Fig. 5.1
Gingiva–anatomic crown relationship. Type I – the gingival margin is located incisal to the cementoenamel junction, and the gingival dimension is prominently wider from the margin to the mucogingival junction (a, b). Type II – normal dimension of the gingival margin to the mucogingival junction (c, d)
Alveolar crest-cementoenamel junction relationship (Fig. 5.2) – this can be divided in subtype A (where the distance between these structures is around 1.5 mm, and a normal attachment of gingival fibers into the cementum is observed) or subtype B (both structures are at the same level) [8].
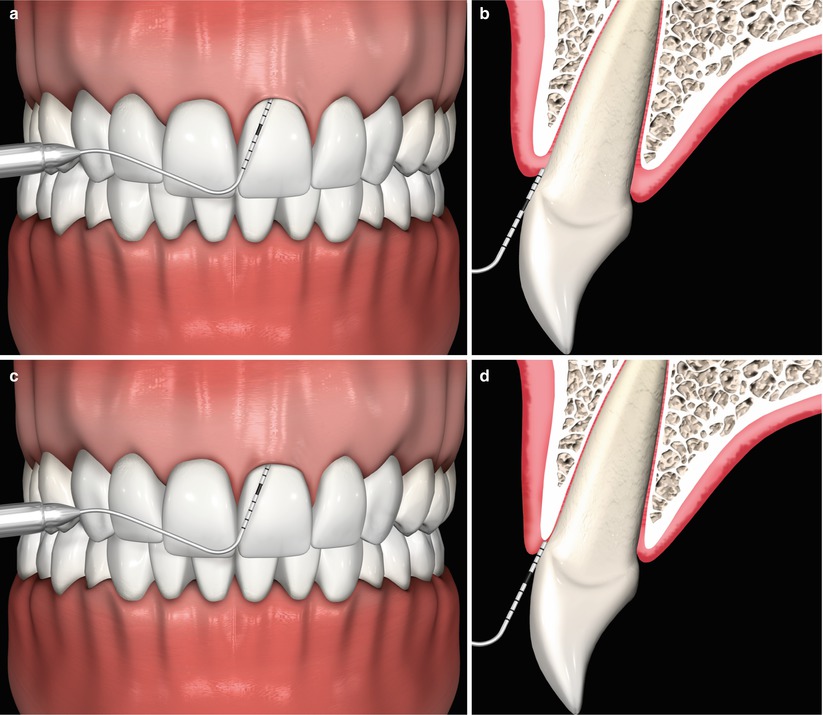
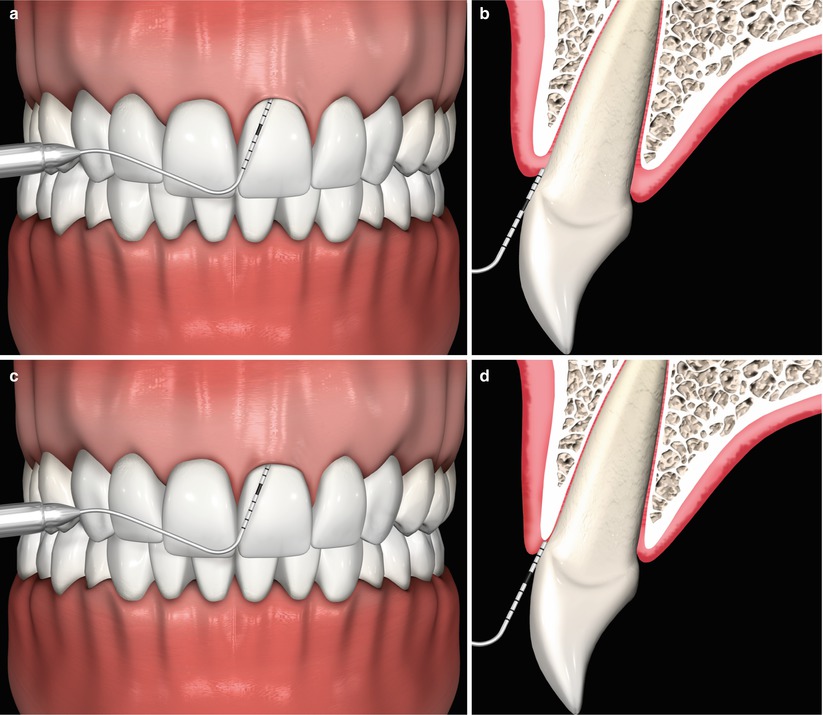
Fig. 5.2
(a–d) Alveolar crest–cementoenamel junction relationship. Subtype A – the distance between these structures is around 1.5 mm, and a normal attachment of gingival fibers into the cementum is observed (a, b). Subtype B – both structures are at the same level (c, d)
In addition, the knowledge on the anatomical characteristics of periodontal tissues of maxillary anterior teeth (i.e., gingival zenith and location of the alveolar bone crest with respect to the cementoenamel junction) and smile line/facial structures may be used clinically to determine the ideal unilateral positioning of the gingival margin during periodontal surgical treatment alone or in combination with multidisciplinary approaches involving orthodontic and prosthetic therapies [17].
5.1.3 Esthetical Clinical Crown Lengthening: “What May Be Expected After the Use of Periodontal Plastic Surgery Procedures?”
Despite being considered of more esthetic than of functional concerns, it has been demonstrated that an excessive gingival display (or gummy smile) may have a detrimental impact on the opinion of “a patient’s attractiveness, friendliness, trustworthiness, intelligence, and self-confidence” [14].
Descriptions of the use and outcomes of clinical lengthening procedures for the correction of anatomical discrepancies of the gingival and osseous architectures (e.g., altered dental eruption), gummy smile, and prior to prosthetic restorations may be found in the literature, and these approaches have encompassed the use of periodontal surgical techniques alone or in association to restorative procedures:
-
Pontoriero and Carnevale [9] evaluated the stability of the marginal periodontal tissues up to 12 months following surgical crown lengthening performed at the anterior and posterior teeth. A mean gingival coronal displacement of the gingival margin of 1.2 mm was found at buccal/lingual sites and 0.5 mm at interproximal sites from the end of the surgical procedure to the last follow-up – this outcome seemed associated to thick periodontal biotypes.
-
Lanning et al. [10] observed that the biological width is reestablished to its original dimension 6 months after surgery, as well as when the amount of bone to be removed is based on the future margins of the restoration and the original length of the biological width – definitive restorations may be performed 3 months after treatment (even in esthetic areas).
-
Deas et al. [11] also observed a significant gingival rebound of 30.8 % of gain of crown height achieved with surgical procedure, 6 months following treatment, related to the flap position over the alveolar bone crest at suturing.
-
Joly et al. [12] described a minimally invasive flapless approach valid for patients presenting a wide band of keratinized tissue and thin bone (i.e., patients with a thin or intermediate biotypes).
5.1.4 Type of Defect/Condition to Be Indicated
Treatment of patients with high smile line (gummy smile) or with discrepancies in the gingival margin (zenith) of anterior teeth that may impact the patient’s esthetics (i.e., patient’s personal report describing a deteriorated esthetic appearance due to its “gingival smile”)
5.1.5 Type of Defect Not to Be Indicated
Exposure of no more than 2 mm of gingival tissue during a natural smile (i.e., medium or low smile line) and in areas where the stability of the dentition may be compromised
5.1.6 Basics of the Surgical Sequence
For the flapless esthetic clinical crown lengthening procedure [12], an adequate band of keratinized tissue and a thin bone should be present. In this procedure, sulcular or inverted beveled incisions are performed on the anterior teeth requiring crown lengthening based on the amount of bone/soft tissue to be removed and the new position of the gingival margin established (in relation to the cementoenamel junction). This may be facilitated with the assistance of a diagnostic wax-up, a clinical mock-up, and an acrylic individual surgical guide since it assists the picturing of the future position of gingival margins and restorations’ shape (when indicated). These steps permit a more accurate, predictable, and less traumatic/invasive surgical procedure. After that, the collars of gingiva should be removed, and osseous remodeling takes place via “gingival sulcus” using micro-chisels, and no suture procedures are required (Fig. 5.3).


