Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Describe signs of successful and unsuccessful root canal treatment.
- 2.
Describe the most common modalities used to determine success or failure.
- 3.
State the approximate range of expected outcomes of routine, uncomplicated root canal treatment based on pretreatment conditions.
- 4.
State predictors of success and failure.
- 5.
Identify endodontic and nonendodontic causes of treatment failure.
- 6.
State the outcomes of retreatment, endodontic surgery, and intentional replantation.
- 7.
State the outcomes of fixed partial denture and single tooth implant treatments.
- 8.
Approach treatment planning of root canal failure, recognizing the advantages and disadvantages of different treatment modalities.
The highest possible long-term levels of comfort, function, and esthetics are the primary objectives of root canal treatment in patients with inflammation or infection arising from disease of pulpal origin or trauma. These objectives are achieved by eliminating or significantly reducing bacteria and preventing recontamination. Rubber dam isolation and aseptic technique provide a hygienic environment. Thorough chemomechanical cleaning and shaping eliminate or significantly reduce pathogenic bacteria. Complete obturation eliminates a habitat for bacteria. Leak-resistant restoration prevents bacterial recontamination and achieves functional and esthetic rehabilitation.
Optimal outcomes are dependent on attainment of these technical goals. Because of the complexity of root canal systems, less than perfect instrumentation and obturation methods, and leakage of permanent restorations, elimination of bacteria from the root canal systems cannot be achieved in some cases. Adherence to proper protocol significantly improves the prognosis of root canal–treated teeth; however, because of the complex interactions between host and pathogen, unexpected results are occasionally seen, regardless of whether proper or improper protocols were followed.
The purposes of this chapter are to (1) define success and failure, (2) describe methods for evaluation of endodontic outcomes, (3) provide success rates, (4) explain the signs and symptoms of negative outcomes, (5) discuss factors influencing outcomes, and (6) compare the outcomes of initial nonsurgical root canal treatment with those of retreatment, endodontic surgery, and alternative treatments, such as single tooth implants.
Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Describe signs of successful and unsuccessful root canal treatment.
- 2.
Describe the most common modalities used to determine success or failure.
- 3.
State the approximate range of expected outcomes of routine, uncomplicated root canal treatment based on pretreatment conditions.
- 4.
State predictors of success and failure.
- 5.
Identify endodontic and nonendodontic causes of treatment failure.
- 6.
State the outcomes of retreatment, endodontic surgery, and intentional replantation.
- 7.
State the outcomes of fixed partial denture and single tooth implant treatments.
- 8.
Approach treatment planning of root canal failure, recognizing the advantages and disadvantages of different treatment modalities.
The highest possible long-term levels of comfort, function, and esthetics are the primary objectives of root canal treatment in patients with inflammation or infection arising from disease of pulpal origin or trauma. These objectives are achieved by eliminating or significantly reducing bacteria and preventing recontamination. Rubber dam isolation and aseptic technique provide a hygienic environment. Thorough chemomechanical cleaning and shaping eliminate or significantly reduce pathogenic bacteria. Complete obturation eliminates a habitat for bacteria. Leak-resistant restoration prevents bacterial recontamination and achieves functional and esthetic rehabilitation.
Optimal outcomes are dependent on attainment of these technical goals. Because of the complexity of root canal systems, less than perfect instrumentation and obturation methods, and leakage of permanent restorations, elimination of bacteria from the root canal systems cannot be achieved in some cases. Adherence to proper protocol significantly improves the prognosis of root canal–treated teeth; however, because of the complex interactions between host and pathogen, unexpected results are occasionally seen, regardless of whether proper or improper protocols were followed.
The purposes of this chapter are to (1) define success and failure, (2) describe methods for evaluation of endodontic outcomes, (3) provide success rates, (4) explain the signs and symptoms of negative outcomes, (5) discuss factors influencing outcomes, and (6) compare the outcomes of initial nonsurgical root canal treatment with those of retreatment, endodontic surgery, and alternative treatments, such as single tooth implants.
