Fig. 18.1.
Increasing loads (vertical arrows) will increase the concavity (c). This process is compensated for by apposition on the concave side (C) and bone resorption on the convex side (T) of the bone. Accordingly, the medullary canal will also shift towards the resorption side (T). Similar conditions are encountered in the maxillary sinus most of the time. Since the concavity of the small inner lumen is routinely too pronounced, even minute loads will stimulate expansion of the bone tissue in this area. Inside the sinus we find a “frost upside down” situation. (From Martin et al. 1998)
Therefore, age-related involution does not take place in the paranasal sinuses (Kittel and Göhr 1965). The contrary is the case: involution of the bone limiting the lumen will result in further “pneumatization”.
When implants are placed along the maxillary sinus, both the osteotomy and the changing masticatory function of the restored teeth will interfere with a resting system. As a consequence of mastication and bone remodelling, both the shape of the maxillary sinus and the exterior shape of the maxilla may change. For this reason, we prefer the trans-sinus approach of implant insertion, in which the implant disk remains clear of the sinus floor. Thus the bone in the sinus floor area is allowed to float freely, which, in our experience, reduces the risk that further sinus expansion leads to caudalization of the implant with the possible consequence of premature contacts that may lead to osteolysis and implant fracture.
The following paragraphs are intended to verify the points raised in the previous list by considering additional properties of cortical bone:
-
If extensive augmentation of the sinus is performed (e.g. with parietal bone) and even supplemented with a Le Fort I down fracture, all direct relationships of the osteonal trajectories to the chewing muscles are severed or destroyed. Unless these structures regenerate spontaneously in the postoperative phase, the loads transmitted by the newly installed implants will be the prime determinant of the functional orientation of the reorganizing bone. Hence the direct stimulus of masticatory function ensures that major bone areas surrounding the implants remain in function.
-
For sinus augmentation with iliac bone blocks or autologous cancellous chips as grafting material, the implants have to be inserted either immediately or in due course before the enlargement of the concavity that results from the procedure is corrected as postulated by FNT. Following insertion of the implant, the confrontation between bone and implant surface (e.g. “extraterritorializing response” according to Donath) creates an effective incentive for bone preservation. The masticatory loads acting on the implants offer additional direct and indirect functional stimuli for bone preservation.
Surface stimulus of unloaded implant – the sheer presence of an extraneous material in the enossal space will influence bone remodelling and bone formation/mineralization.
Direct functional stimulus of implant – enhanced force transmission along the bone interface in enossal implants loaded by masticatory forces; this type of stimulus acts beyond the immediate contact area.
Indirect functional stimulus of implant – torsion between the cranial bones is enhanced as the activity of the masticatory muscles increases; this stimulus will even capture bone areas where no implants are installed but where modelling is prompted just by the increase in masticatory activity.
-
By contrast, if the sinus is augmented by adding non-resorbable extraneous material, the fact that the bone content is not resorbed will counteract the tendency of the sinus to expand. As a result, the interval until implantation can be much longer. Since the non-resorbable particles prevent the formation of longer trajectories, the concavity cannot be corrected even in cases where biochemical conditions are ideal. Non-resorbable or poorly resorbable augmentation materials behave like “mini-implants”, in that their sheer presence offers an incentive for bone preservation.
-
Much more serious forms of sinus expansion are observed when posterior teeth are lost at a young age than in cases where tooth loss occurs later in life. This is due to the higher BMU activation frequency (see Chapter 9.1) in younger patients, which is sufficient to promote bone remodelling in itself. Bone structures of older patients are characterized by a higher density of secondary osteons, less porosity and stronger mineralization.
-
Internal sinus grafting according to Summers will reverse the spatial configuration. Instead of a concavity, the peri-implant bone area is characterized by a bone convexity following this type of procedure that is more likely to resist bone resorption. This is compounded by the implant-related stimuli acting on this bone structure and favouring the preservation. The bone develops within a well-defined area and can be preserved in the immediate vicinity of the implant. The mechanism is similar to the one seen with natural molar roots extending into the maxillary sinus.
-
Once implants have been installed, the sinus will continue to change its spatial extension in accordance with the biomechanical realities. This is particularly true in cases of strategic implant placement where little functional stimulus is exerted directly by the implants. At the same time, qualitative and quantitative bone changes are likely to occur as the masticatory forces increase after denture sores have resolved. These alterations will involve either enhanced mineralization (if the bone volume remains constant) or an increase in total bone volume.