Fig. 5.3
(a–e) Esthetical clinical crown lengthening – flapless procedures [12], baseline (a), clinical mock-up positioned determining the future gingival margin and guiding the external beveled incisions (b), removal of gingival collars (c), osteotomy via the gingival sulcus (d), no sutures are performed (e)
With respect to the conventional surgical procedure, full-thickness flap rising should be performed after the removal of soft tissue collar. Osseous resection may be carried out using chisels or rotatory instruments with carbide burs, and the flap is positioned at the level or apical to cementoenamel junction (based on the periodontal/restorative treatment proposed) and sutured by 5-0 or 6-0 nylon/Teflon sutures (Fig. 5.4). The sutures are removed 14 days after surgery. In addition, patients should be instructed not to brush the teeth in the treated area, as well as they are prescribed 0.12 % chlorhexidine gluconate and instructed to rinse gently twice a day for 2–3 weeks, or until safe and comfortable toothbrushing can be performed. Overall, like all other periodontal plastic surgery procedures, analgesics, anti-inflammatory drugs, and/or systemic antibiotics are prescribed if needed, as well as no adverse effects are expected in the treated sites.
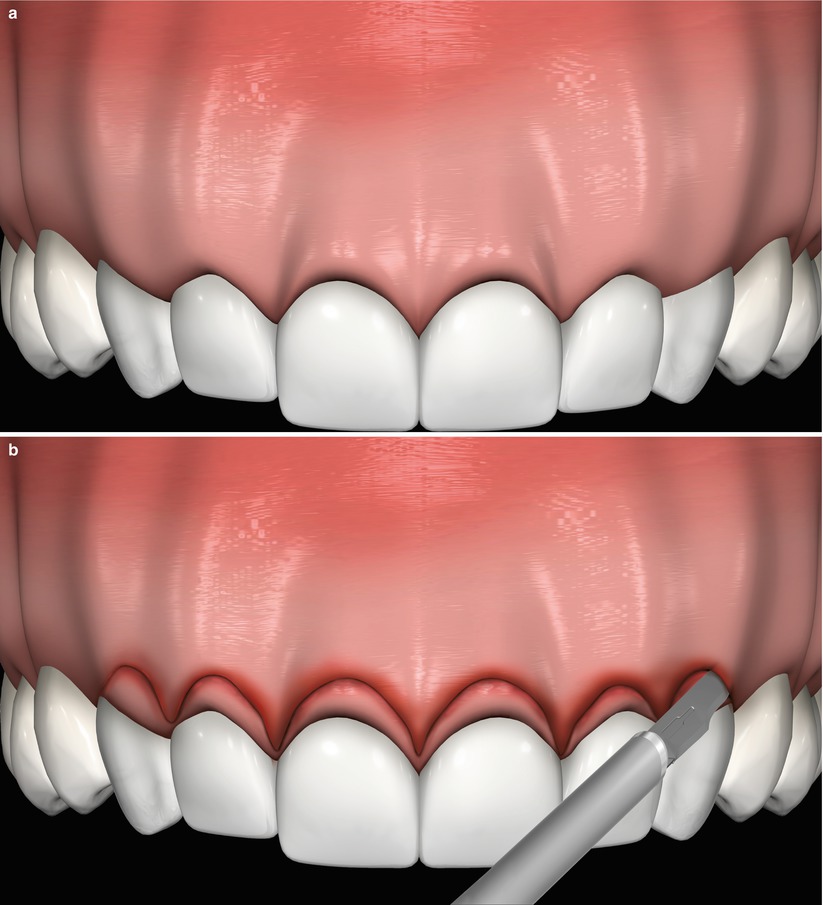
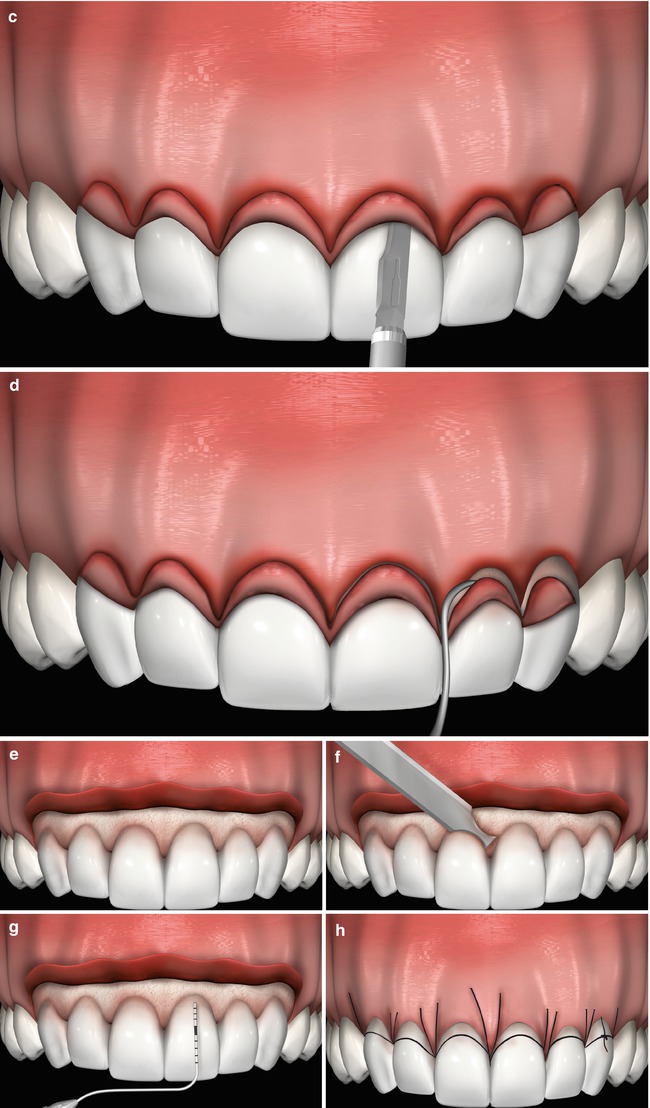
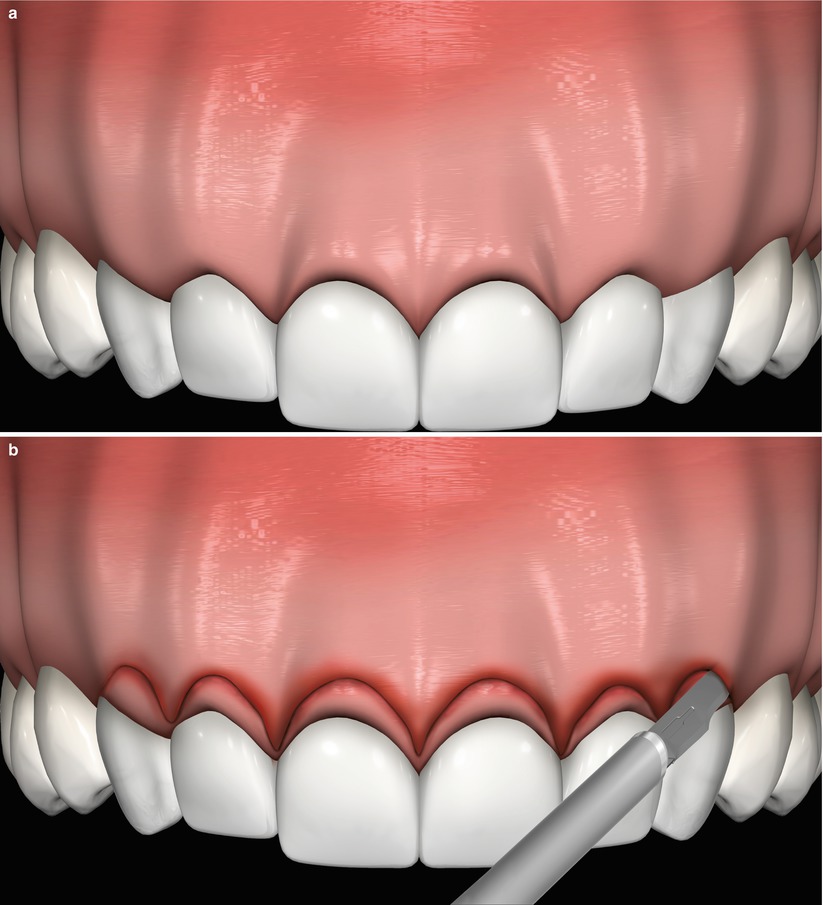
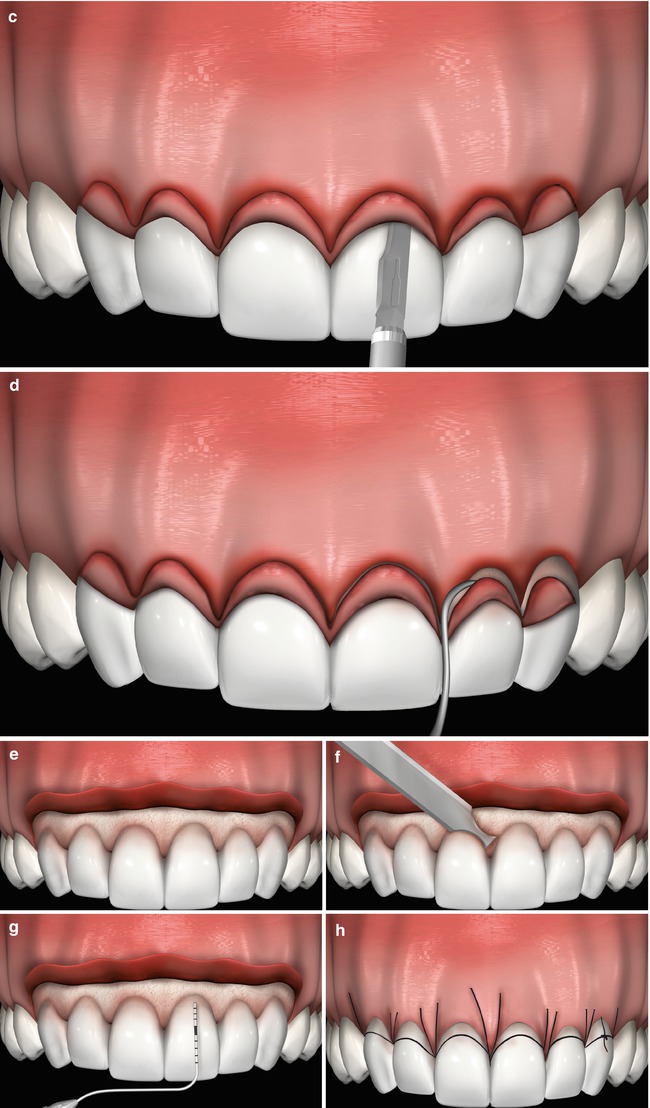
