Introduction
In this study, we aimed to assess the patient and treatment factors that influence the success rate and the duration of the orthodontic-surgical modality for impacted central incisors.
Methods
The records of 60 consecutively treated patients (64 impacted incisors) were retrospectively evaluated. The success rate and the duration of each stage of treatment were examined in relation to age, sex, etiology of impaction, location of the impacted tooth, and type of surgical exposure performed. Logistic regression analyses were applied.
Results
The group consisted of 26 male and 34 female subjects, 7.0 to 21.9 years old; 27 patients had impactions because of root dilaceration, 29 had impactions because of obstruction, and 4 had impactions with unknown causes. The overall success rate was 90.0%. Five of the 6 failures were dilacerated incisors. The average duration of treatment was 21.6 ± 8.7 months. The only factor that significantly increased the duration was the height of the impacted tooth. Dilaceration was related to a longer stage of traction and, in older patients (late mixed and full permanent dentition), to a longer finishing stage.
Conclusions
The orthodontic-surgical treatment of impacted incisors is generally successful, but relatively long. Patients and parents should be warned of the risk of failure and the increased treatment duration, especially for dilacerated incisors impacted high in the alveolus.
Highlights
- •
We reported on the level of risk of failure in the treatment of impacted central incisors.
- •
We reported on the importance of the etiology as the principal factor influencing the prognosis.
- •
We reported on the duration of treatment of impacted central incisors.
- •
We determined the main factors that increase the treatment time.
Although the prevalence of noneruption or impaction of the maxillary central incisor is low, its occurrence is disfiguring for a young child and of considerable concern to the parents. The causes of this phenomenon can be divided into 2 main groups: obstructive and traumatic causes.
The most common obstruction in the anterior maxilla is the presence of at least 1 midline supernumerary tooth. The frequency with which this occurs has been found to be between 1.5% and 3.5% in random population samples, although only between 28% and 60% of these patients will have resultant eruption disturbances of the incisors. Odontomes are much rarer findings that cause obstruction in this area, and they may vary in size and type (complex or composite).
Trauma at an early age, before the permanent teeth have erupted, can cause damage to the root-forming cells of the unerupted permanent tooth germ and an attenuated productivity rate of the root portion, and also change the orientation of the tooth in the alveolar process. This results in the development of a dilacerated tooth, which will then not usually erupt unaided.
The parents of a child with an unerupted central incisor, unilaterally or bilaterally, will usually be motivated to seek treatment much earlier than the parents of a child with almost any other orthodontic problem. From the clinical point of view, early treatment is important for the following reasons: (1) an unerupted maxillary central incisor can cause unesthetic and compromised appearance, oral function, and speech; (2) it can cause tipping of adjacent teeth, thus reducing the space for the unerupted incisor; and (3) it is a significant environmental influence in delaying and altering the eruption path of the ipsilateral maxillary canine.
The available treatment options for this condition include (1) extraction of the tooth followed by prosthodontic rehabilitation; (2) extraction of the tooth and realignment of the lateral incisor into the central incisor position, with the canine and premolar sequentially moved mesially and anatomically modified by grinding, crowning, and so on; or (3) the orthodontic-surgical modality.
Most patients seeking treatment for impacted central incisors are young children. Therefore, any prosthodontic solution can only be temporary and will need to be modified and updated several times before a more permanent solution becomes possible at age 18 years or so, at the cessation of growth. Extraction of the impacted tooth will also lead to severe alveolar bone loss that will undermine the future implant site.
In contrast, the orthodontic-surgical solution aims for complete alignment of the natural teeth and requires no prosthodontic enhancement. The eruption of the impacted tooth draws the surrounding alveolar bone to produce a bony crest height and periodontium similar to those of the adjacent teeth.
In the past, it had been assumed that space opening and elimination of the cause would be adequate to produce spontaneous resolution of the impaction. However, evidence-based studies have shown that autonomous eruption occurs in only 54% to 78% of patients, with a delay of up to 3 years and with spontaneous acceptable alignment occurring in only a few patients.
More recent research has examined the effect of several variables on the eruption of impacted teeth in children after the removal of supernumeraries or odontomes. This study found disappointing outcomes regarding spontaneous eruption after extraction of the impediment, which varied in relation to its type and form. The authors did not investigate whether acceptable alignment occurred in the successful subjects, leaving the reader to assume that orthodontic treatment would still be necessary in many patients and justifying the need for a phase 1 procedure.
