Introduction
There is little agreement on the expected duration of a course of orthodontic treatment; however, a consensus appears to have emerged that fixed appliance treatment is overly lengthy. This has spawned numerous novel approaches directed at reducing the duration of treatment, occasionally with an acceptance that occlusal outcomes may be compromised. The aim of this study was to determine the mean duration and the number of visits required for comprehensive orthodontic treatment involving fixed appliances.
Methods
Multiple electronic databases were searched with no language restrictions, authors were contacted as required, and reference lists of potentially relevant studies were screened. Randomized controlled trials and nonrandomized prospective studies concerning fixed appliance treatment with treatment duration as an outcome measure were included. Data extraction and quality assessment were performed independently and in duplicate.
Results
Twenty-five studies were included after screening: 20 randomized controlled trials and 5 controlled clinical trials. Twenty-two studies were eligible for meta-analysis after quality assessment. The mean treatment duration derived from the 22 included studies involving 1089 participants was 19.9 months (95% confidence interval, 19.58, 20.22 months). Sensitivity analyses were carried out including 3 additional studies, resulting in average duration of treatment of 20.02 months (95% confidence interval, 19.71, 20.32 months) based on data from 1211 participants. The mean number of required visits derived from 5 studies was 17.81 (95% confidence interval, 15.47, 20.15 visits).
Conclusions
Based on prospective studies carried out in university settings, comprehensive orthodontic treatment on average requires less than 2 years to complete.
Highlights
- •
The quest to reduce treatment duration has intensified in recent years.
- •
Notwithstanding this, the mean expected treatment duration has been unclear.
- •
On the basis of this review, a mean treatment time on the order of 20 months appears to be typical.
- •
The relative merits of measures to hasten orthodontic treatment should be balanced against this yardstick.
It is accepted that comprehensive orthodontic treatment is lengthy; the time frame is largely dictated by the biologic principles underpinning optimal tooth movement. There has been a lack of clarity concerning the typical duration of treatment. In a previous review that included observational studies, the authors were unable to arrive at an overall estimate of treatment duration. In spite of this lack of a clear yardstick, there has been a seemingly relentless drive among orthodontists and general dentists to reduce the duration of orthodontic treatment. Modern adjuncts directed at hastening treatment include newer technologies and novel surgical procedures, but some clinicians also resort to eschewing integral treatment phases in an effort to reduce treatment times.
Excessive treatment duration has been linked to a greater susceptibility to iatrogenic consequences of appliance therapy, primarily root resorption and plaque-induced conditions, including demineralization. Moreover, patient compliance and oral health–related quality of life may be impaired by longer treatment, particularly in adults. Shorter treatment times may, therefore, theoretically offer advantages to both treatment providers and patients, although shorter treatment is not without significant potential disadvantages.
For providers of care, there may be financial incentives in delivering more efficient treatment, most likely associated with fewer visits and shorter chairside times. However, potential financial gain may be tempered by the necessity for prolonged and diligent retention associated with the placement of teeth in inherently unstable positions with limited torque expression when the objectives of treatment are confined to the alignment of anterior teeth in isolation.
Novel approaches, involving various degrees of financial outlay and theoretical risk, have included expensive vibratory appliances and adjunctive surgical procedures to expedite tooth movement. Both, however, appear to be largely unproven; a randomized trial failed to identify an increase in the rate of orthodontic alignment in conjunction with a well-marketed, nonsurgical adjunct involving vibratory stimulation. Moreover, a recent Cochrane review highlighted a lack of evidence to support the use of surgical adjuncts at this stage, with only 4 clinical trials incorporating a total of just 57 patients. Furthermore, patient perceptions of surgically assisted orthodontics are not all favorable, especially when given the alternative of other noninvasive techniques.
It is therefore increasingly important that there is an appreciation of the expected length of orthodontic treatment before routinely embarking on treatment involving compromised objectives or adjunctive procedures, particularly with the lack of evidence underpinning these approaches. The aim of our review was to determine the duration of orthodontic treatment with fixed appliances.
Material and methods
The protocol for this systematic review was registered on PROSPERO international prospective register of systematic reviews ( www.crd.york.ac.uk/prospero ; protocol, l CRD42014014983). The following inclusion and exclusion criteria were used.
- 1.
Study design. Randomized and prospective nonrandomized studies carried out in primary or secondary care or in the community were to be included. Studies with short follow-up periods not including the duration of orthodontic treatment and retrospective studies were excluded.
- 2.