Fig. 5.4
(a–h) Baseline (a), external beveled incision (b) Intrasulcular incisions (c). Gingival collar removal (d). Full-thickness flap raised (e). Osteotomy and osteoplasty (f). Checking the distance of the alveolar crest to the cementoenamel junction (g). Flap positioned and sutures apically (h)
5.1.7 Orthodontic Tooth Extrusion: “Can Orthodontics Act as a Coadjuvant to the Use of Periodontal Plastic Surgery Procedure?”
Orthodontic extrusion associated with periodontal flap surgery or fiberotomy, during or immediately after extrusion, may be considered an additional resource for single tooth requiring esthetical clinical crown lengthening [20]. Fiberotomy has the advantage of preventing the return of the dental structure to its original position or the concomitant extrusion of both soft and hard tissues, which may lead to the need of additional plastic periodontal surgical procedures [20]. However, in sites lacking interpapillary gingiva, orthodontic extrusion without fiberotomy may provide superior esthetical gains (Figs. 5.5 and 5.6).
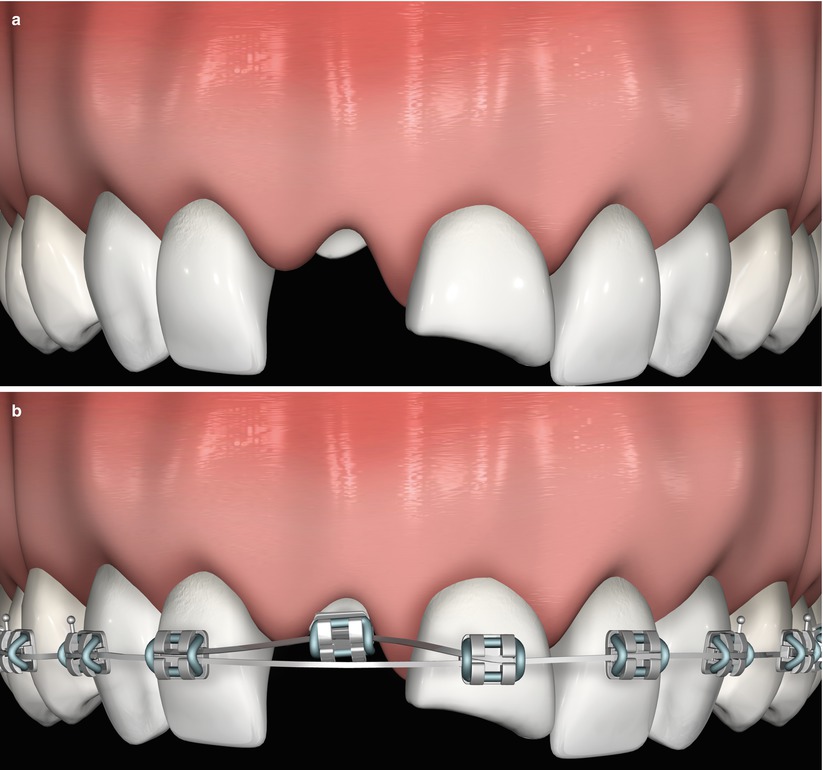
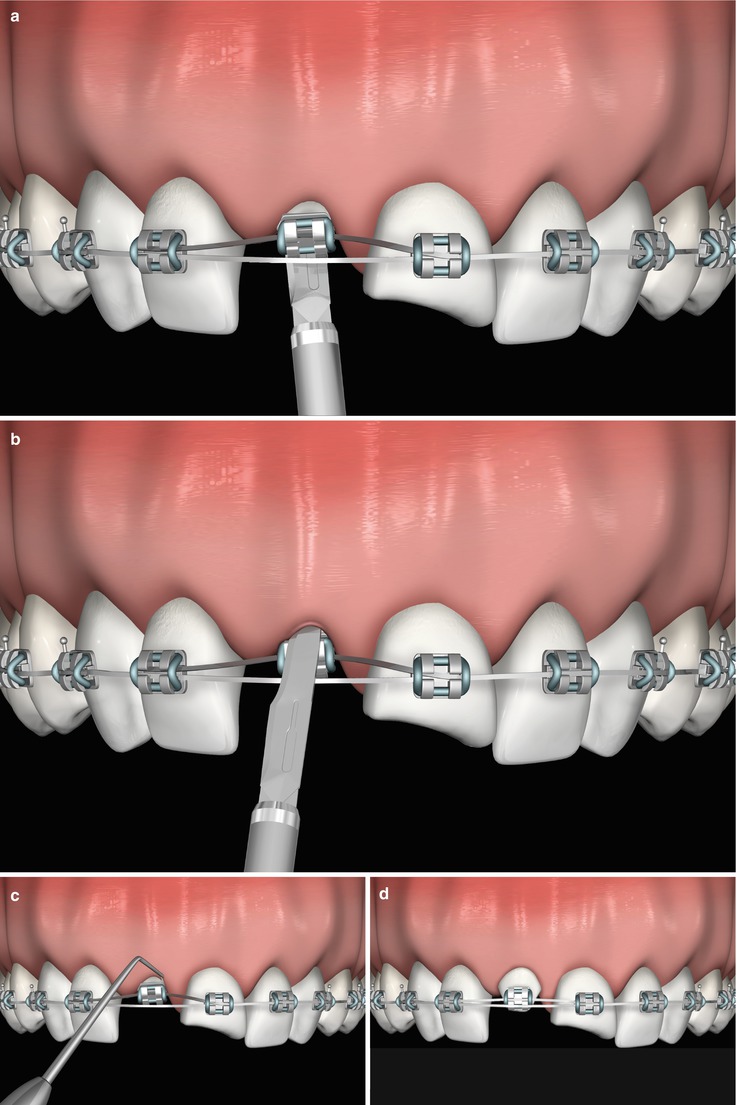
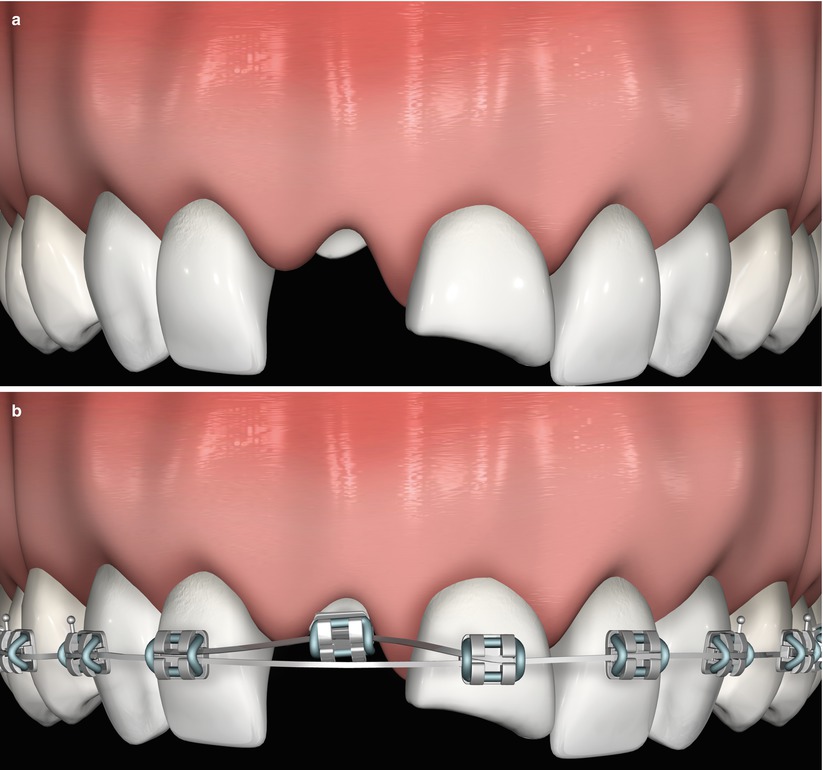
Fig. 5.5
Orthodontic tooth extrusion associated to fiberotomy in esthetic areas. Baseline – one or more teeth presenting fractures or caries invading the biological width (a). Use of partial fixed orthodontic appliance – passive bonding (in the same horizontal