Fig. 7.1
(a) Left portrait: age 34 years 8 months pretreatment (b). Patient portrait: 35 years 3 months postsurgery. The surgical improvement was dramatic and involved maxillary impaction, mandibular autorotation, and bilateral sagittal split osteotomy for mandibular advancement as well as advancement genioplasty (Reprinted with permission from Handelman and Greene [2]). (c) Cephalometric superimposition on Nasion-Basion line at Basion. Presurgery: 34 years 8 months solid line and 35 years 3 months dotted line. Note: soft tissue advancement of lower lip and chin. This improvement would not be possible limited surgery to the maxilla. (d) Panorex: age 34 years 8 months. Note: minimal size of condyles [2]
7.5 Pathology of the Condyle Undergoing Resorption
The TMJ condyle is covered with a layer of fibrocartilage. During ICR/PCR this tissue breaks down, and then the outer osseous cortex of the condyle starts to resorb [8, 9]. This is seen on imaging as resorption lacunae, with the disappearance of the dense outer cortical layer. Other changes include narrowing as well as shortening of the condylar process and ultimately there are changes in the length of the ramus [8]. There is demineralization of the bone below the cortex of the condyle. This may result in the collapse of articular surface bone, which is clinically manifested by a rapid opening of the bite and opening rotation of the mandible [9]. Although the disease is described as condylar resorption, there may also be resorptive changes occurring in the articular eminence which tends to flatten [3, 9]. ICR/PCR can affect either one or both condyles; if unilateral, the result is significant facial asymmetry. However, in most cases both condyles are involved, although one joint may demonstrate more advanced pathology than the other. This more common bilateral pattern may indicate a genetic predisposition as well as the humoral nature of the etiology. Hatcher has illustrated both the resorptive stages and the eventual healing stages of condylar resorption visualized on CBCT imaging (Fig. 7.2) [26].
Fig. 7.2
Imaging stages of ICR/PCR; CBCT TMJ images at top and associated anatomic illustrations below. Image A – normal TMJ: Band C, the destructive stage; B and E, the repair stage; F, the stable stage (Reprinted with permission from Hatcher [26])
7.6 The Role of the TMJ Disc in Development of ICR/PCR
The TMJ disc acts as a shock absorber during load bearing mandibular movements, while also providing lubricated surfaces over which translation and rotation movements occur [11, 27]. The role of the disc in the etiology of ICR/PCR is controversial in terms of “chicken-and-egg” explanations. The functional surfaces of both the condyle and the articular eminence can demonstrate degenerative changes when the disc is perforated or displaced without reduction [28, 29]. Link and Nickerson studied patients referred for orthognathic surgery and reported that all their open bite cases and 88 % of their Class II malocclusions had bilateral disc displacement [30]. On the other hand, the condyles undergoing resorption simply may not be able to maintain normal disc position, so the discs may become displaced. Wolford and Cardenas recommend joint surgery to attach the displaced disc to the head of the condyle prior to or during orthognathic surgery for ICR/PCR to prevent reoccurrence of disc displacement or changes in disc morphology [31]. Other surgeons do not agree that disc surgery is necessary. They do not enter the joint when performing orthognathic surgery on ICR/PCR patients, especially if the joint is functional – even if the condyle and ramus are severely affected by the disease (Figs. 7.1 and 7.3) [3, 13]. It should be remembered that TMJ disc displacement occurs in about 1/3 of asymptomatic individuals in the random population, while ICR/PCR is a relatively rare occurrence [2, 32]. Also, patients with degenerative joint disease of the TMJ do not necessarily have abnormally positioned discs [32].