Participants. Patients of any age with complete-arch, fixed, bonded orthodontic appliances followed until the end of treatment were to be included. Patients with craniofacial syndromes and cleft lip or palate were excluded.
- 3.
Interventions and comparators. Any treatment intervention involving comprehensive, complete-arch, fixed orthodontic appliances without adjunctive use of removable or functional appliances was included. Patients undergoing treatment involving fixed appliances with surgical interventions including surgical exposure of ectopic teeth were excluded. Interceptive orthodontic interventions were also excluded. Since this was an epidemiologic review, no between-group comparisons were planned.
- 4.
Outcome measures. These were the duration of orthodontic treatment (months) from appliance placement to removal and the number of visits.
Search strategy for identification of studies
Comprehensive electronic database searches were undertaken without language restrictions as follows: MEDLINE via OVID (to November 2014, Appendix ), the Cochrane Oral Health Group’s Trials Register (November 2014), and the Cochrane Central Register of Controlled Trials (CENTRAL, the Cochrane Library Issue 3, 2014). Unpublished literature was accessed electronically through ClinicalTrials.gov ( www.clinicaltrials.gov ) and the National Research Register ( www.controlled-trials.com ) using the term orthodontic . In addition, efforts were made to obtain conference proceedings and abstracts, with authors contacted to identify unpublished or ongoing clinical trials. Reference lists of included studies were screened for additional relevant research.
Assessment of relevance, validity, and data extraction
Data were extracted independently and in duplicate by 2 authors (A.T., S.Y.C.) using prepiloted data extraction forms. The investigators were not blinded to the authors or the results of the research, and any disagreements were resolved by discussion with a third author (P.S.F.). The following information was recorded where available: (1) year of publication and study setting; (2) participants: sample size, age, and sex; (3) type of intervention; (4) type of control; and (5) outcomes: treatment duration (including means and standard deviations in months, where available) and number of visits (means).
Authors were contacted to clarify data as required, including information on treatment duration.
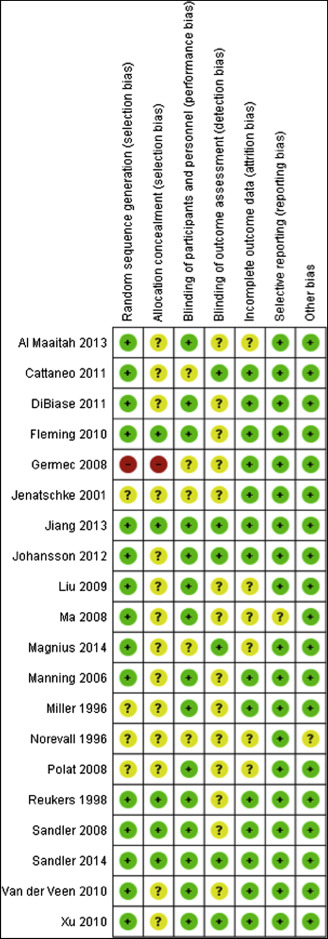
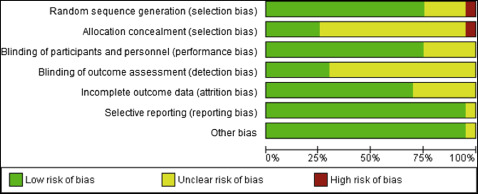
The quality of the eligible trials was assessed independently and in duplicate by 2 authors (A.T., S.Y.C.), and any disagreements were resolved by discussion with a third reviewer (P.S.F.). The Cochrane Collaboration’s risk of bias tool was used to assess risk of bias for randomized controlled trials (RCTs), and the Newcastle-Ottawa scale was used for the nonrandomized studies. The following domains were assessed as being at low, high, or unclear risk of bias for the RCTs: sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias) and outcome assessors (detection bias), incomplete outcome data addressed (attrition bias), selective outcome reporting (reporting bias), and other biases. An overall assessment of risk of bias (high, unclear, low) was made for each included trial. Studies with at least 1 criterion considered to be at high risk of bias were considered to be at high risk of bias overall and excluded from the primary analysis. The nonrandomized studies were judged on 3 broad perspectives consisting of 8 domains: selection of the study groups, comparability of the groups, and ascertainment of the outcome of interest. A star system was used in which high-quality studies could receive a maximum of 9 stars. A rating of 5 stars or fewer signified low quality. Studies at high risk of bias and low quality were excluded from the primary meta-analysis.
