Loss of soft and hard tissue is common after tooth extraction. Substantial resorption of alveolar bone compromises esthetics and may result in prosthetic and surgical limitations. Immediate implant placement at the time of tooth extraction is used to maintain alveolar ridge dimensions. Clinical studies support the successful outcome of immediate placement of dental implants in fresh extraction sockets; comparative clinical studies have found that implant survival rates after immediate placement are similar to those after delayed placement. This article addresses surgical techniques for immediate implant placement and the prevention and the management of complications associated with this procedure.
Key points
- •
Clinical studies have reported successful outcome of immediate placement of dental implants in fresh extraction sockets.
- •
Although immediate implant placement has advantages over delayed implant placement, like any other procedure, it is associated with risks and complications.
- •
Case selection and evaluation of patient-related and implant-related factors are keys to the success of immediate implant placement.
- •
A thorough discussion between practitioner and the patient is indispensable to discern patient’s desires.
Introduction
Healing of Extraction Socket
Wound healing in an extraction socket is characterized by resorption of alveolar bone, which may result in restorative complications. Healing of extraction sites when no socket preservation techniques are used results in the resorption of an average of 1 to 2 mm of vertical alveolar bone height and an average of 4 to 5 mm of horizontal alveolar bone width. Most of this bone loss occurs during the first year after extraction, and two thirds of this bone loss occurs within the first 3 months after extraction. Therefore, preservation of alveolar bone immediately after tooth extraction has an important impact on the functional and esthetic outcomes of subsequent prosthetic treatment. The purpose of preserving the extraction socket is to maintain the architecture of the alveolar bone, prevent soft tissue collapse, and minimize or eliminate the need for future bone augmentation procedures.
Histologically, 4 important changes may occur during the 5 stages of normal healing of the extraction site: External dimensional changes at the extraction socket, internal dimensional changes within the extraction socket, dimensional changes in a damaged extraction socket, and dimensional changes in the mucosa. The first stage of healing is characterized by the formation of a blood clot as a coagulum of red and white blood cells. The second stage is characterized by the formation of granulation tissue, which replaces the clot over 4 to 5 days. The third stage is characterized by the formation of connective tissue, which replaces granulation tissue over 14 to 16 days. The fourth stage is characterized by the appearance of osteoid calcification, which begins at the base and the periphery of the socket (early osteoid calcification is present within 7–10 days, and trabecular bone fills the socket by 6 weeks). The fifth stage is characterized by complete epithelial closure of the socket after 24 to 35 days (bone filling occurs between 5 and 10 weeks, and complete filling occurs by 16 weeks). Maximum osteoblastic activity occurs within 4 to 6 weeks.
External dimensional changes at the extraction socket consist of horizontal or buccolingual ridge reduction of approximately 5 to 7 mm (almost 50% of the initial ridge width); this reduction occurs over a period of 6 to 12 months, although most of the changes occur during the first 3 months. Reduction in the apicocoronal or vertical height of 2.0 to 4.5 mm accompanies the horizontal change. Internal dimensional changes within extraction sockets, consisting of a reduction of 3 to 4 mm in the vertical height of the socket, or approximately 50% of the initial socket height, have been reported after 6 months of healing. Most of this bone loss occurs during the first 3 months after tooth extraction. Dimensional changes in damaged extraction sockets most likely consist of fibrous tissue that may occupy a portion of the socket, thereby preventing normal healing and osseous regeneration.
Elevating the flap after extraction may compromise the blood supply of the thin buccal plate, which has little or no cancellous bone, resulting in partial or complete resorption of the buccal plate. At the surgically treated tooth site (full-thickness flap elevation) in dogs, the mean amount of bone loss is 1.0 mm buccal and 0.1 mm lingual. Surface bone resorption has a more pronounced effect on the delicate buccal bone than on the lingual bone.
