This case report describes the treatment of a 14-year-old adolescent patient who had 2 impacted maxillary central incisors with distoangular root dilacerations. He also had an impacted maxillary left canine, with the crown completely overlapping the root of the lateral incisor, and insufficient space. The general dentist referred this patient because the maxillary central incisors had still not erupted 2 years after extraction of the retained deciduous incisors. A unilateral expander with a modified vestibular arch and an attachment spring on the right side was used to correct the posterior crossbite on the right side and improve the positions of the teeth. The expansion appliance was also applied as a high anchorage device to move the central incisors and the left canine into position during the initial stages. After this phase, fixed appliances were used to redistribute the space in the anterior maxillary region to create enough space for repositioning the impacted teeth. This procedure restored the normal appearance of the maxillary arch, with good periodontal health and without evidence of root resorption, apart from the distoangular root dilacerations of the 2 maxillary central incisors.
Eruptive disturbances are alterations of normal tooth eruption, including accelerated, delayed, failed, or deviated in the direction of tooth eruption, and can be related to general or local etiologic factors. An impacted central incisor is usually diagnosed during the mixed dentition, because maxillary central incisors usually erupt before the canines, when a child is between 8 and 10 years of age.
The principal local factors involved in this anomaly are supernumerary teeth, odontomas, and trauma. Dilaceration can be a sequel of trauma and is associated with maxillary central incisor eruption failure. The dilaceration can be mild, moderate, or severe and can alter the eruptive pathway of the tooth, causing impaction.
The purpose of this case report is to describe the treatment of a patient with both maxillary central incisors impacted with distoangular root dilacerations. The maxillary left canine was also impacted, and a unilateral posterior crossbite was present on the right side.
Diagnosis and etiology
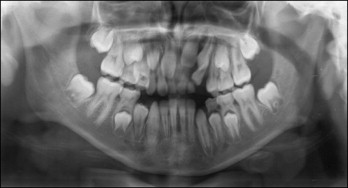
A 14-year-old boy was referred by his dentist because neither maxillary central incisor had erupted 2 years after extraction of both retained central and left lateral deciduous incisors ( Fig 1 ). He had a permanent dentition, and his chief complaint was an unesthetic smile because of the unerupted maxillary central permanent incisors ( Fig 2 ).
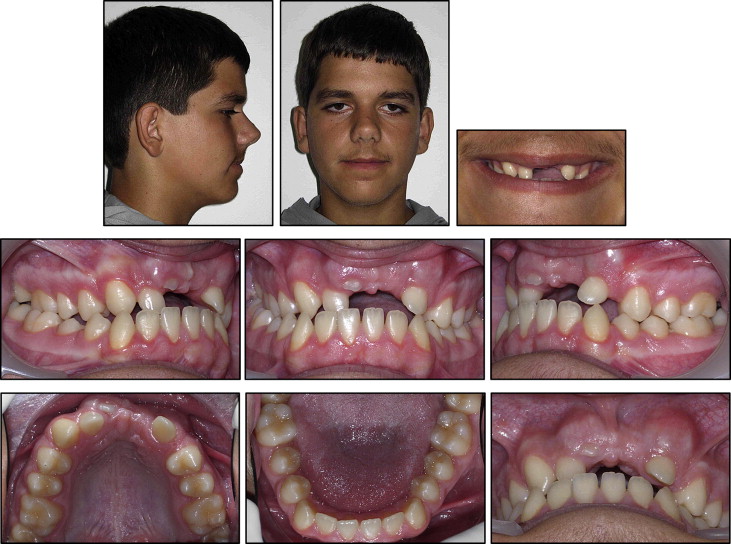
The patient was physically healthy and had a history of dental trauma when he was 7 years old. However, there was no mention of any tooth displacements or intrusion injuries. The facial photographs showed a concave profile and a retruded upper lip with an obtuse nasolabial angle ( Fig 2 ). There were no gross asymmetries. This patient had no parafunction or dysfunction, and the examination and history disclosed no temporomandibular joint disorders.
Both maxillary central incisors were impacted and lacked adequate space for proper eruption because of the drift of adjacent teeth into the unoccupied spaces ( Figs 2-4 ). The maxillary dentition exhibited a narrow asymmetric dental arch with a unilateral right posterior crossbite (from the right lateral incisor to the right first molar), which was due to lingual tipping and a slight mandibular functional shift. There was significant dental crowding in the maxillary arch, with a Class II molar relationship on the right side and a Class I relationship on the left side. No crowding was present in the mandibular arch, even though the mandibular right canine was malpositioned. Overjet and overbite were −2.3 and −5.5 mm, respectively.