18.5 Implantological Approaches to the Sinus Area
There are two basic concepts for the placement of BOI implants in the distal maxilla and the sinus area.
18.5.1 Augmentation-Based Insertion of BOI Implants
In the 1980s, an implantation technique was introduced in connection with disk implants to treat the area of the maxillary sinus in the presence of insufficient vertical bone volume. This is achieved by first elevating the membrane before installing the basally osseointegrated implants. The procedure is started by performing an incision in the upper mesial area of the anterior vestibular sinus wall (e.g. in the canine fossa), then the membrane is carefully elevated in a dorsal, caudal and cranial direction. After drilling the implant bed and inserting the implant, the cavity created in the sinus is filled with a grafting material, sometimes mixed with autologous cancellous bone tissue. By and large, this procedure has yielded good results over the past 20 years. Sometimes the membrane ruptures when elevated. In that case, the surgeon must decide whether the augmentation procedure should be continued and an attempt be made to repair the membrane. In smokers, the membrane is very thin and therefore ruptures more frequently. By contrast, such tearing rarely occurs in membranes that are thickened by chronic inflammation. Also, the increased blood supply associated with inflammations may arguably promote the healing process.
In theory, it would be advantageous not to open the sinus completely. In practice, however, we have observed infections in the augmentation area separated by the bony sinus where they are particularly difficult to manage.
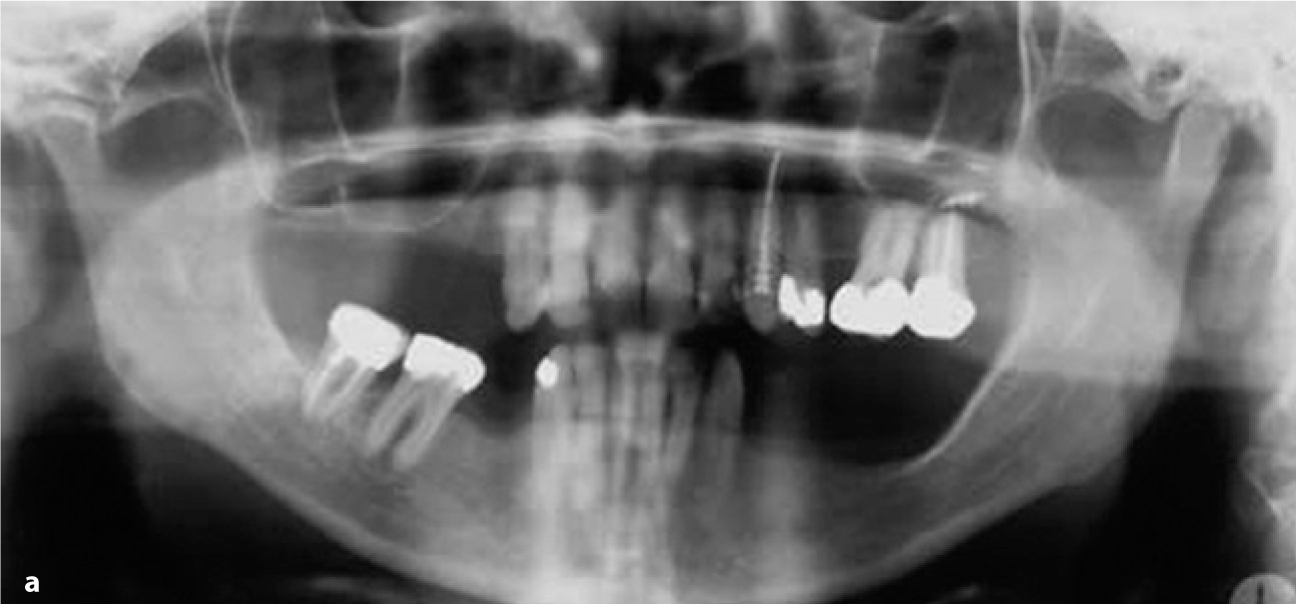

Fig. 18.2a,b.