Fate of Buccal Bone
Buccal bone generally is thinner than lingual and palatal bone ( Fig. 1 ). The crest of the buccal bone is composed solely of bundle bone. Buccal dehiscence and fenestration of the buccal plate of socket are frequently present. There are 3 main sources of blood supply to the alveolar bone around teeth: The periodontal ligament blood vessels, the periosteal blood vessels, and the alveolar bone blood vessels. After tooth removal, 20% of the blood supply from periodontal ligament blood vessels is discontinued. If a flap is elevated on the buccal side, the periosteal blood supply will be discontinued for 4 to 6 days, until new anastomoses occur. The thin cortical bone buccal plate has no endosteal blood vessels; therefore, complete resorption of the buccal plate may occur if no socket preservation technique is used. Bone grafting is frequently used to prevent collapse and to minimize resorption of the thin buccal plate. However, no comparative clinical studies have evaluated the fate and stability of the buccal bone over time with or without bone regeneration.
Immediate Implant Placement
Immediate implant placement is defined as the placement of an implant into the extraction socket at the time of tooth extraction. Immediate loading is defined as the placement of full occlusal or incisal loading on a dental implant restoration. Immediate provisionalization is a clinical protocol for the placement of an interim prosthesis, either with occlusal contact with the opposing dentition (ie, immediate occlusal loading) or without such occlusal contact (ie, immediate nonocclusal loading) at the same clinical visit during which the implant is placed. Delayed loading refers to applying force on an implant at some point after initial placement; a prosthesis is attached or secured after a conventional healing period (for the maxilla, 3–4 months; for the mandible, 2–3 months). Early loading refers applying force on an implant after initial placement; a prosthesis is attached to the implant(s) before the end of the conventional healing period.
There is variation in the descriptive terminology used in the dental literature to describe the timing of implant placement. In 2004, Hammerle and colleagues published a consensus report containing a new classification system for the timing of implant placement. This classification is based on the structural changes that occur after extraction on and knowledge derived from clinical observations ( Table 1 ).
| Classification | Terminology | Time After Extraction | Clinical Findings |
|---|---|---|---|
| Type 1 | Immediate implant placement | Immediately | Fresh extraction socket |
| Type 2 | Early implant placement | 4–6 wk | Healed soft tissue |
| Type 3 | Delayed implant placement | 3–4 mo | Healed soft tissue and substantial bone healing |
| Type 4 | Late implant placement | >4 mo | Completely healed bone |
Introduction
Healing of Extraction Socket
Wound healing in an extraction socket is characterized by resorption of alveolar bone, which may result in restorative complications. Healing of extraction sites when no socket preservation techniques are used results in the resorption of an average of 1 to 2 mm of vertical alveolar bone height and an average of 4 to 5 mm of horizontal alveolar bone width. Most of this bone loss occurs during the first year after extraction, and two thirds of this bone loss occurs within the first 3 months after extraction. Therefore, preservation of alveolar bone immediately after tooth extraction has an important impact on the functional and esthetic outcomes of subsequent prosthetic treatment. The purpose of preserving the extraction socket is to maintain the architecture of the alveolar bone, prevent soft tissue collapse, and minimize or eliminate the need for future bone augmentation procedures.
Histologically, 4 important changes may occur during the 5 stages of normal healing of the extraction site: External dimensional changes at the extraction socket, internal dimensional changes within the extraction socket, dimensional changes in a damaged extraction socket, and dimensional changes in the mucosa. The first stage of healing is characterized by the formation of a blood clot as a coagulum of red and white blood cells. The second stage is characterized by the formation of granulation tissue, which replaces the clot over 4 to 5 days. The third stage is characterized by the formation of connective tissue, which replaces granulation tissue over 14 to 16 days. The fourth stage is characterized by the appearance of osteoid calcification, which begins at the base and the periphery of the socket (early osteoid calcification is present within 7–10 days, and trabecular bone fills the socket by 6 weeks). The fifth stage is characterized by complete epithelial closure of the socket after 24 to 35 days (bone filling occurs between 5 and 10 weeks, and complete filling occurs by 16 weeks). Maximum osteoblastic activity occurs within 4 to 6 weeks.