Statistical analysis
Clinical heterogeneity of the included studies was analyzed by reviewing the treatment interventions and protocol, including participants and settings, appliance designs, and use of extractions or additional procedures. Statistical heterogeneity was assessed based on a graphic display of the estimated treatment durations in conjunction with 95% confidence intervals. A weighted estimate of treatment duration was calculated from the included studies. Sensitivity analyses were planned at the outset to address studies at higher risk of bias and other potential sources of heterogeneity including overriding effects of large studies and differences in outcomes related to specific treatments (eg, extraction vs nonextraction), study setting (primary or secondary care), or patient groups (adults over 18 years vs adolescents). Meta-analyses and sensitivity analyses were undertaken with Stata software (StataCorp, College Station, Tex) using metan and metareg commands.
Results
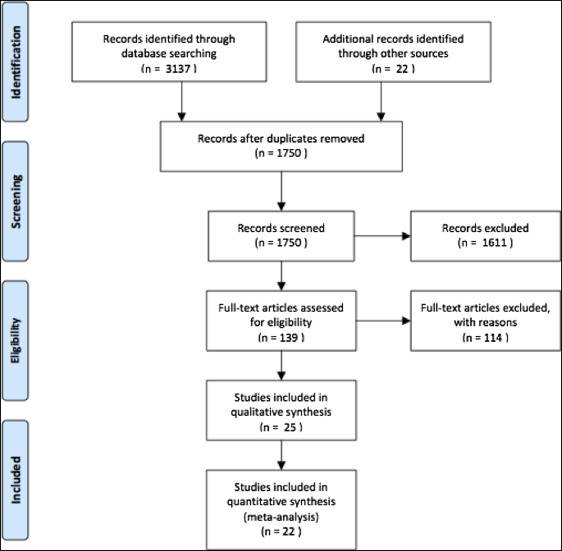
The search returned 1728 studies after removal of duplicates. All abstracts were reviewed, and 139 potentially relevant articles were retrieved in full. Additional screening of reference lists returned another 22 articles for review. After a detailed assessment, which included contacting the relevant authors for further clarification of data relating to treatment duration, 114 studies were excluded ( Appendix ), and 25 remained ( Fig 1 ; Table ). Twenty studies were RCTs, and 5 were controlled clinical trials (CCTs). All included studies were carried out in a university or hospital setting. Among the primary studies, other primary outcomes of interest other than estimates of overall treatment duration, included bracket failure rates, prevalence of decalcification, and occlusal outcomes.
| Study | Design | Participants | Intervention/comparison | Extraction (yes/no) | Adults/young people (<18 y) |
|---|---|---|---|---|---|
| Al Maaitah, 2013 | RCT split mouth | N = 34: 204 brackets SEP and 204 brackets conventional etch. Each group split in ≤17 y and >17 y. Overall mean age, 18.7 y; range, 12-26 y; sex, 13 M, 21 F | SEP vs conventional etch | No | Both |
| Banks, 2000 | CCT | N = 94: 49 fluoride- releasing modules (782 teeth) and 45 nonfluoride-releasing modules (740 teeth). Overall mean age, 16 y | Fluoride-releasing modules vs nonfluoride- releasing modules | No | Both |
| Borsos, 2012 | CCT | N = 30: 15 palatal implant (PI) and 15 transpalatal arch (TPA). Overall mean age, 14.22 ± 1.37 y | PI vs TPA | Yes | Young |
| Cattaneo, 2011 | RCT | N = 41: 20 active ligation In-Ovation R and 21 passive ligation Damon 3 MX | In-Ovation R (active) vs Damon 3 MX (passive) self-ligation | No | Both |
| DiBiase, 2011 | RCT | N = 48: 27 Damon 3 and 21 Synthesis. Overall mean age, 16.2 y; sex, 32 M, 30 F initially | Damon 3 self-ligation vs Synthesis conventional ligation | Yes | Both |
| Fleming, 2010 | RCT | N = 54: 28 SmartClip self-ligation and 26 Victory conventional ligation. Mean overall age, 15.81 ± 2.58 y; sex, 18 M, 36 F | SmartClip self-ligation vs Victory conventional ligation | Yes | Both |
| Germec, 2008 | RCT | N = 26: 13 extraction and 13 nonextraction | Extraction vs air rotor stripping | Yes | Both |
| Jenatschke, 2001 | RCT (feasibly study) | N = 33: 18 chlorhexidine varnish (CHX) and 15 placebo varnish. Median overall age, 15 y; range, 11-18 y | CHX varnish vs placebo varnish group | Unclear | Both |
| Jiang, 2013 | RCT | N = 95: 48 acidulated phosphate fluoride (APF) and 47 placebo | 1.23% APF vs placebo | Unclear | Young |