plane) of 0.022-in. brackets from the first right bicuspid to the first left bicuspid (on the tooth to be extruded, the bracket is positioned more apically to provide an extrusive component), placement of a 0.014-in. nickel–titanium arch wire and a 0.019 × 0.025 in. stainless steel auxiliary arch used to stabilize the segmented wire (b)
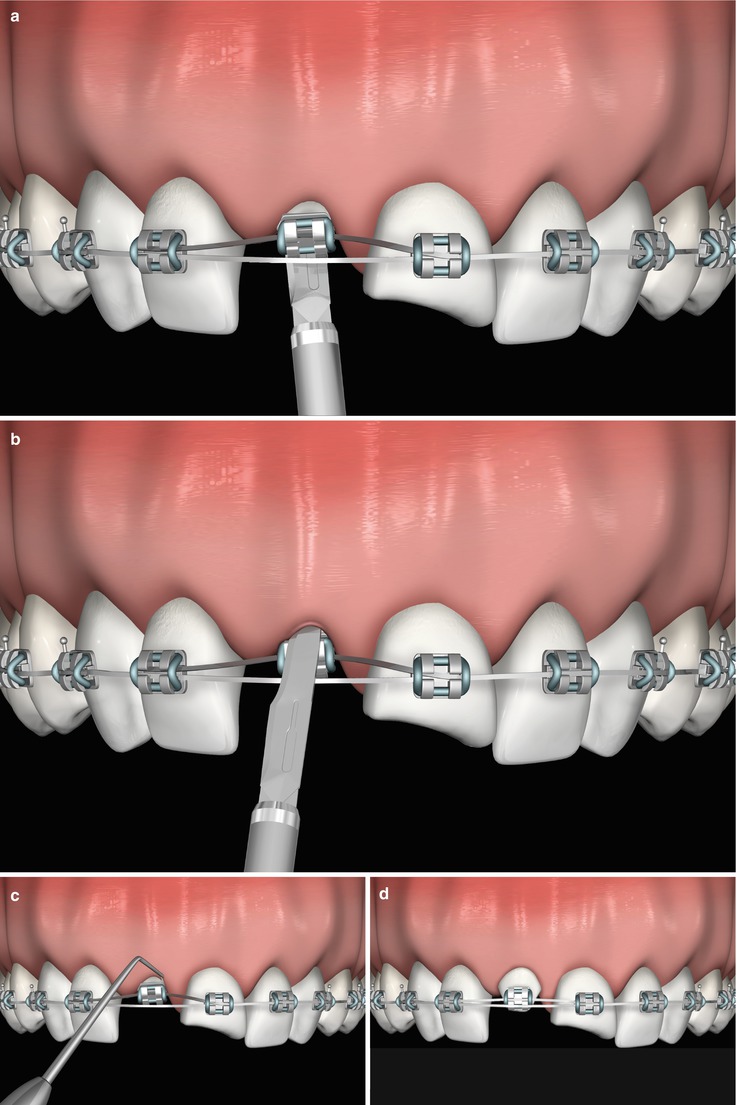
Fig. 5.6
Palatal intrasulcular incision (a). Buccal intra sulcular incision (b). Scaling and removal of supracrestal gingival fibers (c). Orthodontic extrusion without changes in the gingival margin (d)
5.1.8 Clinical Remarks: Implications for Practice and Clinical Decision-Making on Esthetical Clinical Crown Lengthening
Most of the data on crown lengthening procedures regard to studies on teeth requiring restorative approaches. Indeed, just one randomized trial on the treatment of anterior teeth exclusively due to esthetical purposes (on multiple teeth) was published up to now [13]. Overall, the outcomes accomplished by the use of esthetical clinical crown lengthening procedures, in clinical terms, may improve patients’ esthetics because of the harmonization of the gingival tissues and teeth and the concomitant improved balance between lips, gingiva, and facial profiles [13]. These favorable conditions will result in more stable outcomes that may be maintained for long-term periods when the patients’ full-mouth plaque score is less than 20 % [16].