Definitions of Success and Failure
Patients, third-party payers, and dentists, all stakeholders in the dental delivery system, have differing perspectives on and expectations for the outcomes of root canal treatment. Patients are usually satisfied if their teeth are comfortable, functional, and esthetically pleasing. Insurance companies measure success by access to care, quality of care, cost, and the longevity of the treatment provided. Dentists are usually most concerned with the delivery of optimal care, predictable elimination of disease as measured clinically and radiographically, and fair compensation. The real art of dentistry is to coordinate and interface these perspectives and expectations among the stakeholders without sacrificing the quality of care.
Over the years, many terms have been used to describe endodontic outcomes. Sometimes the same words have been defined in different ways by different authors. Therefore, it is important to understand the definitions of the words being used. The simple terms “success” and “failure” may be clear to all. The absence of clinical symptoms and apical lesions is the principal indicator of successful root canal treatment. It is important to remember that apical periodontitis is frequently asymptomatic and can often only be demonstrated radiographically.
For a treated tooth with a previously vital pulp and no preexisting apical lesion, success means that the tooth remains asymptomatic and an apical lesion does not form. New symptoms or the appearance of an apical lesion is a sign of a failed root canal in a tooth with a previously vital pulp and no preexisting apical lesion.
For a tooth with a previously necrotic pulp, the treatment is considered successful if the tooth remains asymptomatic, its preexisting apical lesion heals, and no new apical lesion develops. The presence of symptoms or a new or enlarging lesion in a tooth with necrotic pulp indicates failure.
As an alternative to the terms “success” and “failure,” the American Association of Endodontists has proposed the following terms:
- ▪
Healed —Functional, asymptomatic teeth with no or minimal radiographic periradicular pathosis
- ▪
Nonhealed —Nonfunctional, symptomatic teeth with or without radiographic periradicular pathosis
- ▪
Healing —Teeth with periradicular pathosis that are asymptomatic and functional, or teeth with or without radiographic periradicular pathosis that are symptomatic but for which the intended function is not altered
- ▪
Functional —A treated tooth or root that is serving its intended purpose in the dentition
Because the path to bony periradicular healing may be long and irregular, determination of success or failure may be difficult. Many asymptomatic root canal–treated teeth have varying degrees of radiolucency. The dentist must judge whether these teeth are in progress to success or to failure and then advise the patient and manage the teeth appropriately.
When to Evaluate
Recommended follow-up periods have ranged from 6 months to 5 years. Six months is a widely accepted and reasonable interval for a recall evaluation for most patients. The key question is: At what point is it likely that a treatment outcome will not change? In other words: When can it be determined that treatment has either succeeded or failed, and the outcome is unlikely to change, so that no further recall is necessary? A radiographic lesion that is unchanged or has increased in size after 1 year is unlikely to ever resolve; therefore, the treatment may be considered to be unsuccessful. If at 6 months the lesion is still present but smaller, it is likely to be in progress to healing, and additional recall is needed. It takes longer for larger periradicular lesions to heal than smaller lesions. Unfortunately, apparent success may revert to failure at a later time (often as a result of reinfection through coronal leakage). Late healing may also occur. Therefore, an endodontic evaluation, including a patient history, clinical examination, and radiography of teeth treated with root canals, should be part of every comprehensive patient examination.
Methods for Evaluation of Endodontic Outcomes
The patient history, clinical findings, and radiographic examinations are the commonest metrics of root canal treatment outcomes. Evaluation of endodontic outcomes follows the same diagnostic pathway as for initial treatment (see Chapter 5 ). Biopsy of periradicular tissues during endodontic surgery provides a histologic diagnosis, another method for evaluation of success or failure of root canal treatment. This method is not routinely used and is an impractical approach to determine clinical outcomes of root canal treatments.