The treatment of impacted central incisors with dilacerations requires a different approach and is usually lengthy and more complicated. This explains why many patients, dentists, and orthodontists prefer surgical repositioning or extraction with prosthodontic rehabilitation as viable alternatives. However, attitudes seem to have changed recently, with more case reports of orthodontic treatments appearing in the literature.
In contrast to the parallel situation in regard to impacted canines, data concerning the success rate and duration of the orthodontic-surgical modality treatment of impacted central incisors are sparse. Most of the articles offer isolated and subjective clinical experiences. In a recent article addressing this subject, the authors did not specify whether the sample comprised only successfully treated patients or consecutively affected patients from their database, and they reported 100% success.
The aims of our study were to assess success rates and durations of the orthodontic-surgical modality of treatment of impacted maxillary central incisors in a group of consecutively treated patients and to examine factors that may influence these parameters to give accurate information to patients and parents.
Material and methods
The treatment records of 60 consecutive patients with 64 impacted incisors were gathered between 2002 to 2007 from the orthodontic department of Hebrew University in Jerusalem and from the private practices of the 2 senior authors (S.C. and A.B.). The project was approved by the institutional review board.
The inclusion criteria were (1) impacted maxillary central incisors in healthy subjects; (2) a combined orthodontic-surgical approach by one of the 2 senior authors using the same treatment; (3) regular attendance for orthodontic appointments, as determined from the clinical notes; and (4) complete patient records, including diagnostic and treatment entries, pretreatment diagnostically essential radiographic views (good quality panoramic, periapical, and cone-beam computed tomography images that were not available for the older patients), banding and bonding date, debanding and debonding date, date of surgical exposure, and date of full engagement of the impacted incisor bracket in the first plain stainless steel archwire. Subjects with craniofacial syndromes, cysts, or cleft lip or palate were excluded from the study.
The diagnosis of impaction was made on the basis of a clinical examination and diagnostic plane radiographs. In each patient, the diagnosis was confirmed at the time of the surgical exposure by the orthodontist, who was routinely present for this.
Treatment usually followed the order we have described elsewhere. It commenced with anchorage preparation. In most patients, an updated version of Johnson’s twin appliance was used to avoid bonding deciduous teeth that were likely to be shed during treatment. Anchorage was provided by a palatal arch with or without a Nance button, and brackets were placed only on the erupted incisors. After orthodontic leveling, aligning, and reopening of the incisor space, a small attachment was bonded by the orthodontist to the exposed tooth at the end of the surgical procedure if a closed eruption procedure was performed, or within a few days thereafter in case of open surgery. Traction was applied immediately to the freshly bonded attachment. The tooth was brought to its place in the arch by light orthodontic extrusive traction maintained by the ligature wire.
In patients with a classic dilaceration, 2 surgical exposures were usually required. The first was a closed procedure, and the second was an apically repositioned flap, open surgical procedure. This second surgery was needed to prevent the incisal edge of the incisor from breaking through the oral mucosa as it was rotated in the buccolingual plane; this was intended to encourage the emergence of the impacted tooth crown through the attached gingiva.
The main outcome variables were the success rate and the duration of the orthodontic treatment.
Treatment was considered successful if the incisor was brought into its place in the arch. The success rate was determined on the basis of the posttreatment records. The success rate was calculated as the percentage of successfully aligned incisors relative to the total number of incisors treated.
This stage of treatment was specifically aimed for resolution of the impacted central incisor and was completed when the incisor was properly aligned in the arch.
When more comprehensive treatment was considered, only that part of the treatment surrounding the resolution of the incisor was considered, but in general, the treatment of other features of the malocclusion was postponed until the patient was ready for a phase 2 protocol.
The length of treatment in months was determined from each patient’s records.
Total treatment time refers to the period between bonding or banding and debonding or debanding of the orthodontic appliances, and this was arbitrarily divided into 3 constituent treatment periods.
- 1.
T1, from the date of bonding or banding to the date of the surgical exposure. In this preliminary or preparatory stage, bonding or banding was performed, anchorage was prepared, and space was opened for the impacted tooth.
- 2.
T2, from the date of the surgical exposure to the date that the tooth was fully ligated in the main arch with a nickel-titanium wire. This was the traction stage.
- 3.
T3, from the full ligation into the stainless steel wire to the date of debonding or debanding. During this finishing stage, more complex movements such as rotations, uprighting, and torquing were performed.