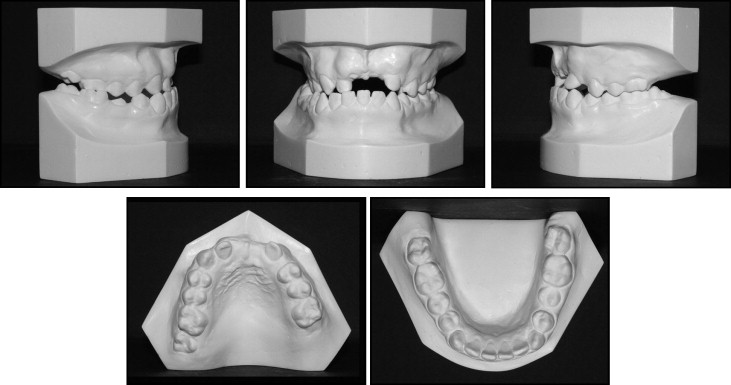
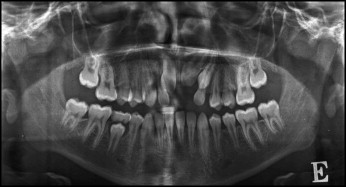
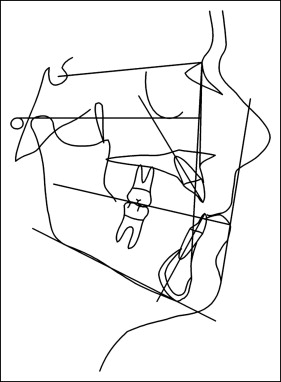
The radiographs showed 2 impacted maxillary central incisors with root dilacerations and an impacted maxillary left canine (the incisal tip of the canine overlapped the root of the lateral incisor ( Fig 4 ). The cephalometric analysis showed a normal skeletal pattern with normal inclination of the mandibular incisors and proclination of the impacted incisors contributing to the acute interincisal angle ( Figs 5 and 6 ; Table ).

| Cephalometric measurement | Norm | Before treatment | After treatment |
|---|---|---|---|
| FMIA (°) | 67 ± 3 | 61.4 | 63.8 |
| FMA (°) | 25 ± 3 | 27.2 | 24.5 |
| IMPA (°) | 88 ± 3 | 91.4 | 91.7 |
| SNA (°) | 82 ± 2 | 83.2 | 86.9 |
| SNB (°) | 80 ± 2 | 81.4 | 84.3 |
| ANB (°) | 1-5 | 1.8 | 2.7 |
| Ao Bo (mm) | 2 ± 2 | −7.0 | −5.9 |
| UI/NA (°) | 22 ± 2 | 32.3 | 20.2 |
| Occlusal plane (°) | 8-12 | 14.0 | 12.3 |
| Z-angle (°) | 75 ± 5 | 80.9 | 74.2 |
| Posterior facial height (mm) | 45 | 48.7 | 58.5 |
| Anterior facial height (mm) | 65 | 76.4 | 80.4 |
| Index post ant | 0.69 | 0.67 | 0.7 |
| Overjet (mm) | 2.5 ± 2.5 | −2.3 | 4.0 |
| Overbite (mm) | 2.5 ± 2.5 | −5.5 | 3.2 |
| Interincisal angle (°) | 126 ± 10 | 120.3 | 133.0 |
Treatment objectives
The following treatment objectives were established for this patient: (1) correction of the posterior crossbite and attainment of adequate space for positioning the impacted central incisors, (2) distal positioning of the right canine to improve its relationship, and (3) fixed appliances to gain adequate space for repositioning the impacted teeth and to create a stable functional occlusion.
Treatment objectives
The following treatment objectives were established for this patient: (1) correction of the posterior crossbite and attainment of adequate space for positioning the impacted central incisors, (2) distal positioning of the right canine to improve its relationship, and (3) fixed appliances to gain adequate space for repositioning the impacted teeth and to create a stable functional occlusion.
Treatment alternatives
Three treatment alternatives were developed: (1) extraction of the unerupted central incisors and restoration with a bridge or implants later when growth had ceased; (2) extraction of the unerupted central incisors with autotransplantation after orthodontic space opening; and (3) orthodontic space opening, uncovering and traction of the impacted teeth, and alignment of these teeth into their proper positions.
Treatment plan
The treatment plan consisted of 2 stages. The first phase involved unilateral expansion (due to the right crossbite). The second stage involved fixed appliances allowing redistribution of the space in the anterior maxillary region to create enough space for the traction of the impacted teeth and their alignment to obtain a good final occlusal relationship.
Treatment progress
In the first stage, a unilateral expansion appliance with a modified vestibular arch and an attachment spring was placed to improve the transverse maxillary constriction, the lingual tipping, and the slight functional crossbite ( Fig 7 ). After the crossbite correction, a Class I molar relationship was obtained on the right side ( Fig 8 , C ).




