Tooth impaction involves factors such as lack of space in the alveolar process, trauma, ankylosis, and mechanical barriers such as abnormal frenum, supernumerary teeth, tumors, and local cysts. When impaction occurs in the anterior region, esthetics are compromised. This report describes the successful approach to treatment for a young boy who had 2 supernumerary teeth associated with impaction of the left central and lateral permanent incisors. Treatment consisted of extracting the supernumerary teeth and performing maxillary expansion with a modified Haas appliance to guide the left central incisor into its appropriate position. The teeth erupted spontaneously after maxillary expansion and an increase in space. A fixed edgewise appliance was placed incrementally to correct the maxillary anterior tooth positions and finish the treatment. Adequate esthetics and function were achieved.
The eruption of permanent teeth is a complex, mostly genetically based series of events in which eruptive movements of the tooth germ take place at a predetermined time and route, and enable the tooth to find its antagonist and establish the occlusal plane. A tooth normally erupts when one half to three quarters of its final root length has developed. Delay in the eruption of a maxillary permanent incisor is a problem occasionally encountered by an orthodontist, and it can indicate impaction. Impacted teeth can cause a series of potential problems such as root displacement and resorption, periodontal problems in adjacent teeth, referred pain, and formation of cysts and odontogenic tumors. In the anterior region, there is the additional concern of altered esthetics.
The etiology of tooth impaction has been described as multifactorial, involving genetic and environmental factors, such as lack of space in the alveolar process, abnormal frenum, prolonged retention of deciduous teeth, trauma, ankylosis, supernumerary teeth, tumors, and local cysts. The maxillary central incisors are the third most commonly impacted teeth in white people, preceded by the third molars and the maxillary canines. The incidence of central incisor impaction is about 0.06% to 0.2% in the general population.
Impacted maxillary anterior teeth can be a challenging problem, and treatment frequently requires orthodontic and surgical interventions. The treatment protocol includes orthodontic space opening, removing the etiologic factor, exposing the impacted tooth, maintaining the open area, and applying traction to the impacted tooth. Several techniques are commonly used to uncover maxillary impactions, including an apically positioned flap, which consists of apically repositioning the raised flap that incorporates the attached gingiva overlying the impacted tooth. The crown of the impacted tooth remains exposed for attachment of an orthodontic bracket. Another technique, the closed-eruption technique, involves raising the flap that incorporates the attached gingiva over the impacted tooth, bonding an orthodontic bracket to the tooth, and then fully replacing the tissue over the tooth and the bracket. Sometimes, however, surgery is not required, because the space-opening procedure can cause spontaneous eruption of the impacted tooth.
In this case report, 2 supernumerary teeth were associated with impaction of the left central and lateral permanent incisors. Treatment consisted of extracting the supernumerary teeth (removing the etiologic factor) and expanding the maxilla with a modified Haas appliance to guide the left central incisor to its appropriate position. No surgery was required to expose the incisors, and the teeth erupted spontaneously after maxillary expansion and the increase in space was obtained.