These radiographs illustrates a case in which two double disk implants were inserted in the right maxilla with adjuvant sinus floor augmentation. The second radiograph was obtained 5 years after the procedure. All implants had been immediately loaded
Anyhow, since load transmission is confined to the ring area of the disks, the customary approach used with crestal implants of introducing a filling material in order to create a load-transmitting implant bed does not even offer theoretical advantages.
One disadvantage of this technique is that the (yet unorganized) augmentation material is in continuous contact with the oral cavity as the mucosa is penetrated by the threaded pin. In our experience, inorganic augmentation materials are better suited for this approach, since any postoperative contact of human bone grafts with the oral cavity is absolutely contraindicated.
Another problematic factor is that the integrity of the membrane inside the sinus itself cannot be verified too well during the procedure. A useful approach to sinus grafting is the technique described by Donsimoni (2003) in which the membrane is only dislodged in the small area immediately surrounding a previously prepared bone cover. Subsequently, suction is applied through the nose, which will gradually elevate the membrane in the absence of direct manipulation. This technique is said to involve a lower incidence of membrane rupture.
In situations where ventilation conditions are inadequate, an additional ventilation pathway must be considered. One way of creating such a pathway would be to fenestrate the area of the lower nasal meatus. Some otorhinolaryngologists have qualified this approach as obsolete, arguing that the drainage pathway for mucus by the defined cilium beat is not affected by this lack of ventilation. This viewpoint is correct with regard to chronic sinusitis. In connection with sinus grafting, however, the eventuality of acute infection and retention must be averted. Therefore, a fenestration as suggested above is absolutely indicated as a precaution against acute events occurring in the sinus both during and after the augmentation procedure. More recently, some otorhinolaryngologists have advocated the use of a drainage tube, to be inserted in the lower nasal meatus as a preoperative measure.
Regarding the medium- and long-term mobility of the implant-restoration complex, the results of transsinus implantation with augmentation may vary substantially. The following outcomes may occur in any combination:
-
The BOI implant is integrated in the vestibular and palatal cortical bone.
-
The BOI implant is better integrated in the augmentation area than in the cortical area (the augmentation area may be mobile or immobile against the cortical area).
Depending on the situation, even successful implants are likely to involve some mobility of the implant-restoration complex. This is true especially if papyraceous thin bone structures were present before the treatment was started, as these do not tend to favour a uniform interconnection between the cortical and the augmentation material. Another factor to consider is that the functional stimuli on cortical bone areas may be reduced by the implant being so firmly integrated in the augmentation material that the native bone structure in the area may disappear.
18.5.2 Trans-sinus Insertion of BOI Implants
Trans-sinus installation of BOI implants is today a routine procedure in dental implantology (Konstantinovic 2003). The most important requirement in this approach is that the opposite cortical structure (i.e. the palatal ridge or the lateral nasal wall) is safely reached and that primary stability of the BOI implant is ensured both on the vestibular and on the opposite side (see Video 9). The harder part is to obtain primary stability in the vestibular bone because the numerous cutting procedures may quickly give rise to inadvertent expansion of the vestibular osteotomy gap. The number of cutting procedures can be reduced by using the newer generation of cutters operated with contra-angle handpieces. The risk of placing the osteotomy too high is greatly reduced with these cutters. Treatment under anaesthesia should still be considered in alveolar ridges characterized by poor accessibility and strong resorption, since anaesthetized patients will not perform uncontrolled movements, so that the surgeon can devote his whole attention to the osteotomy. Today the technical indications for anaesthesia are greatly reduced by the availability of contra-angle handpieces.
The case report in Fig. 18.4a–c illustrates the potential of the BOI system in the non-augmented sinus maxillaries:
Even most BOI users at one time attempted to circumvent the maxillary sinus. This approach has been abandoned, however, based on long-term observations and improvements made to the implant design:
-
Today we know from long-term observations that the survival rate of BOI implants is greatly influenced by the disk diameter. The probability of survival is highest with disk diameters of at least 12 mm (rate of implant loss: <0.5%). This superior outcome of BOI implants with large-diameter disks is attributed to their better force distribution, cortical bone support and protection against infection.