Patient History
Complaints of persistent or worsening symptoms months or years after root canal treatment has been completed are usually an indication of treatment failure and continuing disease. Symptoms related to discomfort or pain on chewing, aching, and so forth are generally an indication of periradicular inflammation or infection. It must be remembered that bony healing takes time and that a tooth that feels “different” on biting may be en route to healing; this should be confirmed clinically and radiographically. Pain on release may indicate a cracked tooth. A bad taste may indicate a draining abscess. Occasionally a patient reports sensitivity to cold or heat; this is most likely related to an adjacent untreated tooth but could be an indication of a missed vital canal in a treated tooth.
Clinical Examination
Presence of persistent signs or symptoms is usually an indication of disease and failure. However, absence of symptoms does not signify success. Periapical pathosis without significant symptoms is usually present in teeth before and after root canal treatment until healing has occurred. There is little correlation between the presence of pathosis and corresponding symptoms; yet when adverse signs or symptoms are evident, there is a strong likelihood that a pathosis is present. Persistent signs (e.g., swelling, probing defect, or sinus tract) or symptoms usually indicate failure.
Clinical criteria for success generally include the following :
- ▪
Absence of swelling and other signs of infection and inflammation
- ▪
Disappearance of sinus tract or narrow, isolated probing defect
- ▪
No evidence of soft tissue destruction, including probing defects
- ▪
The tooth has been restored and is in function.
Radiographic Findings
Radiograph findings can classify the outcome of each treatment as success, failure, or unknown status. Radiographs made at different times must be made in a reproducible fashion and with minimal distortion so that valid longitudinal comparisons can be made over time. The best way to ensure reproducibility is to use a radiographic paralleling device (see Chapter 12 ). Teeth with multiple roots or canals should be examined using both straight-on and off-angle periapical views.
Radiographic success is the absence of an apical radiolucent lesion. This means that a lesion present at the time of treatment has resolved or, if there was no lesion present at the time of treatment, none has developed. Thus radiographic success is evident by the elimination or lack of development of an area of radiolucency for a minimum of 1 year after treatment ( Fig. 22.1 ).
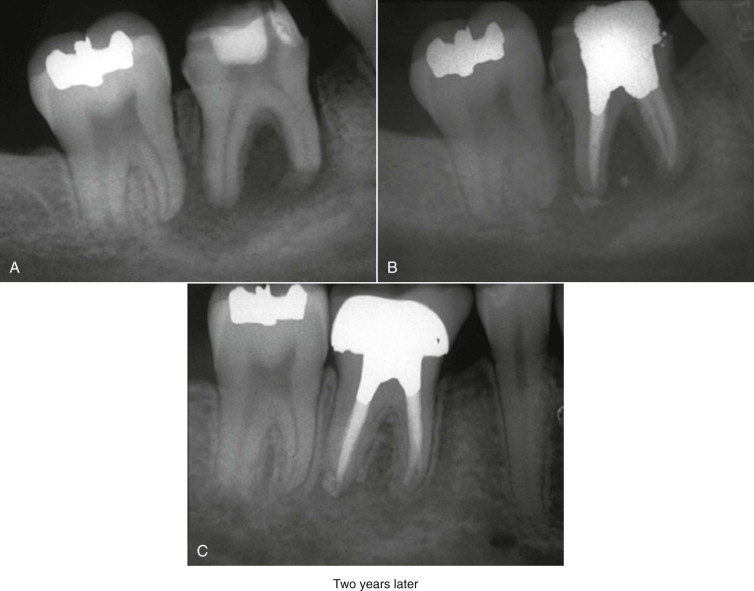
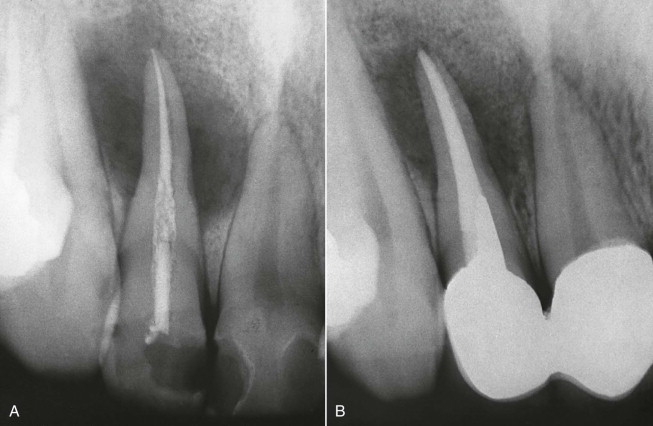
Radiographic failure is the continued persistence or development of radiolucency. Specifically, a radiolucent lesion has remained the same, enlarged, or has developed since treatment ( Fig. 22.2 ). Nonfunctional, symptomatic teeth with or without radiographic lesions are considered failures.
