Introduction
This study evaluated the long-term stability of maxillary molar intrusion and anterior open-bite correction in adults treated by maxillary posterior teeth intrusion with zygomatic miniplates.
Methods
The sample included 26 skeletal anterior open-bite patients, who had maxillary posterior segment intrusion with zygomatic miniplates. Lateral cephalograms were taken at pretreatment, posttreatment, 1 year posttreatment, and 4 years posttreatment.
Results
The mean maxillary molar intrusion was 3.04 mm ( P ≤0.01), and the mean bite closure was 6.93 mm ( P ≤0.01). The intruded maxillary molars relapsed by 10.20% in the first year after treatment and by 13.37% by 4 years after treatment. Overbite relapsed by 8.19% and 11.18% after 1 year and 4 years posttreatment, respectively. The first year after treatment accounted for 76.29% and 73.2% of the total relapses of molar intrusion and overbite, respectively. The 4-year posttreatment relapse amounts of maxillary molar intrusion and overbite were positively correlated with the amount of pretreatment maxillary molar height and the initial open-bite severity, respectively, but negatively correlated with the amounts of maxillary molar intrusion and open-bite correction gained by treatment.
Conclusions
Molar intrusion with zygomatic miniplates appears to be stable 4 years after treatment.
Highlights
- •
Maxillary posterior teeth were intruded with zygomatic miniplates in adults.
- •
Long-term stability of intrusion and anterior open-bite correction were evaluated.
- •
Intruded maxillary molars relapsed by 10.2% in year 1 and 13.37% by year 4.
- •
Overbite relapsed by 8.19% in year 1 and 11.18% by year 4.
- •
Overcorrection of overbite and strict retention are recommended.
Anterior open bite has been considered a challenging malocclusion in treatment, especially in adults, and in retention, owing to its likelihood to relapse. The deformity is caused by combined influences from skeletal, dental, respiratory, neurologic, and habitual factors.
Skeletal anterior open bite is characterized by a steep mandibular plane, an obtuse gonial angle, and increased height of the lower third of the face. Generally, patients with an anterior open bite and a hyperdivergent skeletal pattern have excessive posterior vertical growth of the dentoalveolar complex in the maxilla, the mandible, or both.
Conventionally, treatment options for skeletal open bite in adults include the use of elastics combined with the multiloop edgewise archwire technique or nickel-titanium archwires. However, these mechanics cannot reduce the increased lower facial height of skeletal open bite in adults, since the open bite has been mainly masked by the extrusion of anterior teeth rather than by molar intrusion. Moreover, the extrusion of maxillary anterior teeth to close large open bites might compromise esthetic goals by causing excessive incisal and gingival display.
As a result, treatment of severe skeletal anterior open bite in adults consists chiefly of orthognathic surgery to reposition the maxilla, the mandible, or both. Stability of the open-bite correction was noted in approximately 75% to 85% of the patients treated with various surgical procedures. In addition, the long-term stability of surgical therapies for anterior open-bite correction was investigated in a meta-analysis and indicated 82% stability of the various surgical treatments, measured by positive overbite at 12 or more months after treatment. Despite the relative stability of the surgically corrected anterior open bite, complications, postoperative pain, edema, discomfort, hazards of general anesthesia, costs, and rehabilitation after surgery have made the surgical decision not usually preferred by most patients.
With the introduction of temporary anchorage devices, especially miniscrews and miniplates, intruding the molars into their bony support, producing mandibular autorotation and bite closure, finally is possible. It has been publicized that skeletal anchorage placed with a minor surgical intervention can achieve equivalent treatment results to those obtained by orthognathic surgery. Molar intrusion with skeletal anchorage has now become an accepted treatment protocol for treating skeletal anterior open-bite patients.