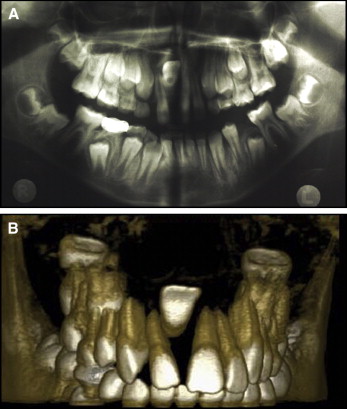
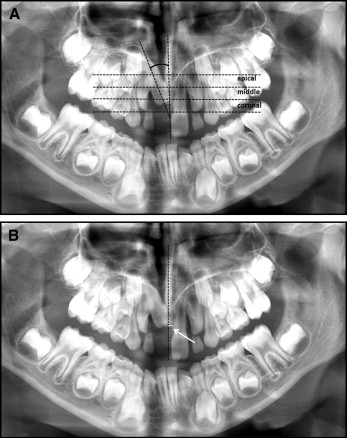
Success rate and duration of treatment were classified as follows: (1) age, younger group (<11 years) or older group (≥11 years); (2) sex; (3) etiology of impaction, trauma, classic dilaceration (crown angulated labially relative to the root, with the palatal aspect facing labially, Fig 1 ), obstruction of the path of eruption (supernumerary, odontoma), or unknown; (4) angulation of the impacted tooth to the midline ( Fig 2 , A ), measured on panoramic views as the angle between the long axis of the impacted tooth and the midline drawn perpendicular to the occlusal plane through the anterior nasal spine; this parameter was omitted in the subjects with dilaceration; the cutoff angle of 20° was based on the median angulation value of the whole group, except for the subjects with dilaceration: <20° or ≥20°; (5) vertical crown height ( Fig 2 , A ), assessed in the panoramic views only for unilateral cases, at the level of the apical third of the root of the adjacent erupted central incisor, the middle third of the root of the adjacent erupted central incisor, and the coronal third of the root of the adjacent erupted central incisor; (6) distance of the impacted tooth to the midline ( Fig 2 , B ), measured on panoramic views as the distance between the most mesial part of the crown of the impacted tooth and the midline, ≤0 mm (the crown crosses the midline) or >0 mm; and (7) type of surgical exposure: open, closed, or combined (closed at the first exposure, open at the second exposure).
According to previous articles, different head positions have little influence on angular and linear measurements if changes in the position of the occlusal plane are equal to or less than 10°.
Statistical analysis
The statistical methods for the associations between each variable, the success rate, and the treatment duration included chi-square tests and logistic regression analyses using SAS software (version 9.4; SAS Institute, Cary, NC) to calculate odds ratios and 95% confidence intervals. A multivariate regression model including 7 categorical variables was performed to identify the factors with a significant impact. All unilateral sides but only 1 side of the bilateral subjects were included in the multivariate analysis. The inclusion of each side as a separate case in the bilateral subjects was discounted because they are not independent variables. The side was chosen at random by the statistician, so that both affected sides had an even probability to be included in the analysis. All statistical tests were 2-sided at α = 0.05.
Results
The patients’ characteristics are presented in Table I . The mean age of the whole group was 19.3 ± 2.5 years, with an age range of 7.0 to 21.9 years. The age groups comprised 33 patients in the young group (mean, 9.0 ± 1 years) and 27 in the older group (mean, 12.2 ± 1.6 years). Twenty-six patients were male, and 34 were female.
| Characteristic | No. of patients (no. of incisors) |
|---|---|
| Age (y) | |
| Younger | 33 (35) |
| Older | 27 (29) |
| Unilateral | 56 (56) |
| Bilateral | 4 (8) |
| Sex | |
| Male | 26 (29) |
| Female | 34 (35) |
| Etiology | |
| Trauma | 14 (15) |
| Classic dilaceration | 13 (13) |
| Obstruction | 29 (32) |
| Unknown | 4 (4) |
| Angulation (°) ∗ | |
| ≤20 | 13 (15) |
| >20 | 16 (17) |
| Height | |
| Apical | 32 (32) |
| Middle | 18 (18) |
| Coronal | 6 (6) |
| Distance to midline (mm) | |
| ≤0 | 31 (31) |
| >0 | 29 (33) |
| Surgical exposure | |
| Closed | 44 (48) |
| Open | 11 (11) |
| Combined | 5 (5) |
∗ This variable was examined only in patients with impacted incisors due to obstructive causes.
Most patients had unilateral impactions (56), and only 4 were affected bilaterally.