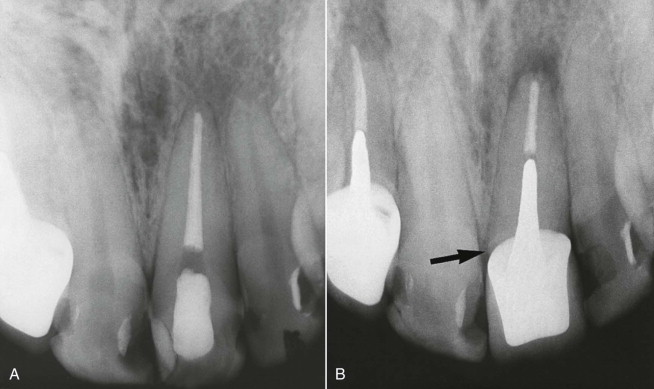
Radiographically unknown status indicates a state of uncertainty. This classification includes teeth with radiolucency that are asymptomatic and functional. The preexisting radiolucent lesion in these teeth has not yet decreased or become larger in size. Teeth with radiolucencies that were treated elsewhere and for which there are no prior radiographs for comparison are often assigned to this category ( Fig. 22.3 ).
A shortcoming of radiographic evaluation is that radiographs may not be made or interpreted in standardized ways. As early as 1966, Bender and coworkers noted that radiographic interpretation is often subject to personal bias and that a change in angulation can give a completely different appearance to the lesion, making it appear either smaller or larger. Also, different observers may not agree on what they see in a radiograph, and the same observer may disagree with his or her earlier interpretation if asked to review the same radiograph at a different time.
Long ago, in order to study predictors of endodontic treatment outcomes, Larz Strindberg created a three-step scale based on the history of symptoms, the clinical examination, and radiographic signs. These criteria were extremely strict, designed for predicting future outcomes, not current outcomes; even the appearance of a poorly defined lamina dura was reason for assignment as failure. Later, Ørstavik and associates suggested a five-step periapical index (PAI) for use in epidemiologic studies of root canal treatment. A current patient radiograph is compared to a set of five standard radiographic images ranging from a radiographically healthy periapex to a large periapical lesion. Preoperative and recall radiographs are assigned scores according to their resemblance to one of the five reference images. The PAI can classify root canal treatments as “healing” if the lesion size is reduced, “healed” if the lesion has been completely eliminated, or “developing” if a new lesion has formed. The PAI correlates with the histology and radiodensity; it is accurate, reproducible, and discriminatory. However, root canal treatments measured using the PAI typically do not reach complete healing for several years. As late as 4 to 5 years after surgery, according to the PAI, slow healers tend to outnumber late failures.
Cone beam computed tomography (CBCT) can be used for endodontic diagnosis and for assessment of healing. CBCT may sometimes reveal pathology not seen using periapical radiography. However, healing must be judged over time using a comparable baseline preoperative view; it cannot be assessed by a single snapshot nor by comparison of dissimilar images. Currently, CBCT has lower resolution, greater expense, and considerably higher radiation exposure than conventional periapical films and digital images.