Only a few studies in addition to case reports have evaluated the stability of open-bite patients treated by intrusion of the posterior teeth with skeletal anchorage. Sugawara et al reported about a 30% relapse rate of intruded molars 1 year after treatment in a case series of 9 open-bite patients treated with mandibular molar intrusion. Lee and Park found a 10.36% relapse rate for intruded maxillary molars and an 18.1% relapse rate for overbite after a 17.4-month retention period in 11 adults. Baek et al found a maxillary molar relapse rate of 22.88% and an overbite relapse rate of 17% over a 3-year follow-up period in 9 open-bite patients. Deguchi et al noted approximately a 21.7% maxillary molar relapse rate and an overbite relapse rate of 13% after 2 years of retention in 15 female open-bite patients treated with miniscrews. Recently, Scheffler et al studied the stability of anterior open-bite treatment in 33 patients treated by intrusion of the maxillary posterior teeth with a maxillary occlusal splint and skeletal anchorage at 1 year and 2 or more years posttreatment. They concluded that 11% of their patients had greater than 2 mm of maxillary molar relapse after 1 year and 16% at 2 years. The same was true for the relapse in overbite: 15% of the patients had relapses in overbite greater than 1 mm after 1 year and 22% at 2 years, but none had more than a 2-mm change.
Most expert orthodontists can obtain a positive overbite of the teeth in anterior open bite with orthodontic treatment alone or combined with surgical intervention, but maintaining the vertical overlap can be problematic after treatment. Because of the susceptibility for relapse after any orthodontic correction, it is essential to evaluate further than the immediate posttreatment interval to determine long-term stability.
There are few reports with adequate numbers of subjects in long-term investigations of stability of maxillary molar intrusion with skeletal anchorage. Hence, this study was conducted to evaluate the 4-year posttreatment stability of maxillary molar intrusion and overbite correction in adults with anterior open bite treated by intrusion of the posterior teeth with zygomatic miniplates.
Material and methods
The sample size estimation was calculated for the difference in maxillary molar height based on a paired-samples t test using the software PS Power and Sample Size Calculations (version 3.0.43). The mean difference tested for was 1.5 mm. A more liberal standard deviation of the mean difference that was reported by Erverdi et al was used (σ = 2.5 mm), with type I error of 0.05 and power of 80%. The estimated sample size was 24 subjects.
An initial sample of 28 patients with skeletal anterior open bite was selected according to the following criteria.
- 1.
Patients with Angle Class I or Class II malocclusion, permanent dentition with anterior open bite (defined by cephalometric overbite measurement of at least −3 mm and a maximum of −8 mm), and age between 19 and 28 years.
- 2.
Maxillary posterior vertical dentoalveolar excess according to the analysis of Burstone et al. It was measured as the length of a perpendicular line from the maxillary first molar mesiobuccal cusp tip to the palatal plane (female, mean is 23 mm [SD, 1.3 mm]; male, mean is 26.2 mm [SD, 2 mm]).
- 3.
Acceptable or orthodontically correctable incisor-lip relationship.
All subjects were treated by the same orthodontist (E.S.M.) at the Department of Orthodontics, Faculty of Dentistry, Alexandria University in Egypt. Written informed consent was obtained from each subject before the study. Approval regarding the ethical concerns of this study was obtained from the ethical committee of the Faculty of Dentistry at Alexandria University.
The clinical technique used was described in more detail in a preliminary report. In brief summary, treatment was conducted with the standard edgewise technique using 0.022 × 0.028-in conventional brackets. Orthodontic leveling was carried out in 3 independent segments for the maxillary arch (1 anterior and 2 posterior).
When the maxillary segments were leveled with a 0.019 × 0.025-in stainless steel segment, the patients received a double transpalatal arch fabricated from 1.2-mm stainless steel round wire to counteract the buccal tipping of the molars during intrusion. It was placed 4 mm from the palate to create sufficient room to accommodate the posterior impaction ( Fig 1 , A ).