External dimensional changes at the extraction socket consist of horizontal or buccolingual ridge reduction of approximately 5 to 7 mm (almost 50% of the initial ridge width); this reduction occurs over a period of 6 to 12 months, although most of the changes occur during the first 3 months. Reduction in the apicocoronal or vertical height of 2.0 to 4.5 mm accompanies the horizontal change. Internal dimensional changes within extraction sockets, consisting of a reduction of 3 to 4 mm in the vertical height of the socket, or approximately 50% of the initial socket height, have been reported after 6 months of healing. Most of this bone loss occurs during the first 3 months after tooth extraction. Dimensional changes in damaged extraction sockets most likely consist of fibrous tissue that may occupy a portion of the socket, thereby preventing normal healing and osseous regeneration.
Elevating the flap after extraction may compromise the blood supply of the thin buccal plate, which has little or no cancellous bone, resulting in partial or complete resorption of the buccal plate. At the surgically treated tooth site (full-thickness flap elevation) in dogs, the mean amount of bone loss is 1.0 mm buccal and 0.1 mm lingual. Surface bone resorption has a more pronounced effect on the delicate buccal bone than on the lingual bone.
Fate of Buccal Bone
Buccal bone generally is thinner than lingual and palatal bone ( Fig. 1 ). The crest of the buccal bone is composed solely of bundle bone. Buccal dehiscence and fenestration of the buccal plate of socket are frequently present. There are 3 main sources of blood supply to the alveolar bone around teeth: The periodontal ligament blood vessels, the periosteal blood vessels, and the alveolar bone blood vessels. After tooth removal, 20% of the blood supply from periodontal ligament blood vessels is discontinued. If a flap is elevated on the buccal side, the periosteal blood supply will be discontinued for 4 to 6 days, until new anastomoses occur. The thin cortical bone buccal plate has no endosteal blood vessels; therefore, complete resorption of the buccal plate may occur if no socket preservation technique is used. Bone grafting is frequently used to prevent collapse and to minimize resorption of the thin buccal plate. However, no comparative clinical studies have evaluated the fate and stability of the buccal bone over time with or without bone regeneration.
Immediate Implant Placement
Immediate implant placement is defined as the placement of an implant into the extraction socket at the time of tooth extraction. Immediate loading is defined as the placement of full occlusal or incisal loading on a dental implant restoration. Immediate provisionalization is a clinical protocol for the placement of an interim prosthesis, either with occlusal contact with the opposing dentition (ie, immediate occlusal loading) or without such occlusal contact (ie, immediate nonocclusal loading) at the same clinical visit during which the implant is placed. Delayed loading refers to applying force on an implant at some point after initial placement; a prosthesis is attached or secured after a conventional healing period (for the maxilla, 3–4 months; for the mandible, 2–3 months). Early loading refers applying force on an implant after initial placement; a prosthesis is attached to the implant(s) before the end of the conventional healing period.
There is variation in the descriptive terminology used in the dental literature to describe the timing of implant placement. In 2004, Hammerle and colleagues published a consensus report containing a new classification system for the timing of implant placement. This classification is based on the structural changes that occur after extraction on and knowledge derived from clinical observations ( Table 1 ).
| Classification | Terminology | Time After Extraction | Clinical Findings |
|---|---|---|---|
| Type 1 | Immediate implant placement | Immediately | Fresh extraction socket |
| Type 2 | Early implant placement | 4–6 wk | Healed soft tissue |
| Type 3 | Delayed implant placement | 3–4 mo | Healed soft tissue and substantial bone healing |
| Type 4 | Late implant placement | >4 mo | Completely healed bone |
Outcome and advantages of immediate implant placement
Several retrospective, prospective, and randomized, controlled clinical studies have evaluated the clinical outcome of immediate placement of an implant in an extraction socket. Generally, clinical studies reported similar short-term and long-term survival rates (1–7 years) for immediate and delayed implant placement. As reported by Lang and associates, the survival rate of immediate implants is 97.3% to 99%. The effect of apical pathology on the survival of an implant immediately placed in an extraction socket is debatable. Some studies have found that the survival rates for implants placed immediately into infected sockets and those for implants placed in noninfected socket or healed ridges are similar.