The use of flapless approaches may decrease gingival height and volume, as well as lead to a minimal injury to the blood vessels and tissues, a reduced surgical morbidity, a more uniform healing process, and prevent the formation of scars [12, 13, 16]. Additionally, multidisciplinary treatment plans based on a diagnostic wax-up and a mock-up may guide the surgical procedure, reduce the gingival trauma, and assist posterior prosthetic treatment planning with restorative/prosthetic laminate veneers or full crowns. For such cases, the locations of the future biological width should be anticipated. However, information on the long-term maintenance of results have not been established yet, thus the potential of tissue regrowth (specially within patients presenting a thick periodontal biotype) should be assessed during wound healing in order to establish the best time for the subsequent definitive restorative treatment when intrasulcular prosthetic margins are planned to complete the case [9, 11].
Additionally, when multidisciplinary approaches were indicated for teeth presenting color alterations, shape deformities, irregular positioning in the dental arch, inadequate contact points, cervical lesions, and excessive occlusal wear, these should be carefully planned. The establishment of a proper crown length/width ratio may improve the outcomes of surgical procedure (i.e., central incisors > canines > lateral incisors) as it may provide an improved balance between teeth and gingiva during a smile (a better distribution of the six teeth of the anterior maxillary sextant) [7]. Within treatment planning involving ceramic crowns or laminated veneers, these should present smooth and precise margins located no more than 0.5 mm into the gingival sulcus, as well as a minimum of 3 mm distance of the margins