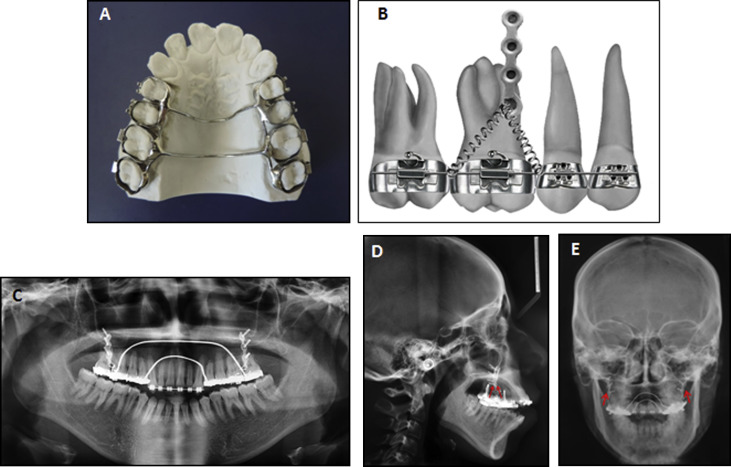
The patients were then referred for the surgical placement of the miniplates. All patients had titanium I-shaped multipurpose miniplates (Gebrüder Martin, Tuttlingen, Germany) fixed with 3 bone screws (Gebrüder Martin) 7 mm in length to the contour of the lower surface of each zygomatic buttress by the same surgeon. Maxillary posterior intrusion was started 4 weeks after the surgical procedure.
A nickel-titanium coil spring (GAC, Bohemia, NY) was attached from the exposed hook of the miniplate to the first molar to deliver an intrusive force of 450 g per side ( Fig 1 , B-E ). The intrusion force was stopped when the anterior overbite reached 1 to 2 mm.
Before starting the maxillary posterior intrusion, the mandibular arch was stabilized by a continuous 0.019 × 0.025-in stainless steel archwire bypassing the mandibular incisors to prevent the compensatory eruption of the mandibular molars during intrusion of the maxillary posterior teeth.
Throughout the treatment, the patients were instructed to perform tongue exercises using orthodontic intermaxillary rubber bands; the bands were placed on the tip of the tongue to bring it to the level of the incisive papilla. These exercises were repeated at least 4 or 5 times per day, aiming to reeducate the tongue posture in these open-bite patients.
After the completion of intrusion, the maxillary molars were ligature-tied to the miniplates, which remained until the end of active treatment. The subjects were evaluated for the need for extractions to correct mandibular anterior crowding, overjet, or reduced interincisal angle. Extraction of 4 first premolars was deemed necessary in all subjects. The patients were referred for the extractions. The mandibular incisors were bonded. Both arches were releveled to 0.019 × 0.025-in stainless steel wires, and the remaining spaces were closed.
The retention protocol included maxillary and mandibular Hawley retainers to be worn full time during the day except at mealtimes and toothbrushing during the first year after treatment. A maxillary Hawley retainer with a posterior bite plane was to be worn during the night to prevent overeruption of the posterior dentition. For the second year of retention, the patients were instructed to wear the maxillary Hawley retainer with the posterior bite plane with the traditional mandibular Hawley retainer only at night. During the third and fourth years, the same appliances were used 1 night a week. Additionally, the tongue exercises were reinforced during the retention period.
Lateral cephalograms of the subjects were taken before treatment (T1), immediately after treatment (T2), 1 year posttreatment (T3), and 4 years posttreatment (T4).