Traditional guidelines have stressed the need for complete healing of the alveolar bone before an implant is placed into a fresh extraction socket, a process that usually requires several months. This lengthy undisturbed healing period extends the time of oral functional disability and substantial resorption of the alveolar ridge may occur. Shanaman and Denissen and co-workers reported that the dimensions of the alveolar ridge can be maintained after immediate implant placement, whereas Werbitt and Goldberg reported that soft tissue preservation is optimal after immediate implant placement. Immediate implant placement may reduce the number of operative interventions required and the treatment time. The ideal orientation of the implant may be achieved. Preserving the architecture of the hard and soft tissues at the extraction site may provide optimal restorative esthetics ( Table 2 ).
| Advantages | Disadvantages |
|---|---|
| One surgical procedure | Surgically demanding; complex procedure |
| Less treatment time | Risk of marginal mucosal recession |
| Preservation of bone at extraction site | Adjunct connective tissue graft |
| Reduction in cost | Adjunct bone graft or guided bone regeneration |
Guidelines for immediate implant placement
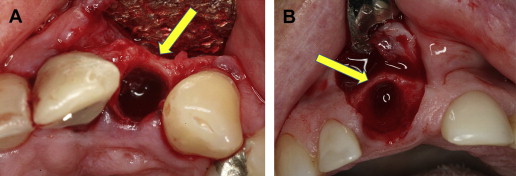
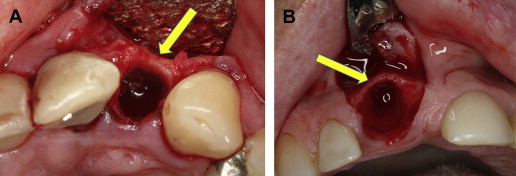
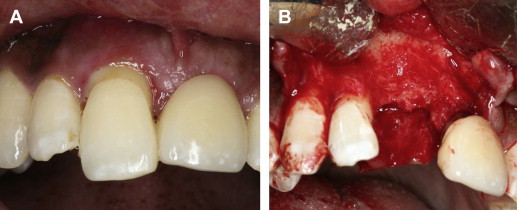
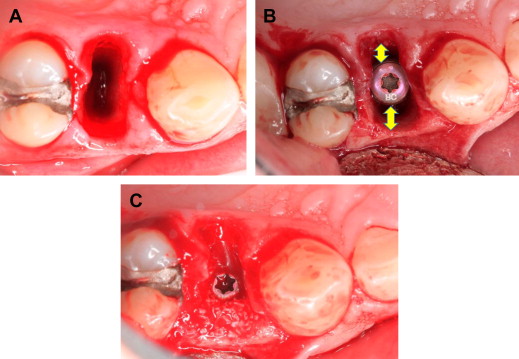
Several indications suggest that immediate placement may be an appropriate procedure with good oral hygiene; the presence of a single failing tooth with good adjacent dentition; the presence of adequate and harmonious gingival architecture with the surrounding dentition; adequate bone volume to accommodate an implant, with minimum dimensions of 3.5 × 10 mm and without the need for bone grafting; no dental trauma affecting the alveolar bone; osseous-level dental decay without purulence; and endodontic failure without periapical infection, a residual nonrestorable root, or root fracture ( Fig. 2 ). On the other hand, the following are contraindications for immediate placement: Active infection, lack of bone beyond the apex, a close relationship to anatomic vital structures (ie, mandibular canal, maxillary sinus, nasal cavity), dental history of bruxism, parafunctional habits, lack of stable posterior occlusion, perforation or loss of the labial bony plate after tooth removal, and inability to achieve primary stability ( Fig. 3 ). The most predictable method of successful immediate implant placement are maintenance of the soft tissue architecture with conservative tissue manipulation (ie, leaving the periosteum intact) to preserve the blood supply, maintenance of the buccal plate, and firm implant stability with a minimum torque value of 30 Ncm and an implant stability quotient of at least 60 ( Box 1 ).