Histologic Examination
Routine histologic evaluation of periapical tissues after root canal treatment is impractical and impossible without surgery. If a treated tooth were to be evaluated histologically, success would be signified by reconstitution of the periradicular tissue structure and absence of inflammation ( Fig. 22.4 ).
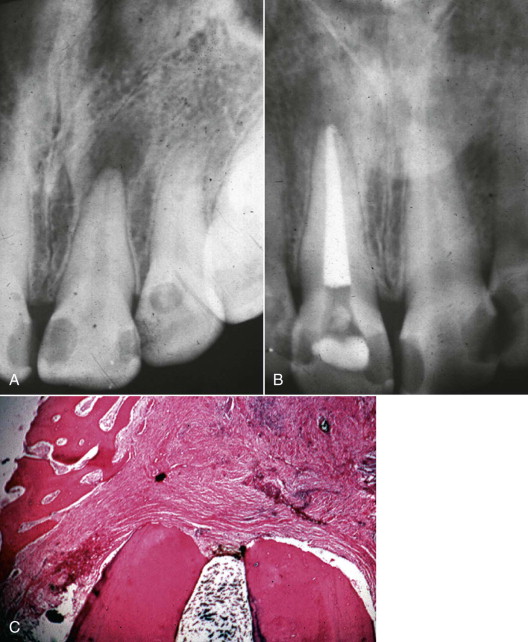
The degree of correlation between histologic findings and radiographic appearance is unclear. Two cadaver-based histologic investigations of teeth treated with root canals reached different conclusions. Brynolf concluded that most root canal–treated teeth showed some periradicular histological inflammation despite the appearance of radiographic success. In contrast, Green and colleagues observed that most root canal–treated teeth with radiographically normal periapices were indeed free of histologic inflammation. Thus, with current technology, the patient history, clinical evaluation, and radiography are the only practical means of assessing healing after root canal treatment.
Success Rates
As is the case for all dental and medical procedures, some root canal treatments may be unsuccessful. Prompt recognition and management of treatments that do not resolve and heal are critical but can be difficult and complex. Historically, it has been thought that success rates for root canal treatment, using highly discriminatory instruments such as the Strindberg criteria or the PAI, range from 80% to 95%. However, general percentages should be taken with caution, and each case should be individually assessed to determine its probability of success.
Torabinejad and colleagues performed a systematic review of the literature pertaining to success and failure of nonsurgical root canal therapy and assigned levels of evidence (LOE) to the studies. In the prior 40 years, 306 articles had been published related to the outcome of nonsurgical root canal treatment. Fifty-one studies included at least 100 teeth; meta-analysis of these studies suggested an overall radiographic success rate of 81.5% over a period of 5 years. Others who assessed the 4- to 6-year outcomes of initial endodontic treatment have reported similar overall healing rates. In a recent systematic review, Torabinejad and colleagues compared the outcomes of endodontically treated teeth with those of single implant crowns, fixed dental prostheses, and no treatment after extraction. Success data in that review consistently ranked implant therapy as superior to endodontic treatment, which in turn was ranked as superior to fixed prosthodontic treatment ( Table 22.1 ). However, very different criteria for success are used in implant dentistry, endodontics, and prosthodontics; therefore, such comparisons lack validity. Comparison of survival rates is much more meaningful.