The lateral cephalometric radiographs were traced through the midpoints between the right and left structures, and any magnification was corrected in the measurements. Several angular and linear measurements were obtained from lateral cephalograms to analyze the skeletal, dental, and soft tissue changes ( Table I ; Fig 2 ).
| Measurement | Definition |
|---|---|
| Skeletal measurements | |
| SNA (°) | Anteroposterior position of maxillary base to the anterior cranial base |
| SNB (°) | Anteroposterior position of mandibular base to the anterior cranial base |
| ANB (°) | Anteroposterior relationship of maxillary base to mandibular base |
| ANS-Me (mm) | Lower anterior facial height, the measurement between anterior nasal spine (ANS) and menton (Me) |
| N-Me (mm) | Total anterior facial height, the measurement between nasion (N) and Me |
| SN-MP (°) | Mandibular plane angle, the angle between mandibular plane, gonion (Go)-Me and anterior cranial base plane (SN) |
| SN-Pog (°) | Angle between SN and N-pogonion (Pog) |
| VP-Pog (mm) | Distance between the vertical reference plane and Pog |
| N-S-Gn (°) | Angle between SN and gnathion (Gn) |
| Dental measurements | |
| U6-PP (mm) | Maxillary posterior dentoalveolar height, the perpendicular distance between the mesial cusp of the maxillary first molar and the palatal plane |
| U1-FHP (°) | Angle between the long axis of the most anterior maxillary central incisor and the constructed Frankfort horizontal plane |
| L1-FHP (°) | Angle between the long axis of the most anterior mandibular central incisor and the constructed Frankfort horizontal plane |
| L1-MP (°) | Angle between the long axis of the most anterior mandibular central incisor and the mandibular plane |
| L1-MP (mm) | Perpendicular distance between the most anterior mandibular central incisor tip and the mandibular plane |
| U1-FHP (mm) | Perpendicular distance between the most anterior maxillary central incisor tip and the constructed Frankfort horizontal plane |
| L6-MP (mm) | Mandibular molar height, the perpendicular distance between the mesial cusp of the mandibular first molar and the mandibular plane |
| Overjet (mm) | Horizontal distance between the incisal edges of the maxillary and mandibular central incisors, perpendicular to the constructed Frankfort horizontal plane |
| Overbite (mm) | Vertical distance between the incisal edges of the maxillary and mandibular central incisors, perpendicular to the vertical reference plane (VP) |
| Soft tissue measurement | |
| Soft tissue facial convexity (N′-Sn-Pog′) (°) | The smaller angle formed by the intersection of the N′-Sn line and the extension of the Pog’-Sn line at Sn |
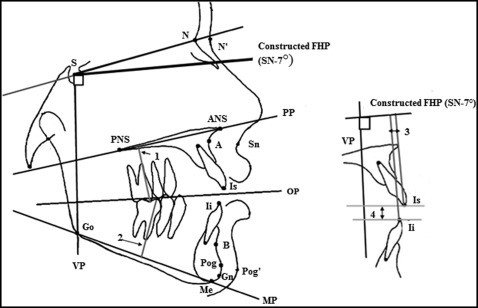
A constructed Frankfort horizontal plane was drawn with an inferior angle of 7° to the sella-nasion plane from point S; a vertical line, drawn from point S at 90° to the constructed Frankfort horizontal plane, functioned as the vertical plane of reference.
Statistical analysis
To preserve reliability, all cephalometric measurements and analyses were performed by the same investigator (E.S.M.). To exclude the intraexaminer error in the measurements, 10 randomly selected radiographs were retraced 2 weeks after the first measurements by the same examiner. A paired t test and the intraclass correlation coefficient were performed for the first and second measurements. The difference between the 2 sets of measurements was insignificant; the paired t test and the intraclass correlation coefficient were greater than 0.9.
The statistical analysis was accomplished using the SPSS software (version 17; SPSS, Chicago, Ill). Normal distribution of the sample data was confirmed with the Kolmogorov-Smirnov test. Results of this test demonstrated that all variables were normally distributed. A paired t test was used to compare the variables at T1 and T2. Comparisons among T2, T3, and T4 were done by repeated-measures analysis of variance followed by a paired t test. The Pearson correlation coefficient was used to study the correlations between the variables. Comparisons of the treatment changes between Angle Class I and Class II patients were performed using independent-samples t tests. The significance level was set at P ≤0.05.
Results
Table II shows the demographic data of the study sample. Two of the original 28 patients were lost to follow-up at T3; hence, 26 subjects were analyzed. Minimal mobility of the zygomatic miniplates was reported in 3 patients, but it did not warrant removal.
| Demographics | Treatment duration | ||
|---|---|---|---|
| Range | Mean | SD | |
| Pretreatment age | 19 y 4 mo-26 y 11 mo | 22 y 5 mo | 2y 4 mo |
| Duration of intrusion | 5-10 mo | 7.5 mo | 2.3 mo |
| Total treatment duration (T1-T2) | 24-28 mo | 26.2 mo | 1.98 mo |
| Duration between debonding and 1 year posttreatment (T2-T3) | 12-14 mo | 12.9 mo | 0.89 mo |
| Duration between end of 1 year posttreatment to end of 4 years posttreatment (T3-T4) | 36-41 mo | 38.6 mo | 2.11 mo |
∗ Study sample: 26 patients (15 women, 11 men). Angle classification: 16 Class I, 10 Class II.
The mean measurements and standard deviations for the selected cephalometric variables at T1, T2, T3, and T4 are shown in Table III . The mean differences of the measurements between the various time intervals are given in Table IV .
| T1 | T2 | T3 | T4 | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Skeletal measurements | ||||||||
| SNA (°) | 81.86 | 2.59 | 80.20 | 2.62 | 80.31 | 2.60 | 80.42 | 2.69 |
| SNB (°) | 75.00 | 3.21 | 77.18 | 3.23 | 76.96 | 3.29 | 76.79 | 3.34 |
| ANB (°) | 6.86 | 1.13 | 3.02 | 1.11 | 3.35 | 1.14 | 3.63 | 1.15 |
| ANS-Me (mm) | 78.05 | 5.83 | 74.48 | 5.50 | 75.05 | 5.49 | 75.55 | 5.49 |
| N-Me (mm) | 124.68 | 6.14 | 121.05 | 5.69 | 121.61 | 5.76 | 122.11 | 5.76 |
| SN-MP (°) | 49.05 | 3.90 | 46.91 | 3.89 | 47.19 | 3.91 | 47.43 | 3.93 |
| SN-Pog (°) | 74.68 | 2.82 | 77.00 | 2.51 | 76.51 | 2.70 | 76.17 | 2.75 |
| VP-Pog (mm) | 45.00 | 6.09 | 47.45 | 6.06 | 46.67 | 6.09 | 46.05 | 6.09 |
| N-S-Gn (°) | 77.09 | 3.01 | 74.86 | 2.67 | 75.39 | 2.83 | 75.69 | 2.89 |
| Dental measurements | ||||||||
| U6-PP (mm) | 28.27 | 2.55 | 25.23 | 2.14 | 25.54 | 2.17 | 25.64 | 2.17 |
| U1-FH (°) | 114.82 | 3.91 | 111.73 | 1.28 | 112.13 | 1.41 | 112.25 | 1.51 |
| L1-FH (°) | 42.82 | 3.87 | 44.30 | 3.59 | 43.96 | 3.59 | 43.87 | 3.58 |
| L1-MP (°) | 91.32 | 1.17 | 90.03 | 1.06 | 90.42 | 0.99 | 90.50 | 0.99 |
| L1-MP (mm) | 44.05 | 2.79 | 45.62 | 2.82 | 45.32 | 2.80 | 45.56 | 2.82 |
| U1-FH (mm) | 74.45 | 3.89 | 76.95 | 3.99 | 76.77 | 4.02 | 77.38 | 3.85 |
| L6-MP (mm) | 34.43 | 1.27 | 34.86 | 1.35 | 34.57 | 1.13 | 34.29 | 1.38 |