of the restorations to the alveolar bone crest should be respected to prevent gingival inflammation and periodontal attachment loss [22, 23]. Provisional dental preparations and restorations (for porcelain veneers or full crowns) may be performed approximately 30 days after surgery, whereas definitive prosthetic restorations may be fabricated after full healing of periodontal tissue (i.e., 6 months postsurgery) [6]. As a general rule, the stability of the soft tissues surrounding ceramic crowns or laminated veneers will be directly linked to the health of periodontal tissues (e.g., lack of plaque-induced periodontal diseases), to the minimum trauma during intrasulcular margin placement and gingival displacement procedures, to the quality of provisional restorations, to the complete removal of excess of temporary and final cements, and the wait for the proper follow-up healing period after surgery before installing the definitive restorations [22].
Finally, the orthodontic extrusion may improve the esthetic crown lengthening as well. It should be performed based on clinical and radiographic data obtained at initial examinations, as well as it should be kept in mind that these may not provide an exact measurement of the amount of tooth/root to be extruded. When orthodontic extrusion was associated to circumferential fiberotomy, it does not lead to significant changes in the gingival and osseous tissues’ anatomy. Conversely, conventional orthodontic extrusion (without fiberotomy) may improve the amount of soft tissue in interproximal areas and favor the achievement of better gingival contours when associated to crown lengthening surgery (Figs. 5.7, 5.8, 5.9, 5.10, 5.11, 5.12, 5.13, and 5.14).
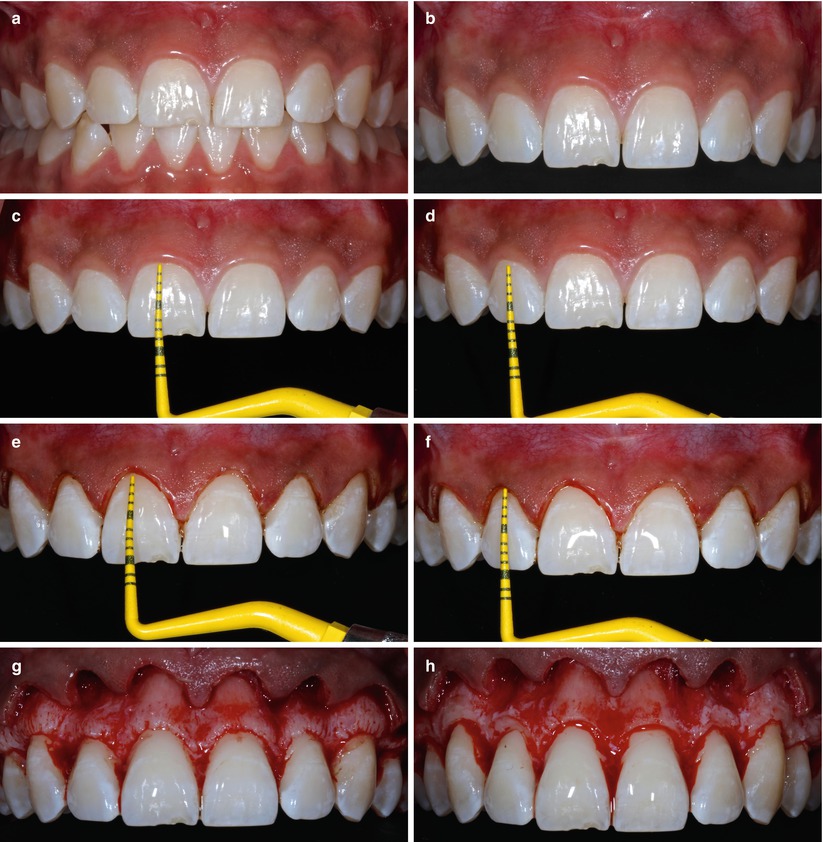

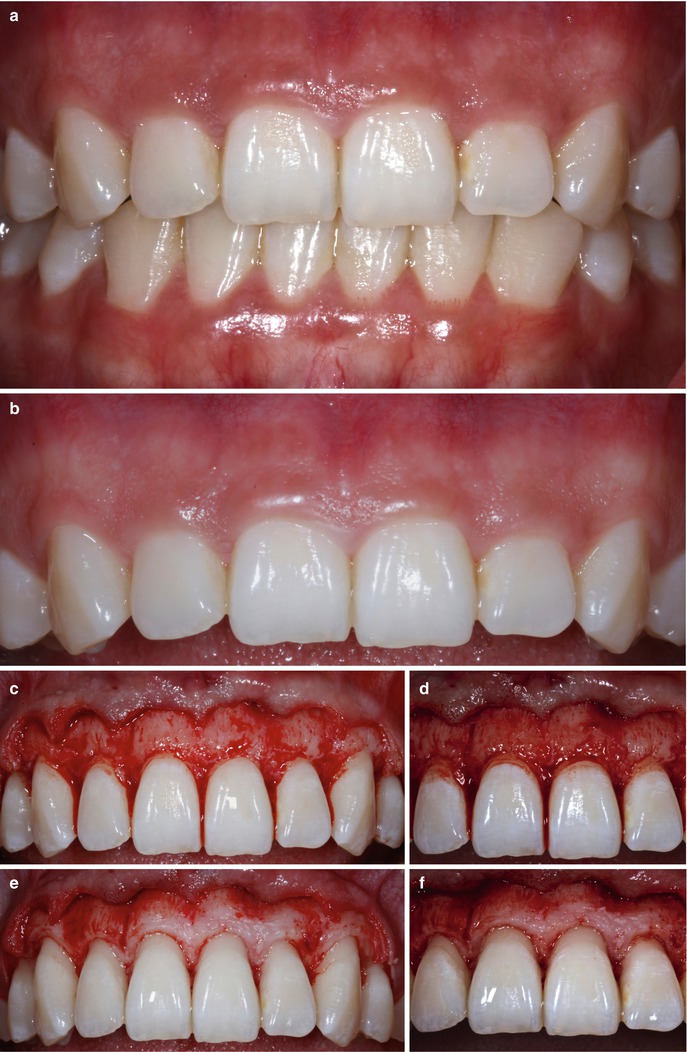