| Procedure | Success (%) | Survival (%) |
|---|---|---|
| 2 to 4 Years | ||
| Dental implant (pooled) | 98 (95-99) | 95 (93-97) |
| Dental implant (weighted) | 99 (96-100) | 96 (94-97) |
| Root canal treatment (pooled) | 90 (88-92) | 94 |
| Root canal treatment (weighted) | 89 (88-91) | — |
| Three-unit bridge (pooled) | 79 (69-87) | 94 |
| Three-unit bridge (weighted) | 78 (76-81) | — |
| 4 to 6 Years | ||
| Dental implant (pooled) | 97 (96-98) | 97 (95-98) |
| Dental implant (weighted) | 98 (97-99) | 97 (95-98) |
| Root canal treatment (pooled) | 93 (87-97) | 94 (92-96) |
| Root canal treatment (weighted) | 94 (92-96) | 94 (91-96) |
| Three-unit bridge (pooled) | 82 (71-91) | 93 |
| Three-unit bridge (weighted) | 76 (74-79) | — |
| 6+ Years | ||
| Dental implant (pooled) | 95 (93-96) | 97 (95-99) |
| Dental implant (weighted) | 95 (93-97) | 97 (96-98) |
| Root canal treatment (pooled) | 84 (82-87) | 92 (84-97) |
| Root canal treatment (weighted) | 84 (81-87) | 97 (97-97) |
| Three-unit bridge (pooled) | 81 (74-86) | 82 |
| Three-unit bridge (weighted) | 80 (79-82) | — |
Survival Rates
Long-term survival rates for endodontically treated teeth are very high, over 90%. A recent systematic review by Torabinejad and colleagues showed that both root canal and implant treatments resulted in a very high survival rate (97% at more than 6 years), compared to only 80% for a fixed dental prosthesis, a three- or four-unit bridge (see Table 22.1 ). Iqbal and Kim reported similar findings in a systematic review when they compared the survival rates of restored endodontically treated teeth with those of implant-supported restorations. Several very large studies have all reported extremely high long-term survival rates for teeth with root canal treatment: Lazarski and colleages, 94% functional survival for 44,613 cases at 3.5 years in the United States; Salehrabi and Rotstein, 97% survival for 1.1 million patients at 8 years in the United States; and Chen and colleagues, 93% survival for 1.5 million teeth at 5 years in Taiwan. Teeth with root canal treatments have remarkably high long-term survival rates.
Patient-Based Outcomes
Patients choose root canal treatment (RCT) to retain teeth (and thus preserve the natural esthetics of their smile) and to relieve pain. Anticipation and experience of root canal–associated pain are major sources of fear for patients and a very important concern of dentists. Pain is anticipated, experienced, remembered, and shared by patients. A recent systematic review found that the severity of pretreatment root canal–associated pain was moderate, dropped substantially within 1 day of treatment, and continued to drop to minimal levels in 7 days. The prevalence of pretreatment root canal–associated pain was high but dropped moderately within 1 day and substantially to minimal levels in 7 days. Supplemental anesthesia is often required during treatment. Pain during RCT was usually less than anticipated. High percentages of patients reported a willingness to choose root canal treatment again. Overall satisfaction ratings for root canal treatment are extremely high, generally above the 90th percentile. Satisfaction is higher when endodontic treatment is provided by specialists, probably a reflection of effective communication and efficient management. Initial costs for root canal treatment and restoration are substantially lower than for replacement with an implant single crown or fixed dental prostheses. Although longitudinal studies show excellent long-term outcomes, it is to the detriment of individual patients that community care may often not follow accepted standards and protocols as described in standard texts, such as this one.
Postoperative Complications
As with all dental procedures, complications may occur after root canal treatment. However, the incidence of long-term postoperative complications appears to be lower than for the alternatives, single tooth implants and fixed dental prostheses. The 10-year complication rate for retained root canal–treated teeth is approximately 4%, compared to approximately 18% for retained single tooth implant restorations. Typical complications include symptoms, swelling, and the need for retreatment. In endodontics, complications are recorded as failures according to the criteria described previously; in other disciplines, complications are generally not recorded as failures.
Prognostic Indicators
The classic landmark study published by Larz Strindberg in 1956 related treatment outcomes to biologic and therapeutic factors. Factors now considered to be predictors of success and failure include (1) apical pathosis, (2) bacterial status of the canal, (3) extent and quality of the obturation, and (4) quality of the coronal restoration. The role of these factors should be discussed with the patient before and after treatment.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