Fourteen patients had a history of trauma; however, most of the patients with classic dilacerations also reported trauma. Therefore, these 2 groups were combined for statistical purposes. In the statistical analysis, this group of 27 trauma-affected patients with or without dilaceration was compared with the group of 29 patients with obstructed incisors. In 4 patients, the specific etiology could not be determined.
The 2 subgroups based on angulation to the midline were much smaller because this parameter was examined only in the obstruction group because of the difficulty of drawing the long axis of the tooth in the subjects with dilaceration. The angulation range was 0° to 140°.
In the unilateral group, most of the incisors were at the level of the apical (32) or the middle (18) third of the adjacent erupted incisor. Only 6 were recorded as coronal, and these were therefore combined with the middle-third group for statistical purposes.
The mean distance of the impacted tooth to the midline was 1.4 ± 3.9 mm, with a range of −4 to 20 mm.
Most patients (44) were treated with a closed surgical exposure, and only 11 had an open procedure. A few patients (5), all with dilaceration, had 2 preplanned surgical procedures, initially closed, and then, as the tooth approached its location in the arch, an apically repositioned flap to invest the tooth with attached gingiva on its labial side. This group was added to the closed surgery group in the statistical analysis because most of the treatment was performed according to the closed surgery approach.
The prognosis (success rate) and the duration of the different stages of treatment are summarized in Table II .
| Variable | SR (%) | Tt (mo) | T1 (mo) | T2 (mo) | T3 (mo) |
|---|---|---|---|---|---|
| Age | 90.0 | 21.6 ± 8.7 | 4.9 ± 3.6 | 8.7 ± 4.4 | 8.2 ± 4.8 |
| Younger | 93.9 | 19.2 ± 13.0 | 4.1 ± 2.4 | 8.0 ± 4.6 | 7.5 ± 10.1 |
| Older | 85.2 | 25.8 ± 10.1 | 6.0 ± 4.1 | 9.6 ± 5.4 | 9.5 ± 5.2 |
| Sex (n) | |||||
| Male | 80.1 | 20.1 ± 8.8 | 5.5 ± 4.2 | 7.4 ± 3.3 | 7.7 ± 5.3 |
| Female | 97.1 | 21.0 ± 12.6 | 4.4 ± 2.5 | 9.6 ± 5.9 | 7.1 ± 6.7 |
| Etiology | |||||
| Trauma and dilaceration | 81.5 | 21.4 ± 8.8 | 5.6 ± 4.4 | 10.1 ± 5.5 | 5.7 ± 3.2 |
| Classic dilaceration ∗ | 69.2 | 22.1 ± 6.1 | 5.5 ± 2.8 | 10.8 ± 5.6 | 5.8 ± 3.4 |
| Obstruction | 96.6 | 18.0 ± 7.4 | 4.9 ± 3.2 | 7.0 ± 3.3 | 6.1 ± 4.6 |
| Unknown | 100 | 31.8 ± 15.5 | 5.5 ± 7.2 | 13.7 ± 7.6 | 12.5 ± 4.9 |
| Angulation (°) † | |||||
| ≤20 | – | 19.6 ± 8.7 | 7.8 ± 6.5 | 7.4 ± 3.1 | 4.4 ± 4.1 |
| >20 | – | 19.6 ± 5.2 | 6.1 ± 3.4 | 7.0 ± 3.2 | 6.5 ± 3.7 |
| Distance to midline (mm) | |||||
| ≤0 | 90.3 | 21.6 ± 10.1 | 5.5 ± 4.1 | 8.2 ± 3.6 | 7.6 ± 5.8 |
| >0 | 89.6 | 23.3 ± 15.1 | 4.8 ± 3.6 | 9.1 ± 6.1 | 9.3 ± 10.1 |
| Height | |||||
| Apical | 84.4 | 23.2 ± 15 | 4.8 ± 3.4 | 9.6 ± 5.0 | 8.7 ± 10.1 |
| Middle and coronal | 95.8 | 19.3 ± 10.1 | 4.9 ± 3.4 | 7.5 ± 5.0 | 6.9 ± 6.5 |
| Surgical exposure | |||||
| Closed and combined | 89.8 | 18.1 ± 8.8 | 5.0 ± 3.9 | 8.1 ± 4.1 | 7.8 ± 6.1 |
| Open | 90.9 | 23.6 ± 12.4 | 6.3 ± 3.5 | 11.6 ± 8.2 | 5.2 ± 4.8 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