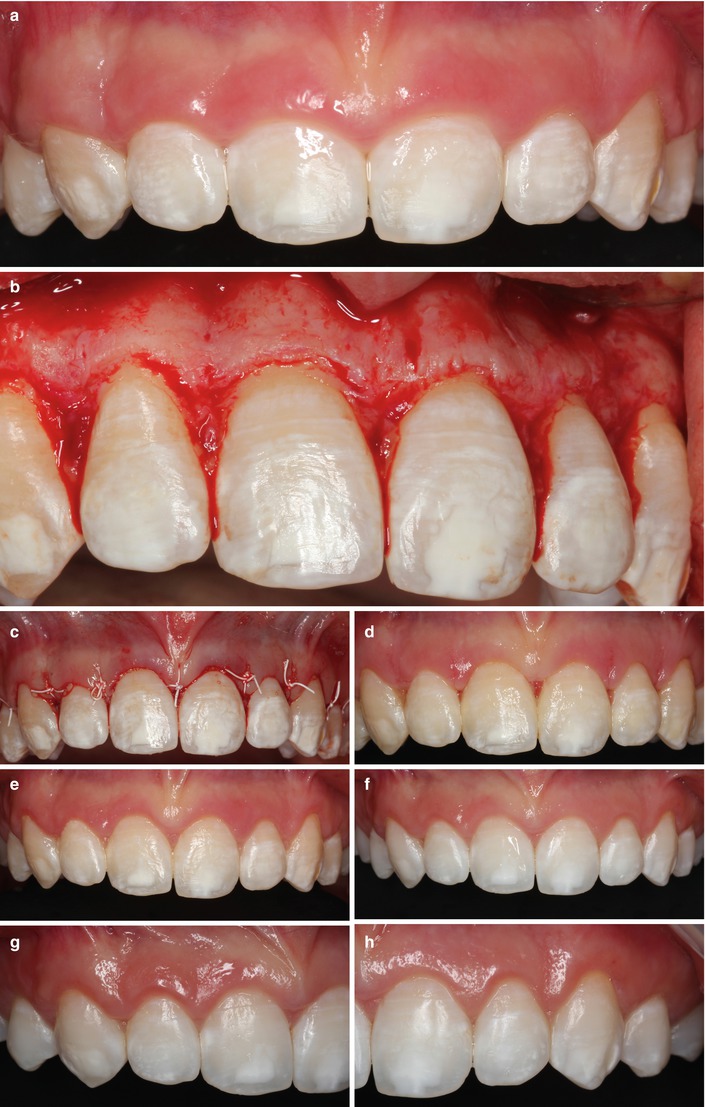


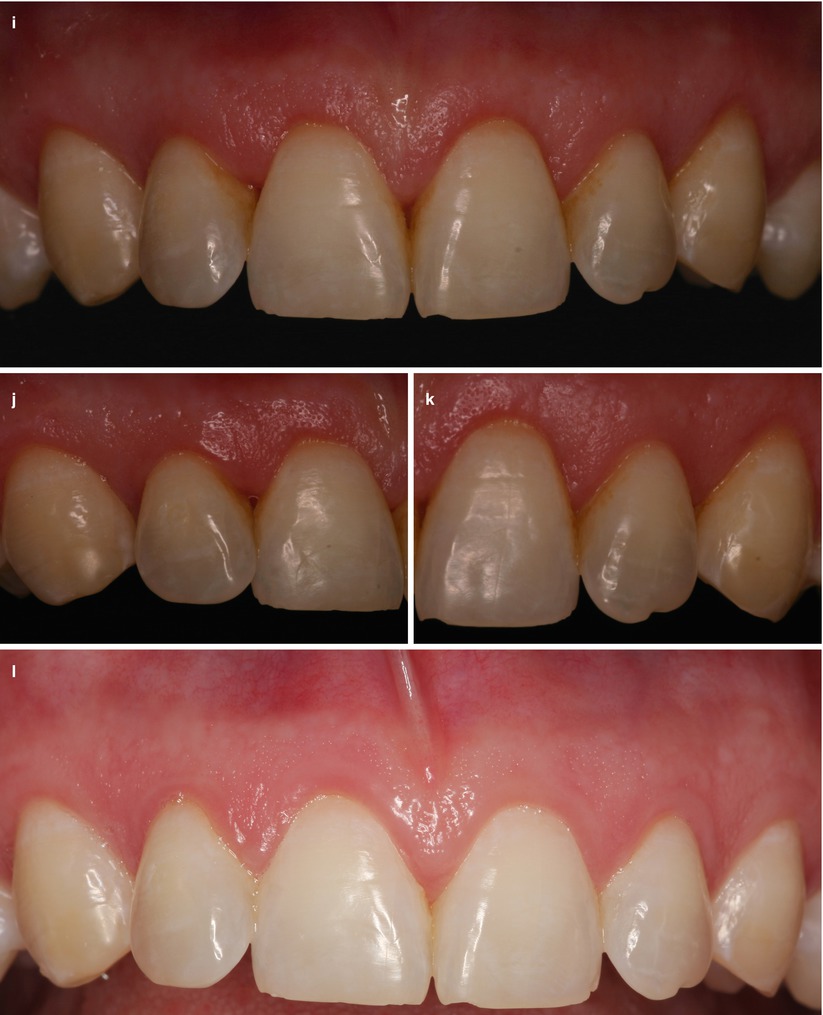
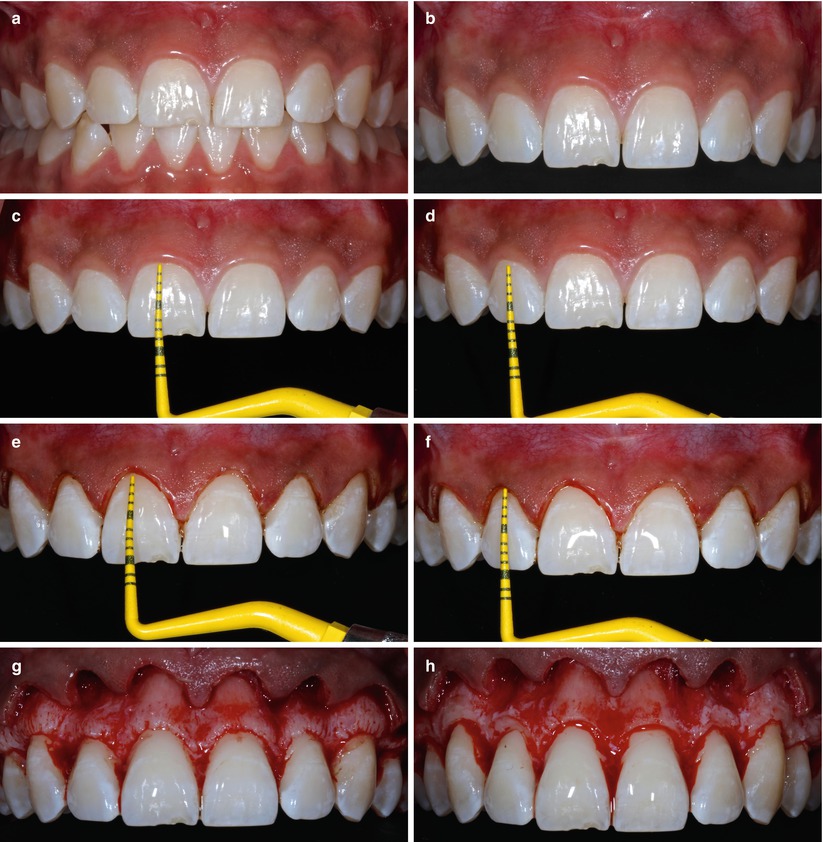

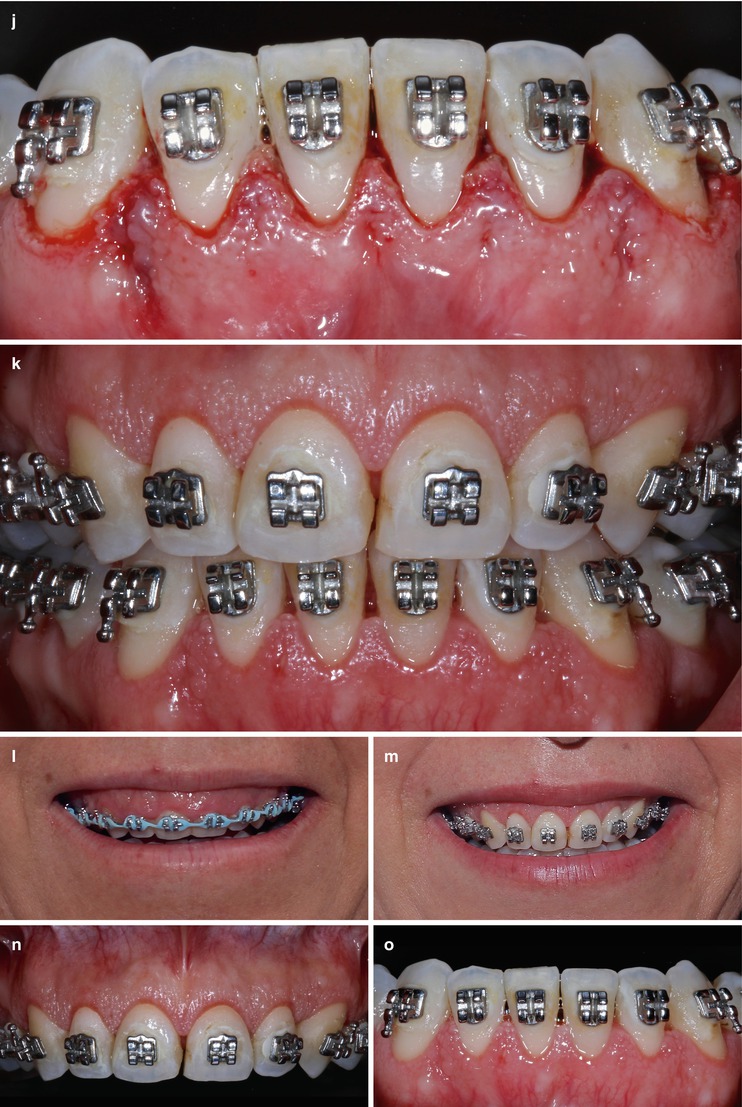
Fig. 5.7
Case I – 8 (a–n) Esthetical clinical crown lengthening of maxillary anterior segment. Baseline – gingiva–anatomic crown relationship type I (a, b). Checking crown length on central incisors (c). Checking crown length of lateral incisor (d). Rechecking of clinical length of central incisors after removal of gingival collar (e). Rechecking of clinical length of lateral incisors after removal of gingival collar (f), alveolar crest–cementoenamel junction relationship subtype B (g). Osseous contour after osteotomy and osteoplasty procedures (h). Flap positioned and sutured apically (i). Flap positioned and sutured apically (j). Smile appearance before (k) and after treatment (l) 3 months follow-up (m, n)
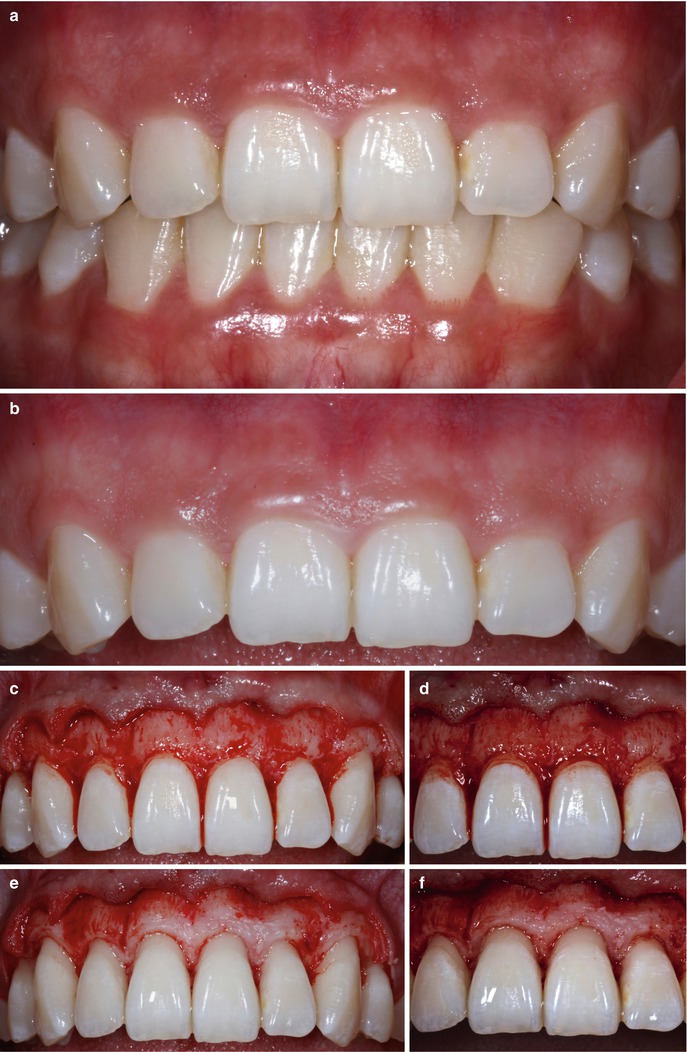

Fig. 5.8
Case II (a–l) Esthetical clinical crown lengthening of maxillary anterior segment. Baseline – gingiva–anatomic crown relationship type I (a, b). Osseous contour before osteotomy and osteoplasty procedures (c). Alveolar crest–cementoenamel junction relationship subtype B (d). Osseous contour after osteotomy and osteoplasty procedures (e). Change of alveolar crest–cementoenamel junction relationship to subtype A (f). Two weeks follow-up – immediately after suture removal (g). Three months follow-up (h). Baseline smile appearance (i). Final smile appearance (j). Gingival anatomy adjacent to upper incisors at 4 months follow-up (k), 4 months follow-up (l)

Fig. 5.9
