The geriatric population (age 65 and older) is the fastest growing segment nationally and globally. The large population will continue to increase because of baby boomers that have recently turned 65 years old. Within this cohort, there is much diversity in health, socioeconomic levels, education, and health beliefs. There is a decline in edentulism yet still there are oral health conditions that persist with age, such as caries, tooth loss, and increased needs for prosthodontic dental treatment. Several factors should be taken into account in geriatric prosthodontic care, including quality of life and psychosocial needs.
Key points
- •
The geriatric population size is increasing.
- •
In the 65-years and older cohort there is an increase in certain medical conditions that affect oral health.
- •
The utilization of dental services by the elderly depends on many factors, such as insurance, socioeconomic status, ethnicity, education, access, and perceived needs.
- •
A trend seen in the delivery of dental services to older people is an increased need for prosthodontic treatment.
- •
In the oral health care of geriatric patients there are multifactorial issues that must be taken into account. These are not only limited to dental techniques but also include risks, nutrition, quality of life, and psychosocial needs.
Introduction
The geriatric population is growing at a faster pace than any group globally. Common medical conditions have dental implications. Although edentulism rates are declining, there are still higher rates of tooth loss in the elderly due to caries, periodontal disease, and ability of the patient to perform oral hygiene care.
There is much diversity in lifestyles and beliefs of the elderly population. Because of this diversity, the delivery of geriatric prosthodontic care must consider several factors in the diagnosis, treatment planning, and delivery of dental treatment. Some barriers exist for the geriatric patient in access to care.
Introduction
The geriatric population is growing at a faster pace than any group globally. Common medical conditions have dental implications. Although edentulism rates are declining, there are still higher rates of tooth loss in the elderly due to caries, periodontal disease, and ability of the patient to perform oral hygiene care.
There is much diversity in lifestyles and beliefs of the elderly population. Because of this diversity, the delivery of geriatric prosthodontic care must consider several factors in the diagnosis, treatment planning, and delivery of dental treatment. Some barriers exist for the geriatric patient in access to care.
Aging trends
Baby boomers are a cohort that was born between the years of 1946 and 1964. The first baby boomers turned 65 years in 2011. It is estimated there will be 71.5 million people age 65 years and older by the year 2030. Currently, 1 in every 8, or 13.1% of the population, is an older American. Persons reaching age 65 have an average life expectancy of 83.8 years with women outliving men. Of geriatric populations, the 85 and older cohort is the fastest growing segment. With this increase in the 65 and older population there will continue to be oral health care needs. The demand for dental professionals knowledgeable in geriatric dentistry will be necessary.
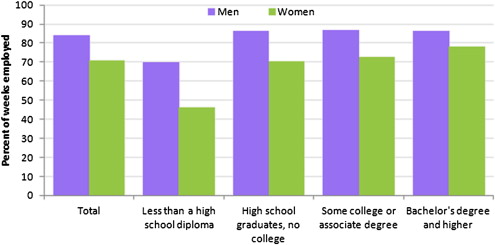
With the aging population there is much diversity in education and socioeconomic status. As the baby boomers continue to migrate to geriatric cohorts there will be changes in the labor workforce. There is a higher educational attainment in the baby boomer age group. The average person in latter baby boomer years was employed 78% of the weeks from age 18 to 46. Fig. 1 shows the percentage of weeks employed by educational attainment during years 1978 to 2010. There is a higher tendency for women who have attained higher educational levels to work more weeks. Men with higher educational attainment also worked more weeks. Educational attainment of less than high school diploma showed the fewest weeks employed for men and women.
With higher educational attainment levels, this will affect dental economics and what baby boomers consider important. A dentist who is keen on understanding population changes will certainly be more in tune to the needs of the elderly. A recent trend seen in the elderly is the use of Internet and social networking. According to the Pew Foundation, persons 65 years and older had an increase in Internet usage from 1% in 2006 to 33% elderly persons using the Internet in 2011. Internet sites visited most often were search engines, news, and government sites. Patient education is important in dentistry. If the geriatric population were increasingly using the Internet, this would be an excellent means to create dental educational web sites for geriatric patients.
Common medical conditions
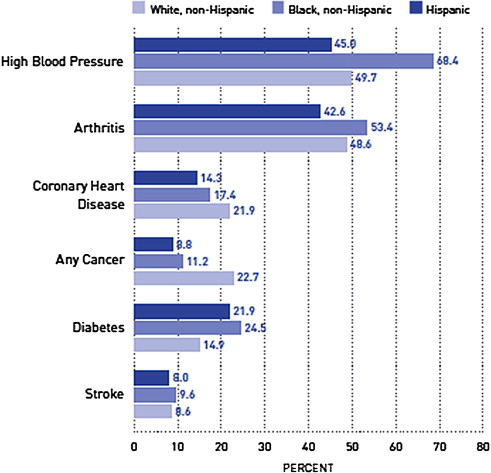
Despite higher educational attainment levels, geriatric populations have higher rates of comorbid diseases compared with younger cohorts. The most common medical conditions in the elderly are coronary heart disease, hypertension, cancer, arthritis, dementia, and traumatic injuries such as falls. Fig. 2 graphs the chronic medical conditions in the elderly according to ethnicity.