Diagnosis and etiology
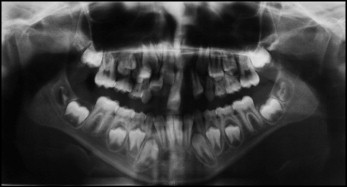
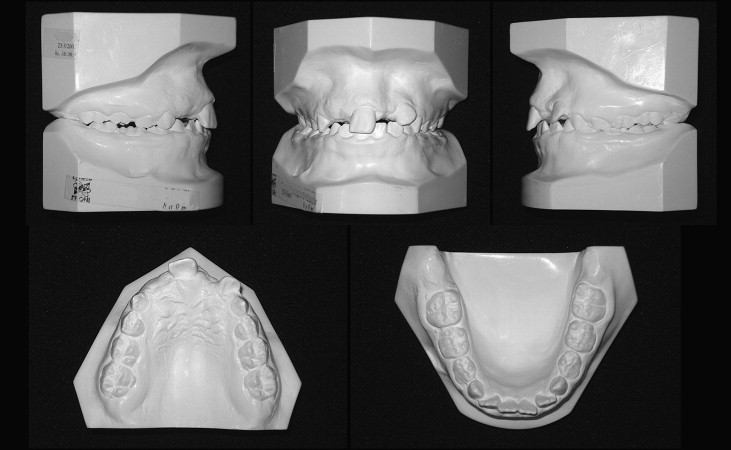
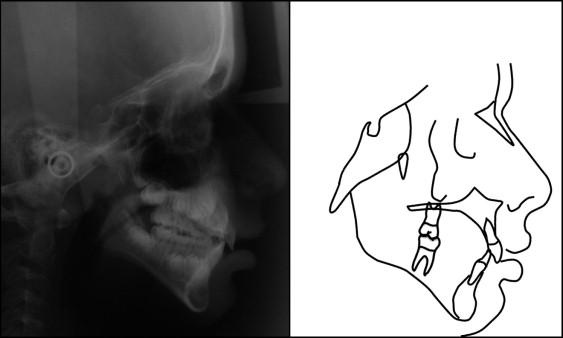
A boy, aged 7 years 4 months, with a history of trauma in the maxillary anterior region when he was 1 year 6 months, sought treatment at our dental office, bringing his panoramic and occlusal radiographs with him. The panoramic radiograph ( Fig 1 ) showed that the right central and lateral permanent incisors were blocked intraosseously because of a supernumerary tooth. Another supernumerary tooth was present between the left central and lateral permanent incisors, and it blocked the pathway to eruption of the left permanent canine and severely displaced the permanent incisors. All 4 maxillary incisors showed severe displacements and alterations in their eruption paths. The clinical examination showed an Angle Class I malocclusion, a relatively straight profile, normal vertical facial proportions, normal nasolabial angle, and absence of the right central incisor. The maxillary left central incisor was deviated 7 mm from the midline to the right quadrant.

The recommendation was to extract the supernumerary teeth before beginning the orthodontic treatment. After surgery, photographs, radiographs, and plaster casts were obtained ( Figs 2-5 ).

Treatment alternatives
Fundamentally, we did not believe that there was another treatment alternative than extracting the supernumerary teeth and gradually guiding the maxillary anterior teeth, as they were erupting, to their correct positions. One point that could be questioned is whether the palatal expansion with a modified Haas appliance was needed. The patient did not have a maxillary transverse deficiency, but we decided to use the expander to give more room for the teeth to erupt. In this situation, the treatment options could also be to (1) extract the supernumerary teeth, wait for spontaneous eruption of the impacted teeth, and start orthodontic treatment, gradually implementing complete fixed orthodontic appliances during the eruption of the permanent teeth; or (2) remove the supernumerary teeth, start maxillary rapid expansion with a modified Haas appliance, and incrementally place edgewise brackets to gradually guide the impacted teeth to their correct positions. After careful consideration, the second alternative was chosen.
Treatment progress
The first step was to remove the etiologic factor. The patient underwent 2 surgeries to remove the supernumerary teeth. The left supernumerary was removed at a private dental office, and the right one was removed during an adenoidectomy performed at a surgical center.
To gain space for the incisors to erupt and guide the erupted left central incisor to its position, a modified Haas appliance was built with a coil spring (0.28 in) in contact with the mesial surface of the central incisor ( Fig 6 , A ). The modified Haas appliance was activated 1 mm in the first day and 0.25 mm twice a day until the 11-mm-long screw was completely activated. During the Haas activation, the coil spring naturally displaced the left central incisor toward the left side. At the same time, 2 standard 0.022-in edgewise brackets (American Orthodontics, Sheboygan, Wis) were bonded to the maxillary left central and lateral incisors. A segmented stainless steel archwire (0.016 in) with a T-loop was inserted and activated between the left incisors until space closure was achieved ( Fig 6 , B ).