Case III 10 (a–j) – Esthetical clinical crown lengthening of maxillary anterior segment. Baseline – gingiva–anatomic crown relationship type I (a, b). Incisions performed and gingival collar delimited (c). Clinical aspect during osteotomy and osteoplasty procedures (d). Flap positioned and sutured apically (e). Flap positioned and sutured apically(f). Smile appearance before surgery (g). Smile appearance after surgery – last follow-up (h). Four months follow-up (i, j)

Fig. 5.10
Case IV 11 (a–h) – Esthetical clinical crown lengthening of maxillary anterior segment. Baseline (a). After intrasulcular incision – no internal beveled incision was performed (b). Osseous contour at the central incisions (c). Osseous contour at the left lateral incisor (d). Osseous contour at the right lateral incisor (e). Flap sutured (f). Three months follow-up (g, h)
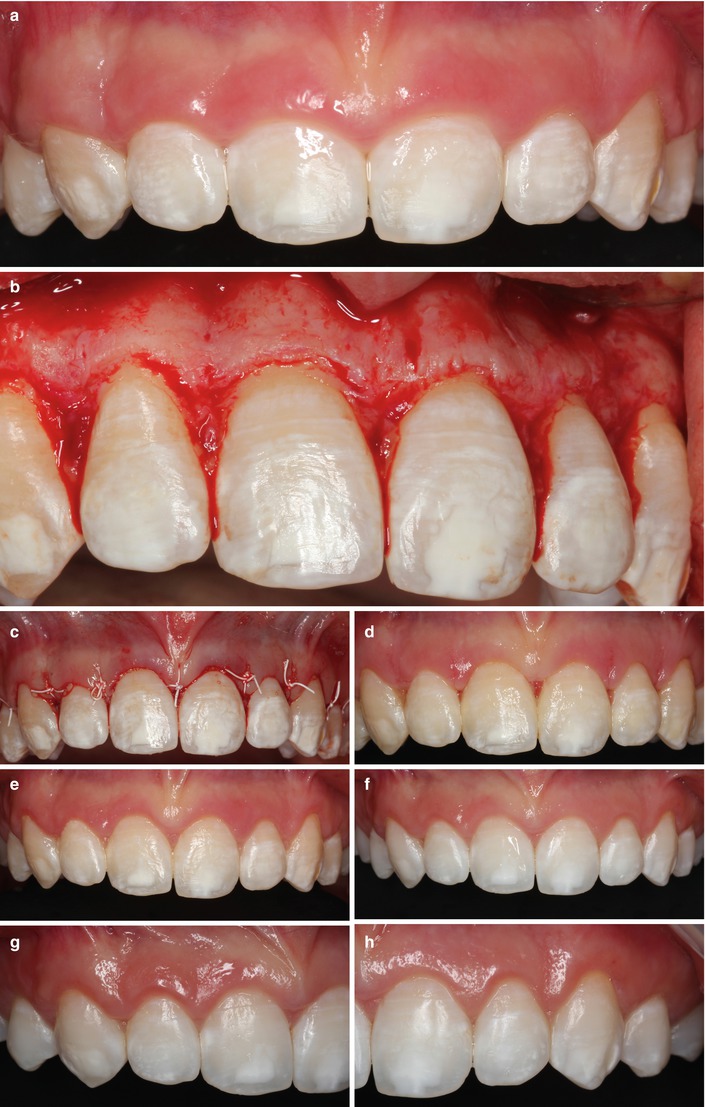
Fig. 5.11
Case V – Esthetical clinical crown lengthening of maxillary anterior segment. Baseline (a). Osseous contour after osteotomy and osteoplasty (b). Flap positioned and sutured apically (c). Fifteen days follow-up (d). Three months follow-up (e). Six months follow-up (f–h)

Fig. 5.12
Case VI – Esthetical clinical crown lengthening of maxillary incisors, baseline (a, b). Gingival collar delimited by the incisions (c). Gingival collar removed (d). Osseous contour before osteotomy and osteoplasty procedures (e). Osseous contour after osteotomy and osteoplasty procedures (f). Flap apically positioned and sutured (g). Fifteen days follow-up (h). Smile appearance 3 months after surgery (i)

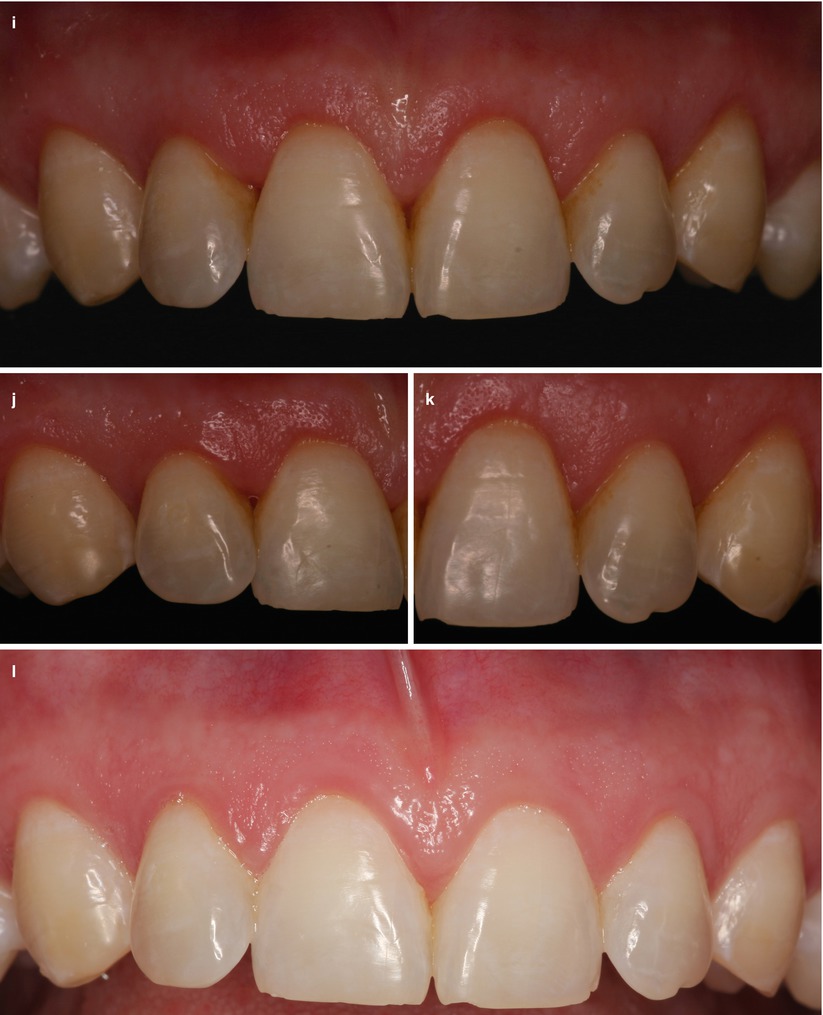
Fig. 5.13
Case VIII 14 (a–l) – Esthetical clinical crown lengthening of anterior maxillary teeth (a). Crown length: right canine (b); right lateral incisor (c), right central incisor (d), left central incisor (e), left lateral incisor and (f) left canine (g). Flap positioned and sutured apically (h), 6 weeks follow-up (i–k), 5 years follow-up (l)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses