Introduction
In this randomized clinical trial, we investigated, using the microbial culture technique and scanning electron microscopy, the contamination of acrylic baseplates of removable orthodontic appliances by mutans streptococci (MS) and evaluated the efficacy of different home disinfection protocols with a 0.12% chlorhexidine gluconate spray (Periogard, Colgate-Palmolive, São Bernardo do Campo, Brazil).
Methods
Fifteen dental students were randomly enrolled in a 3-stage changeover system with a 1-week interval between each stage. The acrylic baseplates were worn full time except at meals to simulate the routine use of removable appliances under clinical conditions. Three 1-week home disinfection protocols were tested in all stages by a different group of students: protocol I, toothbrushing + baseplate brushing + sterile tap water spraying once a day; protocol II, toothbrushing + baseplate brushing + Periogard spraying on the seventh day after appliance placement; and protocol III, toothbrushing + baseplate brushing + Periogard spraying on the fourth and seventh days after appliance placement. After the first week, the volunteers received new baseplates, toothbrushes, and dentifrices, and the regimens were repeated 2 more times. At the end of each week, the baseplates had a randomized disinfection protocol and were sent for microbiologic analysis. A scanning electron microscope was used to examine 3 acrylic baseplates representing each home protocol. The Friedman test (α = 0.05) compared the home protocols for the formation of MS colonies or biofilms on the acrylic surfaces.
Results
MS colonies or biofilms were found on all acrylic baseplates after protocol I. Protocols II and III reduced significantly ( P <0.05) the number of MS colonies and biofilms on the acrylic surfaces. No significant difference ( P >0.05) was observed between protocols II and III. The scanning electron microscope analysis confirmed the results of the microbiologic cultures.
Conclusions
Disinfection of baseplates of removable orthodontic appliances by using 0.12% chlorhexidine spray once or twice a week reduced the contamination by MS on the acrylic surface in vivo.
Orthodontic appliances become colonized by microorganisms after a certain time in the mouth. The use of removable appliances, like that of fixed appliances, results in the accumulation of bacterial biofilm on dental surfaces and metallic and ceramic brackets, orthodontic wires, bands, orthodontic adhesives, springs, elastics, and acrylic baseplates. Orthodontic accessories are difficult to clean during routine oral hygiene and provide retentive sites for microorganisms. These microorganisms are organized as biofilms and can adhere to the components of removable orthodontic appliances, especially the acrylic baseplate, which has porosities on its outer and inner surfaces that create favorable conditions for bacterial colonization. Mature biofilms are composed of several bacterial species, including cariogenic microorganisms, such as mutans streptococci (MS).
Adequate brushing with a fluoride dentifrice is an effective means of controlling the biofilm that forms on the surface of removable orthodontic appliances. However, lack of manual dexterity and inappropriate oral home-care quality and frequency are factors that compromise the efficacy of the mechanical control of biofilm in orthodontic patients.
Removable orthodontic appliances are not disinfected systematically in dental practices. Although there is no specific clinical protocol for the control of bacterial biofilm on orthodontic appliances, the use of antimicrobial agents has been advised for patients to aid in the control of bacterial biofilm formation because toothbrushes cannot completely remove microorganisms from critical retentive sites of the appliances. Chlorhexidine has been considered the gold standard for the chemical control of biofilm compared with other antimicrobials. Although a recent study found that spraying with a 0.12% chlorhexidine gluconate solution (Periogard, Colgate-Palmolive, São Bernardo do Campo, Brazil) was effective in reducing MS colonies and biofilms on the surface of orthodontic acrylic baseplates, no studies have evaluated the efficacy of systematic home protocols based on the use of chlorhexidine for disinfection of removable orthodontic appliances.
In this randomized clinical trial, we investigated, using the microbial culture technique and scanning electron microscopy (SEM), the contamination of acrylic baseplates of removable orthodontic appliances by MS and evaluated the efficacy of different home disinfection protocols with a 0.12% chlorhexidine gluconate spray (Periogard).
Material and methods
One hundred fifty third- and fourth-year undergraduate dental students of both sexes, aged 18 to 25 years, from the Dental School of Ribeirão Preto of the University of São Paulo in Brazil were invited to participate in the study. All students had a clinical interview, a review of dental and medical history, and a clinical examination, and those with good general health and occlusion with favorable dental alignment were considered as eligible participants. Those with severe tooth crowding, accentuated diastemas, and periodontal problems, and those who were using antimicrobial mouthwashes, had any systemic disease, or had used antibiotics within the previous 3 months were excluded from the trial. One hundred students met the criteria for the study. The salivary MS counts of the subjects were determined. Aliquots of 0.05 mL of diluted pure nonstimulated saliva samples were seeded on SB 20 solid culture medium (tryptone soy yeast agar plus 20% sucrose and 0.2 U per milliliter of bacitracin; Sigma-Aldrich, St Louis, Mo), which is a selective medium for MS and was prepared according to Saravia et al and Nelson-Filho et al. The numbers of colony forming units per milliliter of saliva were counted under aseptic conditions with a stereomicroscope (Nikon, Tokyo, Japan) with reflected light. Colonies and biofilms with MS characteristics were transferred to tubes containing thioglycollate (Difco Laboratories, Detroit, Mich) and incubated at 37°C for 24 hours for biochemical identification.
After this initial screening, 21 subjects with salivary MS counts were enrolled as participants. These subjects received verbal and written explanations about the study purposes and procedures, and all signed an informed consent form before final enrollment. The research project was reviewed and approved by the Research Ethics Committee of the Dental School of Ribeirão Preto, University of São Paulo (process 2006.1.477.58.0). By using a table of random numbers, the students were assigned to a 3-stage changeover system with a 1-week interval between each stage. Three home disinfection protocols were established, and each was used by a different group of students in each stage to minimize any variables that could interfere with the results. All 21 volunteers performed all disinfection protocols.
Individual baseplates of orthodontic appliances without wire clasps were constructed on cast models obtained from each patient. No retentive wire components, such as clasps, were used because the study purpose was to investigate the formation of MS colonies and biofilms on acrylic surfaces only. The baseplates were fabricated with autopolymerizing acrylic resin (Ortoclass; Clássico Artigos Odontológicos, São Paulo, São Paulo, Brazil) following the monomer-to-polymer mixing ratio advised by the manufacturer and standard acrylization, trimming, finishing, and polishing techniques.
The patients were requested to wear the acrylic baseplates full time during 7 consecutive days (even for sleep), removing them only during meals, to simulate the routine use of removable appliances under clinical conditions. The students were instructed to brush the teeth and the acrylic baseplates 3 times a day after meals using a toothbrush (Colgate Professional, Colgate-Palmolive) and a dentifrice (Colgate Máxima Proteção Anticáries, Colgate-Palmolive) supplied by the researchers. The antimicrobial agent used in this study was a 0.12% chlorhexidine gluconate solution (Periogard). Sterile tap water was used as a control. The solutions were placed in individual plastic trigger spray bottles (Elyplast, São José dos Campos, São Paulo, Brazil) under aseptic conditions. At bedtime, after brushing, the volunteers were instructed to hold the baseplates in a fixed position and spray the test solution (1 solution for each 1-week stage) on all acrylic surfaces at a distance of 5 cm, repeating 3 times on each side (totaling approximately 2.5 mL of solution). Tap water was sprayed every day during the 7-day trial (protocol I), whereas Periogard was sprayed either once (at day 7) (protocol II) or twice (at days 4 and 7) (protocol III). The sprayed acrylic baseplates were individually stored in sterile closed receptacles and sent to the laboratory for microbiologic processing immediately after removal from the subjects, within a maximum of 30 minutes. After the first week of the trial, the volunteers received new baseplates, toothbrushes, and dentifrices, and the regimens were repeated 2 more times.
The acrylic baseplates were placed into 80-mL sterile universal containers (Pleion Industria e Comércio de Plásticos, Barueri, São Paulo, Brazil) containing bacitracin sucrose broth, which is a selective enrichment broth specific for MS prepared without trypan blue according to the modification proposed by Jensen and Brattall for 3 to 4 days at 37°C. Both sides of the baseplates were analyzed, and the sessile MS colonies or biofilms adhering to the acrylic surface were counted under aseptic conditions with a stereomicroscope with reflected light.
The numbers of MS colonies or biofilms on the acrylic surface after microbial culture were counted and expressed according to a 4-point scoring system, as suggested by Nelson-Filho et al : 0, no MS colonies or biofilms; 1, 1 to 50 MS colonies or biofilms; 2, 51 to 100 MS colonies or biofilms; 3, over 100 MS colonies or biofilms (intense bacterial growth, with confluent colonies, not allowing an accurate counting). Four to 5 colonies or biofilms representing bacterial growth were collected, transferred to tubes containing glass beads and 2 mL of phosphate buffer saline solution, and vortexed for 2 minutes. The resulting suspension was seeded on modified SB 20 agar and incubated in microaerophilia at 37°C for 72 hours. The biochemical tests used for selection of the study subjects were repeated to confirm that the microorganisms on the acrylic surface were MS.
