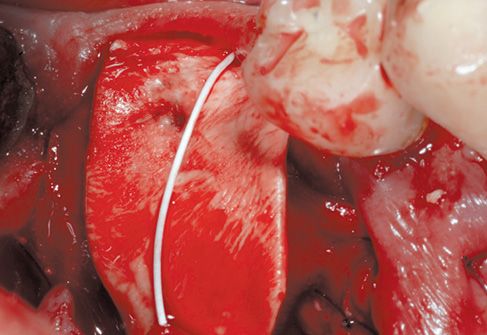
Figure 8.9 • The surgical site is protected with a connective membrane.
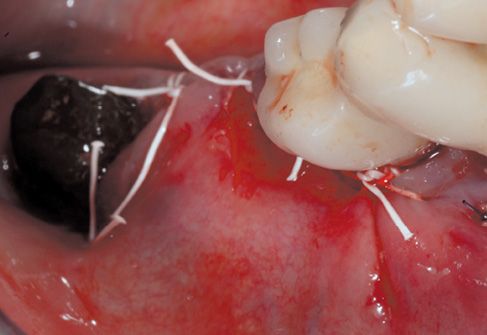
Figure 8.10 • After suitable tissue release, continuous suture with single points results perfectly sealed.

Figure 8.11 • Final x-ray, post-surgery.
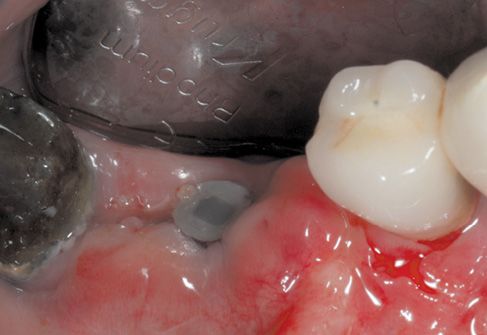
Figure 8.12 • Healing at 1 month.
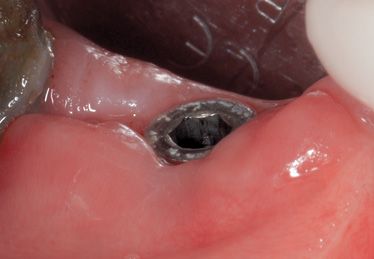
Figure 8.13 • Healing at 3 months.

Figure 8.14 • Control at 5 months.

Figure 8.15 • Control at 1 year.
It should be provided Preset (better if it could be brought up to date periodically with Updates of the producing house) that allows the operator to utilize always the protocols and the settings of the instrument that are more efficacious for the therapy in act.
It should have a great manageability and practical use: this will make us prefer the Laser with light transmission by optical fibers, for an easy access to the posterior areas in oral cavity than those with articulated arms and mirrors system.
THERAPEUTICAL INDICATIONS
In this section, we should consider how the Laser technology, if well managed with the correct parameters, could more and more simplify and make most of the procedures linked to the implant therapy in its different phases. Particularly, the medical Lasers could be of great efficacy in the various phases of the implant therapy: we will consider thus a typical therapy in all its phases and we will analyze the possible ideal applications of the Laser. (Table 8.2).
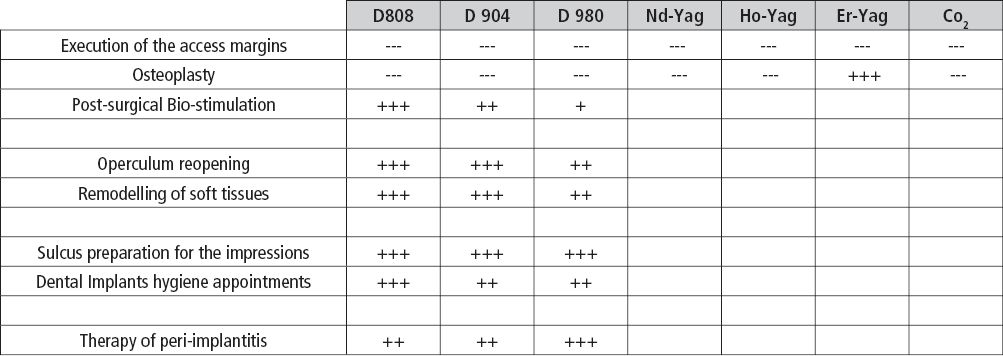
Table 8.2
PHASE I Surgical
Execution of the access margins: the surgical execution of the access margin should be always performed by a cold knife or with a non-laser technique. In fact the intrinsic characteristics of the laser in cutting soft tissue, produce haemostatic intravascular coagulation and a layer, even if minimal, of protein denaturation will make the margins not suitable for sutures, condition extremely advantageous in many circumstances but not in those where we want to obtain a perfect closing of the margins.
Osseous remodelling: the only laser really indicated to operate on bony tissues is the Erbium:YAG Laser because it absolutely is the “coldest” laser and, thanks to its ablative-hydrokinetic characteristics, we can obtain an effect of removal-remodelling, under water cooling, not associated with protein denaturation and vascular alteration of the osseous tissues: in this case, it is preferred to the traditional mechanical methods in many fine osseous applications.
Post-surgical biostimulation: Soft Laser (in particularly, the diode laser with its good tissue pene-tration capacity) used at very low power output (inferior to 0.1W) is able to exercise effects of at-tenuation of the post surgical oedema, to speed the recovery times and to attenuate the possible pain. (Fig. 8.16-8.17)
Case 2: Photo-Biostimulation (Fig. 8.16-8.17)
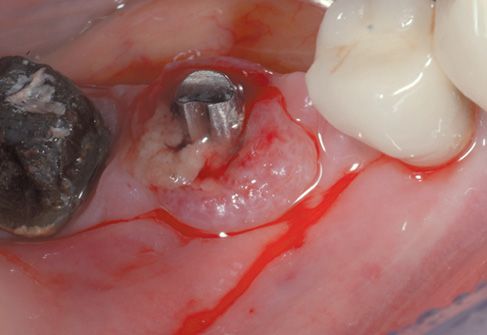
Figure 8.16 • Post-surgical photo-biostimulation, view of the distance between the handpiece, the defocused laser beam and the treated site.
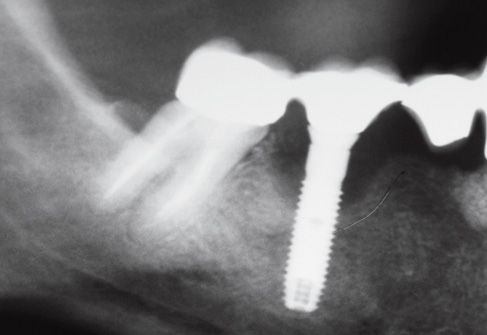
Figure 8.17 • X-ray control.
In the specifics, on top of the undeniable clinical evidences, several scientific studies have been car-ried on both in vitro and in vivo and they have demonstrate how the laser radiation, even at very low energetic power, could determinate several important and interesting effects at the level of the cellular metabolism.
For instance studies in vitro have demonstrated how the laser radiation performed by diode lasers (particularly Ga AI As Laser
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