Fig. 7.3
Series of cephalometric images of a patient with severe ICR/PCR. All x-rays are superimposed on the Nasion-Basion line at Basion. Articulare moves forward due to resorption on the anterior aspect of the condyle. (a) Cephalometric superimposition from pre-orthodontic treatment 10 years, 3 months (solid line) to postorthodontic treatment at 13 years (dashed line). Note at age 10 years 3 months future ICR/PCR could not be predicted. The maxilla grew normally, while the mandible grew vertically but not anteriorly. The mandible rotated down and back, and articulare moved mesially. (b) Cephalometric superimposition of postorthodontic treatment from age 13 (solid line) to 14 years (dashed line). The maxilla grew normally, while the mandible rotated downward and backward, causing an open bite with an increased overjet. Articulare moved forward. (c) Cephalometric superimposition from age 14 years (solid line) to 15 years, 10 months (dashed line). The maxilla has stabilized as growth has ceased. However, the mandible continued its downward and backward rotation and regression, with shortening of the ramus. (d) Cephalometric superimposition from 15 years, 10 months (solid line) to 30 years, 6 months (dashed line). The condylar resorption has continued with shortening of the ramus and mesial movement of articulare. (e) Cephalometric superimposition from 18 years, 6 months (solid line) to 30 years, 10 months (dashed line). The condyle continued to resorb with a downward and backward rotation of the mandible
7.7 Survey of Orthodontists About ICR/PCR
Author CH mailed a questionnaire in 1998 regarding ICR/PCR experience to a group of orthodontists who were members of the Midwest component of the Edward H. Angle Society and faculty of the orthodontic department at the University of Illinois, Chicago [2]. From a total of 69 mailings there were 57 responses, and these practitioners reported seeing only 56 cases of ICR/PCR during their years in practice. An incidence of ICR/PCR of approximately 1 per 5,000 patients was derived by estimating the number of new patients examined over the years in each practice. Another way of looking at the rarity of the incidence was that each provider saw an average of 1.3 ICR cases in his/her career up to the point of the survey. This incidence may be low due to failure to recognize the disease, and small sample size, but it does demonstrate the infrequency of ICR/PCR seen in an orthodontic practice. Surgery centers that perform a large number of orthognathic procedures have reported an incidence of 2–5 %, which is still infrequent, but more common than reported by the orthodontists [15–19].
Of the 56 cases of ICR/PCR recorded in this survey, 35 (62.5 %) were spontaneous with no history of surgery, while 21 (37.5 %) developed the problem following surgery. The following data were derived from 40 of the questionnaires where there was adequate reporting:
-
The ICR/PCR group was comprised of 38 (95 %) females and 2 males who were brothers. There were 37 (92.5 %) whites, 3 Asians, and no blacks in the group.
-
Of the 40 cases, 33 (82.5 %) were reported to be bilateral and 7 were unilateral.
-
The incidence of TMJ or facial pain was 12 (30.7 %) out of 39 cases.
-
The malocclusions before ICR/PCR were diagnosed, 14 (35 %) Class I, 1 (2.5 %) Class I open bite, 12 (30 %) Class II, 12 (30 %) Class II open bite, and 1 unclassified.
-
Severity of the ICR/PCR as rated by the respondents was one case mild, while 39 were described as severe or extreme.
From the responses, it is clear that these were patients that the orthodontist remembered well. This survey should be repeated with a greater number of orthodontic offices participating. However, even these limited findings confirm the anecdotal reports in the literature that ICR/PCR is a disease affecting young females of Caucasian or Asian descent, less than half presenting with TMJ pain, and with variable occlusions prior to developing this problem, and when ICR/PCR does occur it presents as a severe management problem.
7.8 Diagnosis of the ICR/PCR Patient
7.8.1 History
A careful history can reveal the probable diagnosis of ICR/PCR. A report of a sudden change in occlusion is nearly pathognomonic of ICR/PCR. Unfortunately, this change may occur during orthodontic treatment, when it easily can be misinterpreted as being due to unfavorable growth, tongue thrust, or poor cooperation. Or it might initially be regarded as an adverse response to treatment mechanics.
A history of autoimmune and collagen diseases should be part of the historical questioning [5]. Referral to a physician for rheumatoid factor serology should be considered, although this is usually negative in patients with ICR/PCR. A history of TMJ discomfort and disc displacement is an important factor, since a number of ICR/PCR patients report pain or other TMD symptoms and have displaced discs on imaging [2, 30]. When pain is reported, this may be an indication that the disease is active.