The counts of MS colonies or biofilms were analyzed by using the SAS statistical software package (SAS, Cary, NC). The Friedman nonparametric test for paired samples was used to analyze the differences at the 5% significance level among the 3 home disinfection protocols for the formation of colonies and biofilms on the acrylic surfaces.
After counting the MS colonies or biofilms, 3 acrylic baseplates representing the results obtained with each test solution (Periogard and sterile tap water) were selected and prepared for SEM analysis. One fragment of each acrylic baseplate was sectioned with a pair of pliers and placed in 3% glutaraldehyde for 48 hours. The fragments were then rinsed in distilled water, dehydrated in a series of increasing ethanol concentrations, critical-point dried with liquid carbon dioxide, mounted on stubs, sputter-coated with gold under vacuum (Delton Vacuum Desk II, Mooretown, NJ) for 60 seconds, and examined with the SEM operating at 15 kV (EVO 50 microscope; Carl Zeiss, Jena, Germany). SEM micrographs were taken at magnifications from 800 to 3500 times to determine the presence or absence of MS colonies and biofilms. The examiners (I.T.A.P. and I.Y.I) were blinded to the groups during the microbiologic and SEM analyses.
Results
Of the 21 volunteers enrolled in the study, 15 (71.42%) completed their participation in all stages of randomization. Six (28.58%) volunteers were excluded for the following reasons: 3 used antibiotics after entering the study, 2 missed 1 stage of the trial, and 1 lost a baseplate.
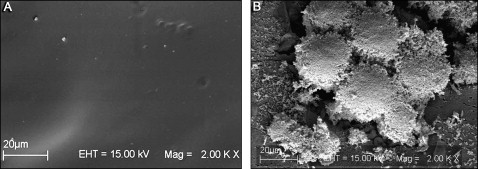
The microbiologic results relative to MS colonies and biofilms adhering to the surface of the acrylic baseplates after the 3 home disinfection protocols are presented in the Table. MS colonies and biofilms were observed in all 15 (100%) acrylic baseplates sprayed with sterile tap water (protocol I, control); 11 of them had intense microbial contamination with uncountable numbers of MS colonies andbiofilms ( Fig 1 ).
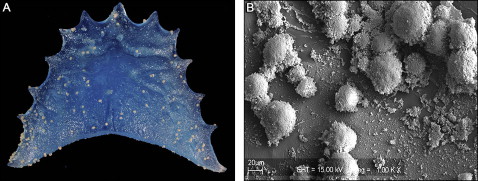
For protocols II (Periogard once a week) ( Fig 2 , A ) and III (Periogard twice a week) ( Fig 2 , B ), there were MS contaminations of 80% and 60%, respectively, with the numbers of colonies or biofilms ranging from 0 to uncountable for both home disinfection protocols. Uncountable numbers of MS colonies or biofilms were found on 7 baseplates disinfected with protocol II and 4 baseplates disinfected with protocol III, whereas 3 baseplates disinfected with protocol II and 6 baseplates disinfected with protocol III showed no MS colonies or biofilms.
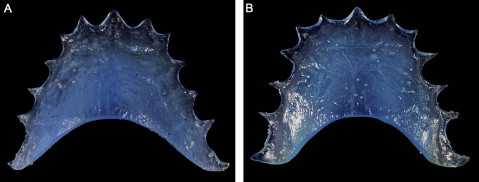
Compared with the baseplates treated with protocol I (control), there were significantly fewer MS colonies and biofilms on the surfaces of 7 baseplates (46.6%) treated with protocol II and 11 baseplates (73.3%) treated with protocol III.
When the microbiologic culture was positive—ie, when MS colonies or biofilms were seen under stereomicroscopy—MS colonies or biofilms were observed on the acrylic surfaces by SEM ( Figs 1 , B , and 3 , B ). When no colonies or biofilms were seen under stereomicroscopy, the SEM analysis showed no microorganisms in the specimens of protocols II and III ( Fig 3 , A ), or a few sparse microorganisms in the specimens of protocol II.