- •
Low-risk patient
- •
Low esthetic expectations
- •
Adequate quality and quantity of soft tissue
- •
Adequate quality and quantity of socket bone
- •
Absence of diffuse infection
- •
Healthy condition of adjacent teeth and supporting structures
- •
Primary stability
Micromovement
Micromovement caused by load peaks higher than friction hold is crucial. Micromovement of the implant can grind and slowly smooth the bone surface, thereby reducing the interlock between bone and titanium and ultimately resulting in a loss of primary stability. It is critical that there are no occlusal implant overloads during the early healing stage. Primary stability is important during the first days after implant installation. The first weeks are a crucial period because primary stability can decrease to critical levels before secondary stability develops. Any micromotion of more than 150 μm causes fibrous encapsulation of the implant. Therefore, patients should be compliant and should avoid high masticatory forces by eating only soft foods for at least for 6 weeks postoperatively.
Horizontal Bone Defect (Jumping Distance)
A horizontal bone defect is defined as the longest distance in a perpendicular direction from the implant surface to the socket wall. In 2003, Botticelli and associates introduced the term jumping distance at implant sites with a horizontal defect dimension; the jumping distance is the horizontal distance between the implant surface and the surrounding bony wall of the socket.
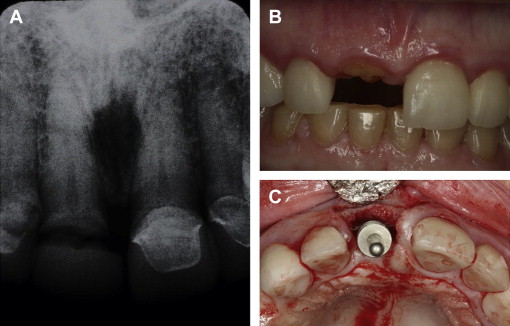
The need for bone grafting and the use of a barrier after immediate implant placement depend on the thickness of the labial plate and the size of the gap between the implant and the adjacent alveolar bone. Although a thick labial plate is generally resistant to resorption and grafting is unnecessary, bone grafting is frequently used to prevent collapse and minimize resorption of the thin labial plate, regardless of the gap size. Bone grafting aids in osteoconduction of osteogenic cells by preserving space and promoting the formation of new bone (the scaffold effect). Human and animal studies have shown that, in implant sites with an horizontal defect dimension of 2 mm or less, spontaneous bone regeneration and osseointegration with adequate bone-to-implant contact can occur; however, if the horizontal defect dimension is larger than 2 mm, the use of a barrier membrane with or without membrane-supporting bone grafting material is warranted for achieving adequate bone-to-implant contact and proper osseointegration. Botticelli and colleagues reported that no bone grafting is needed even if the jumping distance is greater than 2 mm. In a case report study, Tarnow and colleagues concluded that no bone graft, membrane, or primary closure is necessary for filling the jumping distance, provided that the buccal plate is intact after extraction ( Fig. 4 ).
Submerged or Transmucosal Implant Placement
The submerged placement protocol was introduced by Brånemark and colleagues. With this approach, the implant is sealed from the outer environment by the mucosa, and this sealing may decrease the chances of implant contamination. However, several publications of clinical trials using the transmucosal approach for immediate implant placement reported successful outcome.
Tapered or Parallel Side Implant Design
Tapered design implants were used in several clinical studies, and were reported with high success and survival rates in the immediate implant protocol. Because tapered implants are narrow apically and wide coronally, they have the advantage of filling the gap between the implant body and the socket wall at the crest level. It also improves the implant’s primary stability, avoiding buccal wall engagement in the anterior region, and reducing the need for jumping distance augmentation. McAllister and associates reported safe and effective application after using variable thread tapered implants. Although the difference was not significant, Sanz and colleagues reported less vertical and horizontal space using tapered implants than of cylindrical implants after immediate implant placements. However, Lang and colleagues found in a clinical trial that both cylindrical and tapered implants have shown similar short-term outcomes with regard to wound healing and primary stability. Bone augmentation at the time of implant placement was required for both designs in transmucosal placement approach.