A family history of rheumatoid disease, TMD, and open bite malocclusion should be recorded even though there has been no report of familial incidence of ICR/PCR. A history of facial trauma, especially when the TMJ is involved, is important as a possible cause of condylar resorption [5]. Fortunately, only rarely does a trauma case evolve into ICR/PCR.
Orthodontic treatment and third molar extractions have been indicted as possible causes of ICR/PCR [10, 13]. Statistics indicate that this is a very rare disease and a large percentage of the young have had orthodontic treatment and/or third molar removal. Therefore, it is problematic to assign etiology of a rare disease to a common experience. However, in those rare subjects whose condyles are undergoing an early, often undetected, stage of ICR/PCR, orthodontic treatment, and/or third molar extractions may overwhelm the adaptive capacity of their vulnerable condyles.
Young female orthognathic surgery patients who have developed ICR/PCR prior to surgery have been reported to exhibit a history of irregular menstrual cycles, amenorrhea, or oral contraceptive use according to Gunson et al. [7] They suggest that mid-cycle serum levels of 17 beta-estradiol should be measured, because low levels were associated with postsurgical development of severe condylar resorption.
7.8.2 Orthopantogram and Lateral Cephalometric Radiographs
The orthopantogram (OPG) can be used for the gross examination of condylar anatomy. The condyle will appear to have lost mass relative to the rest of the mandible, and appear thin or shortened with flattening of the superior and/or anterior curvature [3]. In many cases, the condylar neck will have a distal inclination [3, 19, 21].
Lateral cephalometric imaging will show mandibular divergence relative to the cranial base and maxilla, shortened posterior facial height, and increased anterior facial height with an increase in the overjet and negative overbite. Sagittal measures for the skeletal Class II relationship will be increased. Serial cephalometric imaging is diagnostic for active ICR. There are many choices for lateral cephalometric superimposition of the films, but the method used in the tracings in this chapter superimposes on the Basion-Nasion plane at Basion (Fig. 7.3). The posterior shadow of the condyle on this plane is defined as articulare. Its location will reposition medially when ICR is active. The mandible on the succeeding cephalometric images will reveal a clockwise rotation, a shortened posterior height (articulare to gonion) and length (Fig. 7.4). One limitation of cephalometric imaging is that it is frequently difficult to visualize the shadow of the head of the condyle in advanced ICR/PCR subjects because of the resorption, thus the more convenient use of articulare.
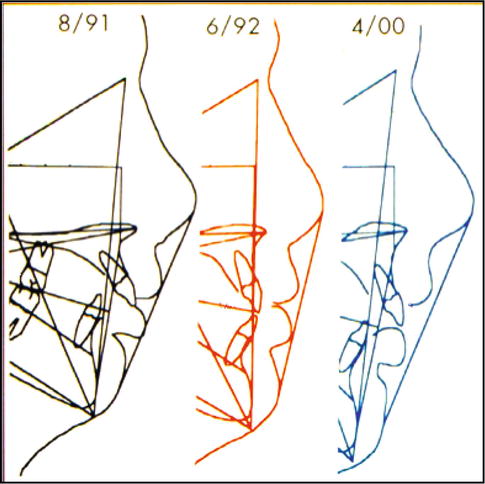
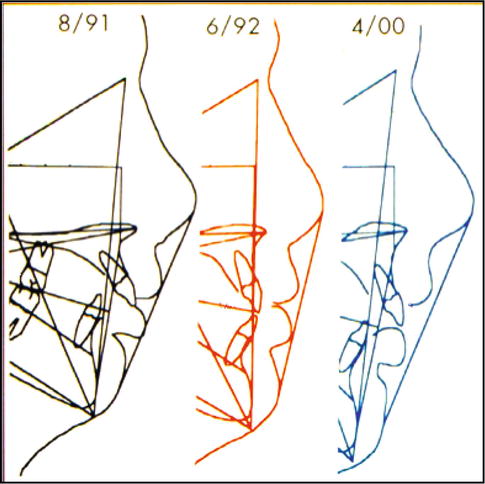
Fig. 7.4
Cephalometric tracing of postsurgical relapse. The left, 15 years 7 months, presurgery; the middle 16 years 5 months showing mandibular advancement for correction; the right 23 years 4 months showing 100 % relapse of the correction (Courtesy of Dr. John Russell, Mobile AL)
7.8.3 Cone Beam Computed Tomography (CBCT)