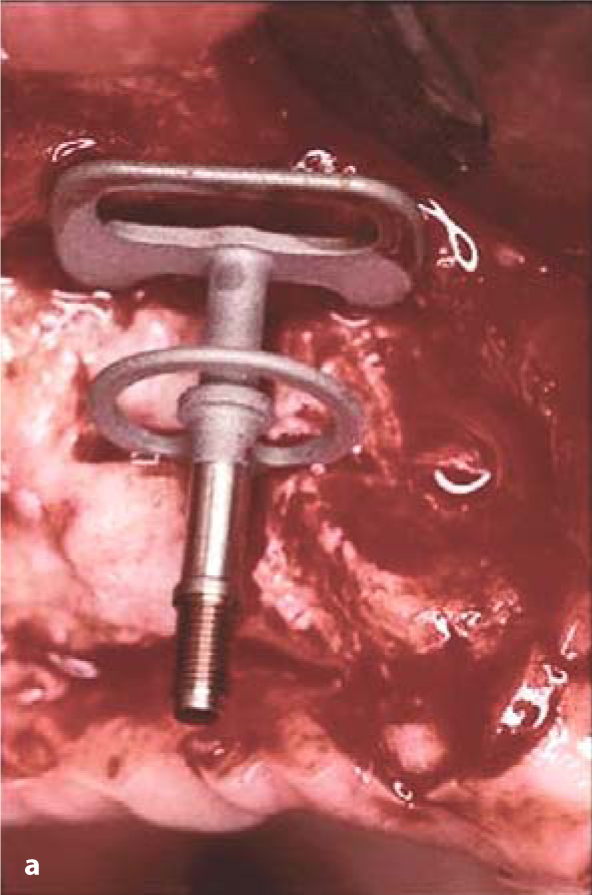
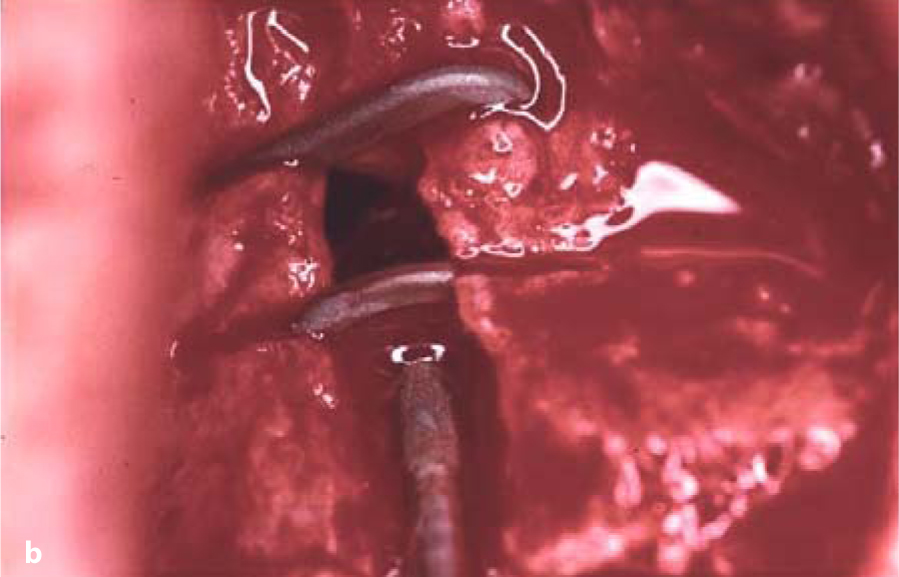
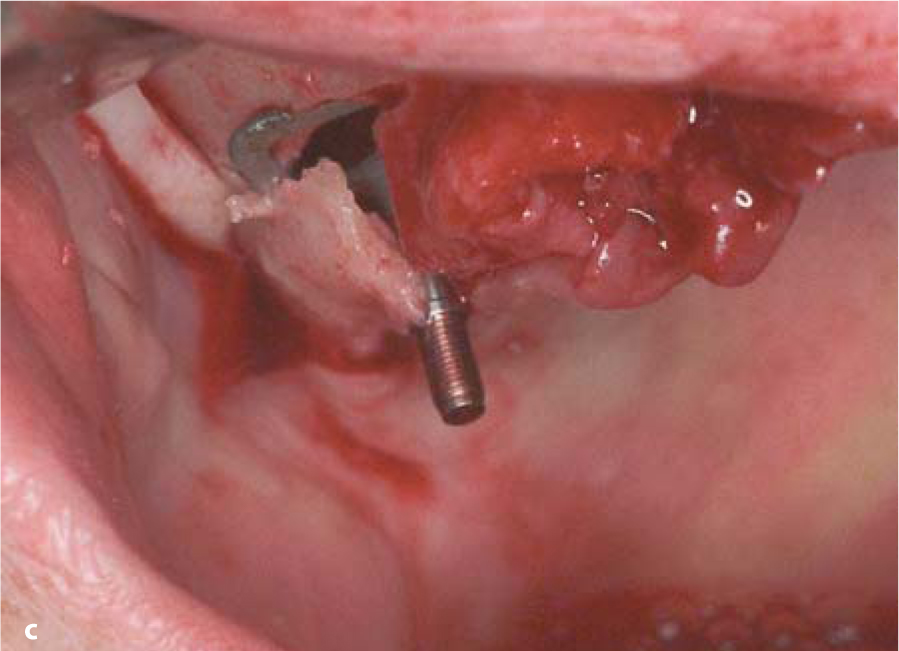 Fig. 18.3.a Lateral insertion of a double-disk BOI implant through the maxillary sinus. b The insertion gap was closed with a mixture of autologous bone and Bio-Oss. c BOI implant placed straight through the sinus in the area of tooth 17. Onlyone edge of the BOI implant protrudes from the bone. This loading area is sufficient even for immediate loading if the mastication is well balanced
Fig. 18.3.a Lateral insertion of a double-disk BOI implant through the maxillary sinus. b The insertion gap was closed with a mixture of autologous bone and Bio-Oss. c BOI implant placed straight through the sinus in the area of tooth 17. Onlyone edge of the BOI implant protrudes from the bone. This loading area is sufficient even for immediate loading if the mastication is well balanced -
In many cases, these large-diameter implants cannot possibly be inserted in the subantral area even if an angulated rather than horizontal insertion path is selected. Frequently, even implants with a disk diameter of 10 mm are not an option. Therefore, it is routinely necessary to consider a more cranial surgical approach.
-
Granulomas, cysts and other undesirable tissue formations can be removed right through the osteotomy gap when the trans-sinus approach is selected.
-
Any implant-related inflammations that might possibly occur sooner or later would quickly affect and destroy a considerable part of the overall bone structure, which is reduced anyway. This eventuality is avoided if the load-transmitting interface is anchored elsewhere to begin with. In that case, most types of inflammation will be able to pass the narrow residual ridge without inflicting major damage.
-