There is increasing scientific evidence in the medical and dental professions that oral health and systemic diseases are related. Periodontal disease induces an elevated systemic inflammatory status. Studies have shown that there is a relationship between periodontal disease and atherosclerotic disease, especially stroke. Diabetes is a risk factor for periodontal disease. Uncontrolled periodontal disease can aggravate diabetic complications. Controlled periodontal disease can improve glycemic control. Dental professionals should intercollaborate with medical professionals when systemic conditions influence oral health care.
Globally and nationally, the health of geriatric populations is a priority. The Department of Health and Human Services has recognized oral health and access to care as a leading indicator for overall health in the Healthy People 2020 objectives. The oral health section of Healthy People 2020 takes into account age, gender, educational attainment, socioeconomic status, race, and access to health insurance.
A new and major goal of Health People 2020 is to improve the health, function, and quality of life of older adults. Objectives very relevant to the elderly are
- •
Increase awareness of the importance to overall health and well-being
- •
Increase acceptance and adoption of effective prevention interventions
- •
Reduce disparities in access to effective preventive and dental treatment services.
The Fédération Dentaire Internationale World Dental Federation has collaborated with the World Health Organization and the International Association of Dental Research to review and revise global oral health goals, objectives, and targets. Like Healthy People, the target year is 2020. The objectives focus on reducing mortality from oral-facial disease, developing evidence-based policies and programs developing cost-effective prevention programs, and reducing oral health disparities. Box 1 summarizes the priority target conditions selected for the global oral health 2020.
-
Global Oral Health: priority target conditions selected by the Fédération Dentaire Internationale, World Health Organization, and International Association of Dental Research
- •
Pain
- •
Infectious diseases
- •
Oral HIV infection
- •
Trauma
- •
Dental caries
- •
Periodontal diseases
- •
Salivary gland disorders
- •
Health care services
- •
Functional disorders
- •
Oropharyngeal cancer
- •
Noma
- •
Craniofacial anomalies
- •
Developmental anomalies
- •
Oral mucosal diseases
- •
Tooth loss
- •
Health care information
As people become older, the correlation between oral health and general health is notable. Oral diseases have manifestations related to chronic systemic conditions. With age, there is an increase in medical conditions that require medication usage. The combination of systemic disease and medications can have a pronounced effect that can increase susceptibility to oral health disease. Another major factor is that with age it may become increasingly difficult to maintain good oral hygiene especially with medical conditions such as stroke or arthritis.
Dental utilization by the elderly
There is a range of dental utilization in the elderly due to the diversity of the population. With the increase in geriatric population size and longevity, there is an increased need for dental services. Factors that influence dental utilization are
- •
Socioeconomic status
- •
Educational attainment
- •
Insurance
- •
Health, health beliefs, and/or perceived needs
The elderly populations have increased rates of tooth loss, dental caries, periodontal disease, xerostomia, and oral cancer. Tooth loss or edentulism increases with age. In the 75-years and older cohort, approximately one-third are edentulous. Tooth loss or edentulism can result in psychosocial changes in a person’s life. Psychological conditions related to edentulism are depression, anxiety, and fear. The effects of edentulism play a major role in quality of life. Impact of edentulism in the elderly includes
- •
Speech
- •
Esthetics
- •
Function
- •
Nutritional deficiencies
- •
Psychological issues, self-image
- •
Quality of life
Frail elderly in long-term facilities can have difficulty obtaining dental services or access to services. As a result, oral health neglect is higher for institutionalized geriatric people that lead to increased tooth loss.
As the geriatric population increases, there are declining rates of edentulism. In 1971 the edentulism rate was approximately 50% for the elderly. In 2004, the edentulism rate had decreased to 23% of the elderly being edentulous. Higher rates of edentulism are found in Native Americans, followed by African Americans, then Caucasians, with Asians and Hispanics having the lowest edentulism rates.
With the increase in tooth retention is seen an increase of dental service utilization. In a 10-year longitudinal study, dentists 40 years and older benefited from an increase of 30.3% to 64.3% in patient visits, service, and expenditures. Healthy community-dwelling geriatric people have the largest increase in relative health spending. In 2010 dental service spending increased 2.3%. Out-of-pocket spending accounts for 40% of dental spending. Out-of-pocket spending in 2010 increased only 0.5%. In 2009, the average dental out-of-pocket expense was $873 and exceeded the average out-of-pocket prescription costs of $700. The 85-years and older cohort has the highest increased rates of dental prevention visits.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