| Overbite (mm) | −4.75 | 2.27 | 2.18 | 0.48 | 1.61 | 0.42 | 1.41 | 0.39 |
| Overjet (mm) | 5.55 | 2.28 | 2.16 | 0.45 | 2.61 | 0.46 | 2.72 | 0.46 |
| Soft tissue measurement | ||||||||
| Soft tissue facial convexity N′-Sn-Pog′ (°) | 25.91 | 3.24 | 23.55 | 2.43 | 23.90 | 2.42 | 24.09 | 2.44 |
| T2-T1 | T3-T2 | T4-T3 | T4-T2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | P | Mean | SD | P | Mean | SD | P | Mean | SD | P | |
| Skeletal measurements | ||||||||||||
| SNA (°) | −1.66 | 0.45 | * | 0.11 | 0.18 | NS | 0.11 | 1.97 | NS | 0.22 | 2.01 | NS |
| SNB (°) | 2.18 | 0.40 | † | −0.22 | 0.09 | NS | −0.17 | 2.36 | NS | −0.39 | 2.35 | NS |
| ANB (°) | −3.84 | 0.70 | † | 0.33 | 0.16 | NS | 0.28 | 0.10 | NS | 0.61 | 0.10 | * |
| ANS-Me (mm) | −3.57 | 1.15 | † | 0.57 | 0.18 | NS | 0.50 | 5.15 | NS | 1.07 | 5.21 | NS |
| N-Me (mm) | −3.64 | 1.06 | † | 0.57 | 0.18 | NS | 0.50 | 4.64 | NS | 1.07 | 4.67 | NS |
| SN-MP (°) | −2.13 | 0.21 | † | 0.27 | 0.05 | NS | 0.24 | 3.55 | NS | 0.51 | 3.55 | NS |
| SN-Pog (°) | 2.32 | 0.48 | † | −0.49 | 0.22 | NS | −0.34 | 2.03 | NS | −0.83 | 1.96 | * |
| VP-Pog (mm) | 2.45 | 0.05 | † | −0.77 | 0.05 | NS | −0.63 | 5.44 | NS | −1.40 | 5.42 | * |
| N-S-Gn (°) | −2.23 | 0.37 | † | 0.53 | 0.20 | NS | 0.30 | 2.57 | NS | 0.83 | 2.52 | NS |
| Dental measurements | ||||||||||||
| U6-PP (mm) | −3.04 | 0.79 | † | 0.31 | 0.07 | NS | 0.10 | 2.04 | NS | 0.41 | 2.03 | NS |
| U1-FH (°) | −3.09 | 3.19 | † | 0.41 | 0.42 | NS | 0.11 | 1.42 | NS | 0.52 | 1.46 | NS |
| L1-FH (°) | 1.48 | 0.59 | * | −0.33 | 0.09 | NS | −0.09 | 3.30 | NS | −0.42 | 3.28 | NS |
| L1-MP (°) | −1.29 | 0.50 | * | 0.40 | 0.10 | NS | 0.08 | 0.99 | NS | 0.48 | 1.02 | NS |
| L1-MP (mm) | 1.57 | 0.07 | NS | −0.30 | 0.05 | NS | 0.24 | 1.88 | NS | −0.06 | 1.89 | NS |
| U1-FH (mm) | 2.5 | 0.11 | † | −0.18 | 0.035 | NS | 0.61 | 2.725 | NS | 0.43 | 2.708 | NS |
| L6-MP (mm) | 0.43 | 0.53 | NS | −0.29 | 0.49 | NS | −0.29 | 0.49 | NS | −0.57 | 0.53 | NS |
| Overbite (mm) | 6.93 | 1.99 | † | −0.57 | 0.09 | NS | −0.20 | 0.38 | NS | −0.77 | 0.43 | NS |
| Overjet (mm) | −3.39 | 2.04 | † | 0.46 | 0.05 | NS | 0.11 | 0.48 | NS | 0.56 | 0.48 | NS |
| Soft tissue measurement | ||||||||||||
| Soft tissue facial convexity N′-Sn-Pog′ (°) | −2.36 | 0.92 | † | 0.36 | 0.11 | NS | 0.18 | 2.09 | NS | 0.54 | 2.09 | NS |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