A maxillary sinus with intact “autocleaning function” offers good drainage pathways to deal with potential inflammations. Particularly in the initial phase of wound healing, the drainage may work both ways – i.e. into the oral cavity as well as into the sinus area. Hence there is no need to terminate the implantation procedure (i.e. installation of BOI implants without adjuvant sinus augmentation) if the sinus membrane is perforated. Such an incident does not per se require further treatment. The patient should be informed, however, to remember to be gentle with this area. Any application of pressure as in nose blowing or pressure compensation must, of course, be strictly avoided.
This development was triggered by growing evidence that the healing process after inadvertent opening of the sinus during BOI implantation procedures was generally uneventful. In this way, surgeons were gradually encouraged to routinely use the non-augmented maxillary sinus as an implantation site.
In our experience, the surface structure of the implant in general and of the threaded pin in particular is especially important in this type of procedure. The former disk implants with their surface-enhanced shafts used to favour cross-contamination from the oral cavity to the sinus in the manner of a candle wick. Screw implants are known to involve similar problems. In BOI implants, which feature a smooth surface along the thin shaft (threadholders), this type of problem is almost non-existent. Using this concept, there is no need to create an additional ventilation pathway in the maxillary sinus unless the patient has a history of sinus problems or, more importantly, if intraoperative verification shows that adequate ventilation is present. Note that the vertical implant segments do not osseointegrate, which is why inflammations in this area will not primarily spread to the bone. This is where BOI implants differ from osteosynthesis plates, where osseointegration along the screw thread is an obvious requirement. Although this integration is achieved in the early phase, osteosynthesis in the craniofacial region (and especially in the area of the frontal sinus) will frequently involve loosening of the screws and a pronounced tendency towards osteolysis down the road because there is no soft-tissue layer between the screw and the bone offering nutrition and spatial limitation at the same time.