While CBCT has increased radiation and cost relative to OPG and cephalometric imaging, it is clearly justified because of its clarity and the avoidance of superimposition of adjacent structures. This enhances the clinician’s ability to see detailed pathologic features of the condyle such as disappearance of the dense outer cortical layer, erosions, sclerosis, flattening and sub-cortical cyst formation (Fig. 7.2) [26, 34]. Prior to CBCT, tomograms of the joint were useful, but they were not three-dimensional, providing only sagittal cuts in one or more planes of space. Both tomograms and CBCT are made in the open and closed mouth position. Both can be useful to follow the progress of ICR/PCR and to determine when the disease is in remission. Radiologists look for the healing of the outer cortical layer [26, 34]. A second CBCT scan taken 1 year after the first should demonstrate a healed and stable joint prior to considering surgery. Also, superimposition of cephalometric images should demonstrate no change in mandibular position during this period.
Unfortunately, a healed joint does not necessarily mean the disease will not reactivate. It has been demonstrated that orthognathic surgery can reactivate the resorption processes [3, 4, 21, 25]. Figure 7.3 illustrates a case carefully followed with tomograms. ICR onset was at age 13 and the condyles were healed by age 16. However, orthognathic surgery performed at this age reactivated the ICR/PCR, resulting in 100% bony relapse.
The appearance of an osteophyte on the anterior aspect of the condyle is associated with ICR/PCR and other degenerative joint diseases (Fig. 7.2). However, this finding is thought to represent the healing of the condyle as it attempts to increase its bearing surface to distribute the joint loads [26, 34].
7.8.4 Radioisotope Diagnosis
The value of performing a radioisotope study as part of the diagnosis of ICR/PCR is disputed. Some believe that the resultant technicium-99 nuclear medicine scan is difficult to interpret, since various other TMJ conditions will also demonstrate high levels of isotope uptake, while others are of the opinion it does have some diagnostic value [25, 33].
7.8.5 Magnetic Resonance Imaging (MRI)
MRI is useful in the examination of the soft tissues of the TMJ such as the cartilaginous integrity of the condylar head surface, articular disc position and condition, joint effusion and marrow edema [35]. However, it does not provide diagnostic images of the bony cortices of the condyle or eminence that are clearly defined by a tomogram or a CBCT scan.
7.8.6 Occlusal Splints: Diagnostic Aspects
Occlusal orthotic splints are suggested as a joint stabilizing modality in ICR/PCR cases when there is joint pain and dysfunction as well as before orthognathic surgery [36]. An often overlooked use is its potential as a diagnostic tool for determining cessation of the resorptive process. Patients suspected of having ICR/PCR should be fitted with a maxillary occlusal splint with contact registered on all the mandibular teeth. If the lower incisors no longer register contact at a future evaluation, this indicates further joint degeneration and active disease [1, 2]. A maxillary occlusal splint should routinely be placed following orthognathic surgery/orthodontic treatment at the time of retention for TMJ comfort, reduction of the forces on the joint, and to evaluate stability of the correction [1, 2, 36].
7.9 Timing and Surgical Options for Correction of ICR/PCR
The role of the orthodontist prior to orthognathic surgery is to prepare upper and lower teeth to an ideal arch form that will maximize occlusal contact in a normal Class I occlusion following surgery. This is true no matter which surgical approach is taken. A limited number of ICR/PCR cases can be successfully treated following remission of the disease by orthodontic means, without performing surgery. This is especially true when the resorption starts in the 20s rather than in the early teens (Fig. 7.5). These patients may have acceptable aesthetics, but this is not the situation in many cases. The tremendous loss of condylar mass and the resulting facial deformity in most cases requires comprehensive surgical management (Fig. 7.1).