Rough Surface
Increased surface roughness of an implant can help to improve primary stability. In a clinical study involving 1925 immediate implants placed from 1988 to 2004, Wagenberg and Froum reported a higher success rate for immediate implants with rough surface than for immediate implants with machined surfaces.
Implant Design
The effect of the design of the implant collar or neck placed immediately after the tooth extraction on the peri-implant soft and hard tissues has been explored in several experimental studies. They reported that implants with roughened and microthreaded neck would cause less resorption of the crestal bone than implants with roughened and not microthreaded neck. These studies are in agreement with 1 clinical study involving delayed implant placement, which showed less marginal bone resorption around roughened and microthreaded neck than of machined neck. The use of tapered platform-switched internal connection implants at the implant shoulder is recommended for immediate implant placement, because these implants can allow rapid rehabilitation with no adverse impact on implant survival.
Guidelines for provisionalization and loading
The outcome of conventional implant loading is predictable in all clinical situations. It is highly recommended in instances of poor primary implant stability, substantial bone augmentation, small-diameter implants, and compromised host conditions.
Achieving primary stability is the key factor in the success of dental implants. Insertion torque is among the methods used for clinical assessment of primary stability. Insertion torque is the amount of torque required to place the dental implant into the prepared osteotomy. With the introduction of newer dental implant systems, various manufacturers have recommended different insertion torques: Low insertion torque, moderate insertion torque, and high insertion torque (32–70 Ncm). Ottoni and colleagues compared immediate-loading implants (test group) that were restored within 24 hours with a provisional crown and conventional-loading implants (control group) after healing. A minimal insertion torque of 20 Ncm was standard for attaining primary stability. The insertion torque was associated with the risk of implant failure for the test group but not for the control group, in which 9 implants failed when the insertion torque was 20 Ncm. The authors concluded that an initial insertion torque of greater than 32 Ncm is necessary for immediate loading of a dental implant with provisional restoration. Furthermore, adding 9.8 Ncm to the insertion torque decreases the risk of implant failure by 20%. Atieh and colleagues investigated the influence of insertion torque (32, 50, or 70 Ncm) and stress distribution on wide-diameter, tapered oral implants placed immediately in extraction sockets of mandibular molars. The authors found that the use of moderate insertion torque (32–50 Ncm) may reduce the risk of implant failure in an extraction socket. Furthermore, they found that the highest insertion torque of 70 Ncm introduced substantial stress and should be avoided during immediate placement of an implant into a fresh extraction socket. The use of higher insertion torque is linked to the introduction of stresses to the bone. These stresses can directly affect the stability of the dental implant or hinder the process of osseointegration by inducing micromovements, which can lead to failure. Cannizzaro and colleagues used the split-mouth design to investigate the effect of medium insertion torque (25–35 Ncm) and high insertion torque (>80 Ncm) on single implants with immediate loading placed without flaps into 50 patients. The patients were observed for 6 months after initial loading. Osseointegration failed for 7 implants placed with medium insertion torque (between 25 and 35 Ncm). On the other hand, none of the implants placed with insertion torque higher than 35 Ncm failed. The authors concluded that single implants with immediate loading should be placed with a higher insertion torque so that early implant failure can be prevented.
Marginal bone loss around immediately loaded implants is comparable with that associated with conventionally loaded implants. Ericsson and colleagues reported crestal bone loss of 0.14 mm for immediate implant loading and 0.07 mm for conventional implant loading. Recent systematic reviews reported that immediate loading is associated with significantly less bone loss than conventional loading.
Early implant failure can be minimized by avoiding lower insertion torque, especially for an implant associated with immediate or early loading. Immediate and early loading require high insertion torque (30–35 Ncm), an implant stability quotient of at least 60, and minimal implant length (≥10 mm), as well as the absence of contraindications such as parafunctional activities, large bone defects, and the need for sinus floor elevation.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