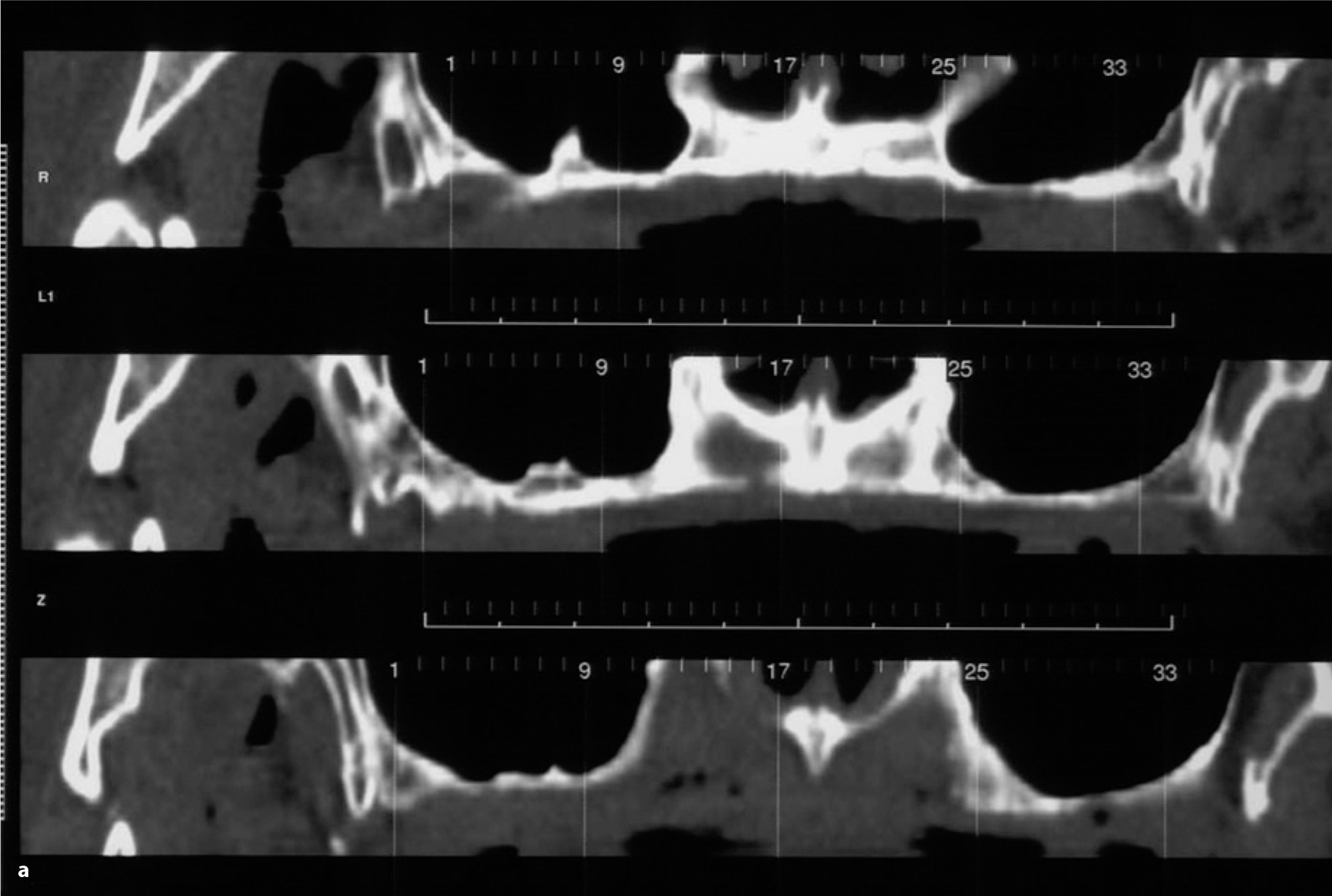
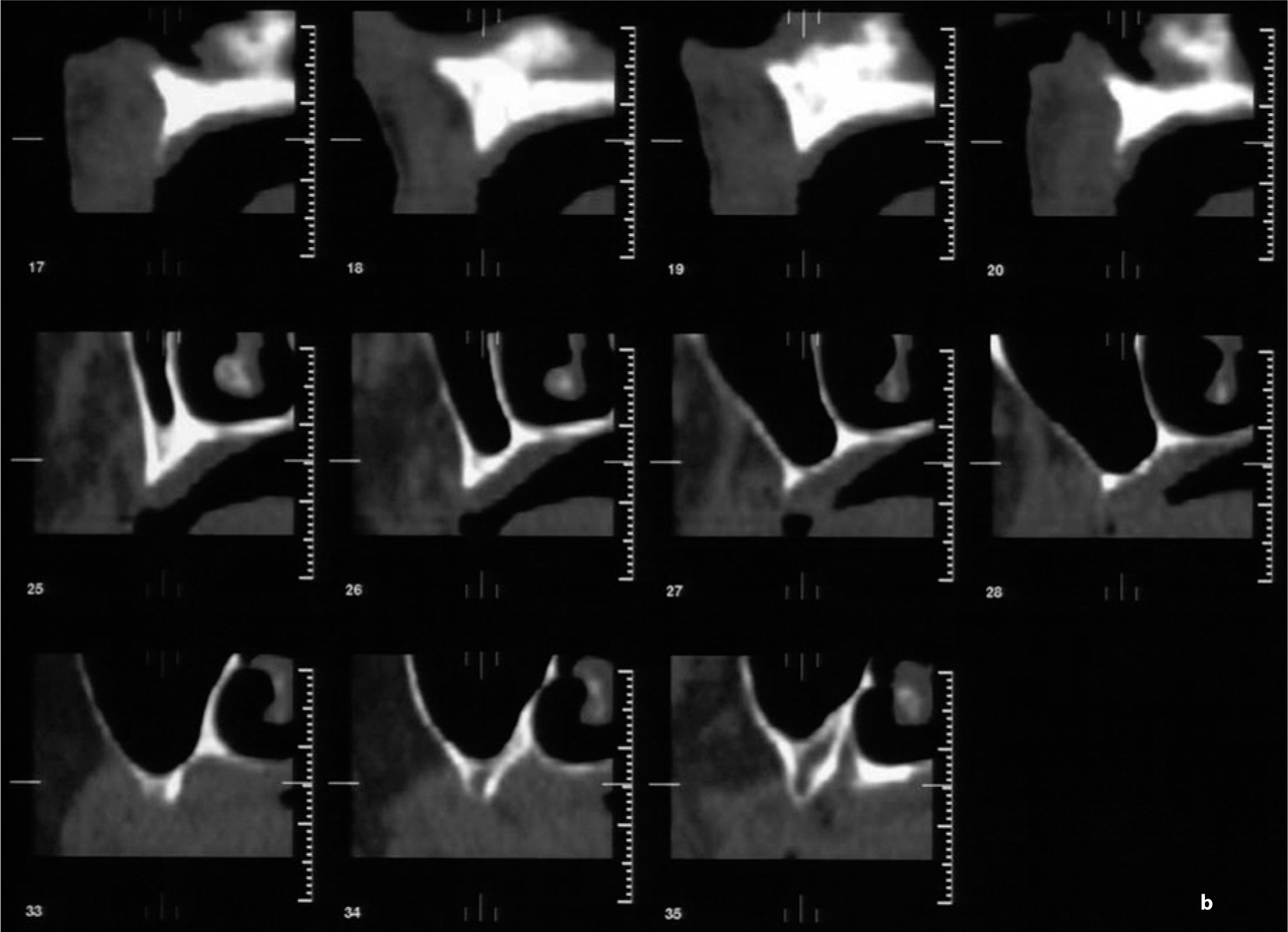

Fig. 18.4.
a Overview CT scan of the maxilla (three sections, distance 3 mm) showing extreme bone resorption. b Cross-sectional imaging of the right maxilla indicated that the bone volume available in the anterior segment was adequate. Bone height was, however, far below 10 mm; the zygomatico-alveolar crest was very flat. A greater amount of residual bone was available at the transition zone from the medial sinus wall to the palate and lateral nasal wall. This structure was a suitable anchorage point for the distal implant. The palatal artery is clearly visible. Segmented implant placement without prosthetic balancing to the contralateral side could not be performed without augmentation. Using the anterior ridge for anchorage would presumably have created substantial phonetic problems and rendered the laboratory work very difficult as well. c Dimensions. An area of thickened mucosa can be seen in the distal segment of the right sinus. The partial denture in the mandible is visibly characterized by occlusal surfaces of composite protruding from the occlusal plane. The BOI implants were loaded immediately on insertion
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