Fig. 7.5
Patient developed ICR/PCR at age 20 years and treated by orthodontic mechanics only. (a) Pretreatment portrait and intraoral photographs at age 26 years 4 months. Note favorable profile despite anterior open bite. (b) Tomograms at age 26 years 11 months demonstrate reduced size of condyles due to resorption from the superior surfaces, signs of flattening and erosions. A small osteophyte extends from the anterior surfaces. The radiologist diagnosed degenerative joint disease that was no longer active, so orthodontic treatment was started. (c) Postorthodontic treatment portrait and inter oral photographs were taken at age 33 years 2 months with the patient 5 years into retention. Note stability of the closure of the anterior open bite
ICR/PCR typically first appears in young adolescents, although Dibbets et al. has shown deformed condyles and growth disturbances in a younger age group [37]. The period from the teen years to the early 20s appears to be the most active time for ICR/PCR. Optimistically, the disease goes into remission and eventually “burns out” by the mid 20s. However, some patients continue to have active ICR/PCR into their 30s (Fig. 7.3). As a result, teenagers diagnosed with ICR/PCR should be advised to postpone orthognathic surgery, young girls with severe facial deformity and/or their parents often insist on correction earlier due to social and peer related pressures.
Another option available is to advance the mandible slowly by distraction osteogenesis, thereby allowing the soft tissue and musculature to adapt to the large mandibular advancements often required in such cases. Schendel et al. reported a case of 15.6 mm vertical elongation and 13.4 mm horizontal advancement using a curved distractor [40].
Gunson and Arnett have taken a more biomedical and pharmacologic approach in the management of patients with ICR/PCR or who might be at risk of postsurgical ICR/PCR [36]. They prescribe an occlusal splint employed for 6 months prior to as well as following orthognathic surgery to reduce the mechanical loads on the joint. Also, before and after surgery they place the patient on a comprehensive series of drugs to relax the musculature, decrease bruxism, decrease inflammation and reduce the patient’s inherent bone resorption capacity [10, 36, 41]. They reported stable postorthognathic surgery results at 24-month follow-up in 24 ICR/PCR patients (American Society of TMJ Surgeons, May 2,3, 2014, Chicago, IL).
The approach to the management of ICR/PCR cases should be individualized and based on the extent of the disease process. Arnett’s and Gunson’s approach appears appropriate for most early cases of ICR/PCR requiring orthognathic surgical management. For cases requiring extreme mandibular advancements, distraction osteogenesis might be considered [38].
If condylar resorption is still active, replacement of the joint with an autologous costochondral graft or total alloplastic temporomandibular joint replacement prosthesis is possible [25, 40–45]. There are a number of ICR/PCR patients who present with one of the following problems, who are best treated with synthetic total joint replacement (TJR). They are individuals with:
Patients with active ICR/PCR may also be candidates for total joint replacement as the artificial joint cannot resorb. The next section will discuss this option in detail.
7.10 Rationale for the Use of TMJ TJR in the Surgical Management of End-Stage ICR/PCR
End-stage disease is the most pernicious condition of an organ or disease state; in this state the organ can barely function. Examples include end-stage renal disease where the kidneys have shut down and the patient requires dialysis, or end-stage cardiac disease where the heart is functioning so poorly that it requires mechanical support or transplantation for the patient to survive [45].
End-stage joint disease portends a joint so architecturally devastated by disease or injury that it results in a severe functional impairment for the patient. In the ICR/PCR patient, the local adaptive capacity of the TMJ condyle has been mechanically and biologically tested in vivo by the disease process and it has failed. This failure is demonstrated by the load-compromised bony architecture having end-stage pathological changes as seen on imaging. Clinically, the articular end-stage pathology is manifested by the patient’s signs and symptoms [41–45].
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


