Hemostasis is an integral and very important aspect of surgical practice. As a rule, most bleeding from dental surgery can be controlled by pressure. When the application of pressure does not yield satisfactory results, or where more effective hemostasis is required, hemostatic agents are used. These agents act to stop bleeding either mechanically or by augmenting the coagulation cascade. Some of the newer agents that are available to the dental profession have been presented.
Bleeding during surgery is a serious clinical problem that can be very disconcerting to the patient and could have serious consequences. During the course of nearly all types of surgery, blood vessels will be disrupted, causing some bleeding, but in the dental setting, this is usually easily controlled. In oral surgery, pressure is commonly used to control bleeding, and this is successful in most cases. In major oral and maxillofacial surgical procedures electrocautery and suture ligatures are most commonly used to control bleeding from small and major vessels. At times, however, where generalized oozing is present and the use of pressure is not effective, and the use of electrosurgical instruments could endanger teeth or nerves, topical hemostatic agents may be needed.
During the recent military conflicts, particularly Iraq, there have been significant advances in hemostatic materials that have proved to be very effective in hemorrhage control on the battlefield. Several of these products are now being adapted for civilian use, and now there is a multibillion dollar hemostasis market with new products and solutions rapidly emerging. This article presents some of these products that are useful for oral surgery or that may become useful. Although the emphasis will be on agents that may be used within the oral cavity, the article will also describe agents that could be useful to oral and maxillofacial surgeons.
The authors hope that the reader will not be lulled into believing that hemostatic agents will become the panacea to the control of surgical hemorrhage. The most important step to always remember in bleeding control is direct pressure, and hemostatic agents should always be considered secondarily. The dentist should be familiar with the general techniques of hemorrhage control for different types of bleeding episodes—small vessels, large vessels, oozing, drug-induced, or when an underlying coagulation defect is present.
Having a general knowledge of the coagulation process will allow the clinician to better understand how the hemostatic agents work and when they should be applied. Hemostatic agents provide control of external bleeding by enhancing or accelerating the natural clotting process through various physical reactions between the agent and blood.
Hemostasis
-
The process of hemostasis is a very complex one that involves 3 major steps: (1) vasoconstriction, (2) formation of a platelet plug, and (3) coagulation (secondary hemostasis).
The first step is an immediate constriction of damaged blood vessels caused by vasoconstrictive paracrine released by the endothelium. This results in a temporary decrease in blood flow within the injured vessel. The second step is a mechanical blockage of the defect by a plug that forms as platelets stick to the exposed collagen (platelet adhesion) and become activated, releasing cytokines (serotonin, thromboxane A2, and endothelin1) into the area around the injury. Released platelet factors (ADP, fibronectin, thrombospondin, fibrinogen and PDGF) reinforce the vasoconstriction and activate more platelets that stick to one another (platelet aggregation) to form the platelet plug. At the same time, exposed collagen and tissue factor initiate the third step, a series of reactions known as the coagulation cascade that ends in the formation of fibrin polymer. The fibrin protein fiber mesh reinforces and stabilizes the platelet plug to become a clot.
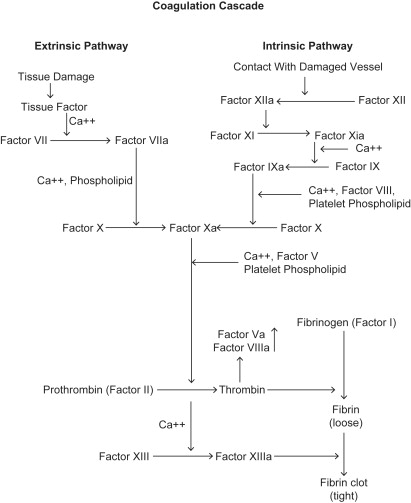
The clotting cascade (secondary hemostasis) is traditionally broken up into 2 basic pathways, the intrinsic pathway and the extrinsic pathway. The intrinsic pathway is primarily activated by collagen, which is exposed and binds factor 12 to initiate this cascade. The extrinsic pathway is stimulated by tissue factor, which is exposed by the tissue injury and through factor 7 activation initiates this pathway. These 2 pathways then converge in a common pathway where thrombin converts fibrinogen to fibrin and then the final clot.
Intrinsic Pathway (Contact Activation Pathway)
The intrinsic cascade is initiated when contact is made between blood and exposed negatively charged surfaces. Upon exposure of a negatively charged surface, prekallikrein, high molecular weight kininogen, and factors 12 and 11 initiate the intrinsic pathway. Upon contact activation, prekallikrein is converted to kallikrein, which activates factor 12 to 12a, which in turn activates factor 11 to 11a. With Ca+ present, factor 11a activates factor 9 to 9a, which cleaves factor 10 to 10a, the beginning of the common pathway. Contact activation of the intrinsic pathway can also occur on the surface of bacteria, and through the interaction with urate crystals, fatty acids, protoporphyrin, amyloid β, and homocysteine.
Extrinsic Pathway (Tissue Factor Pathway)
Factor 3 (tissue factor) is released from the tissue immediately after injury and initiates the extrinsic pathway. Factor 3 forms a complex with factor 7a, which catalyzes the activation of factor 10, which cleaves to become factor 10a.
Common Pathway
The intrinsic and extrinsic coagulation cascades converge at activated factor 10a, resulting in the conversion of prothrombin (factor 2) to thrombin (2a). Thrombin activation occurs on activated platelets. Thrombin then converts fibrinogen to fibrin monomers, activates factor 13 to 13a (transglutaminase), which then cross-link the monomers—with the aid of calcium—to form fibrin polymer and thus the clot Fig. 1 .
Hemostatic agents
A hemostatic agent (antihemorrhagic) is a substance that promotes hemostasis (ie, stops bleeding). These agents act to stop bleeding either mechanically or by augmenting the coagulation cascade. The ideal hemostatic agent should be effective, and the agent itself, along with its metabolic breakdown products, should be safe to use within the body. The locally acting hemostatic agents generally work by increasing the rate of vasoconstriction, sealing vessels/vascular channels, or by promoting platelet aggregation. Gelfoam (Pfizer Incorporated, NY, USA) and Surgicel (Ethicon Incorporated, Somerville, NJ, USA), which work proximally in the intrinsic coagulation pathway via contact activation, have been used in dentistry for many decades and remain the major hemostatic agents in oral surgery. Bone wax controls bleeding by mechanically sealing bleeding channels in cancellous bone. All three agents have been proven to be effective and safe. The authors will present other hemostatic agents that have recently been introduced.
Hemostatic agents
A hemostatic agent (antihemorrhagic) is a substance that promotes hemostasis (ie, stops bleeding). These agents act to stop bleeding either mechanically or by augmenting the coagulation cascade. The ideal hemostatic agent should be effective, and the agent itself, along with its metabolic breakdown products, should be safe to use within the body. The locally acting hemostatic agents generally work by increasing the rate of vasoconstriction, sealing vessels/vascular channels, or by promoting platelet aggregation. Gelfoam (Pfizer Incorporated, NY, USA) and Surgicel (Ethicon Incorporated, Somerville, NJ, USA), which work proximally in the intrinsic coagulation pathway via contact activation, have been used in dentistry for many decades and remain the major hemostatic agents in oral surgery. Bone wax controls bleeding by mechanically sealing bleeding channels in cancellous bone. All three agents have been proven to be effective and safe. The authors will present other hemostatic agents that have recently been introduced.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