| Johansson, 2012 | RCT | N = 90: 44 Time 2 self ligation (SL) and 46 Gemini conventional edgewise (CE). Overall age range, 11.7-18.2 y | Time2 SL vs Gemini CE | No | Both |
| Jung, 2013 | CCT | N = 66: 34 orthodontic mini-implant (OMI) with intreproximal stripping (IPS) and 32 second premolar extraction. Overall age range, 17-44 y | OMI + IPR vs extraction | Yes | Adults |
| Liu, 2009 | RCT | N = 34: 17 mini-implant and 17 TPA. Sex, 6 M, 28 F | Mini-implant vs TPA | Yes | Both |
| Ma, 2008 | RCT | N = 30: 15 mini-implant and 15 headgear (HG). Overall age range, 18-22 y; sex, 16 M, 14 F | Mini-implant vs HG | Yes | Adults |
| Magnius, 2014 | RCT split mouth | N = 46 (836 teeth): 416 teeth pumice and 416 teeth prophy paste. Overall mean age, 14.1 ± 1.4 y; sex, 17 M, 29 F | Oil-free pumice vs prophy paste | Yes | Young |
| Manning, 2006 | RCT | N = 34: 17 (299 bonds) SEP and 17 (298 bonds) Transbond conventional adhesive | SEP vs conventional adhesive (Transbond) | Yes | Young |
| Miller, 1996 | RCT | N = 17: 9 GIC and 8 composite bracket adhesive | GIC vs resin adhesive | Unclear | Young |
| Millett, 1999 | CCT split mouth | N = 40 (240 brackets): 120 brackets GIC and 120 resin. Overall mean age, 13.4 ± 2 y; sex, 17 M, 23 F | GIC vs resin adhesive | Unclear | Young |
| Millett, 2000 | CCT split mouth | N = 45 (426 brackets): 213 compomer and 213 resin adhesive. Overall median age, 14.4 y, range, 13.7-15.5 y; sex, 13 M, 32 F | Compomer vs resin adhesive | No | Young |
| Norevall, 1996 | RCT split mouth | N = 60: 30 machine cut grooves bracket base and 30 mesh foil bracket base; 492 teeth Aquacem (GIC) and 493 Unite (resin). Overall mean age, 13.56 ± 1.57 y; sex, 21 M, 39 F | GIC vs acrylic resin | Yes | Young |
| Polat, 2008 | RCT | N = 20: 10 In-Ovation SL and 10 conventional preadusted edgewise (CPAE) | SL vs CPAE | No | Young |
| Reukers, 1998 | RCT | N = 61: 32 fully programmed appliance (FPA) and 29 partly programmed appliance (PPA). Overall mean age, 12.4 ± 1.2 y | FPA SWA (0.022-in slot) vs PPA (0.018-in slot) conventional edgewise | Yes | Young |
| Sandler, 2008 | RCT | N = 51: 26 palatal implant (PI) and 25 headgear (HG). Overall mean age, 15.2 y; range, 12-39 y; sex, 13 M, 38 F | PI vs HG | Yes | Young |
| Sandler, 2014 | RCT | N = 71 0.22 TADs, 26 Nance, and 23 HG. Overall mean age, 14.22 ± 1.46 y | TADs vs Nance palatal arch vs HG | Yes | Young |
| Van der Veen, 2010 | RCT split mouth | N = 28: 14 buccal appliances maxilla with lingual mandible and 14 lingual appliances maxilla with buccal appliances mandible. Overall mean age, 15.3 ± 1.2 y | Buccal vs lingual appliances | Unclear | Both |
| Xu, 2010 | RCT | N = 63: 32 en-masse retraction and 31 2-step retraction. Sex, 24 M, 39 F | En-masse retraction vs 2-step retraction | Unclear | Young |
The generation of a random number sequence was considered adequate in 15 trials, with only 1 study considered at high risk of bias ( Figs 2 and 3 ). Five studies were judged to have adequate allocation concealment, with allocation concealment not clearly reported in most studies. Blinding of the clinicians and patients to the intervention was not possible in many studies because of the nature of the research. Blinding of outcome assessors was possible; however, this was clearly undertaken in only 6 studies and was unclear in the remaining 14 RCTs. Overall, most of the included RCTs were deemed to be at low or unclear risk of bias. With regard to the CCTs, 4 studies were judged to be of good quality using the Newcastle-Ottawa scale (8-9 stars). One CCT was deemed to be of low quality ( Fig 4 ).