Introduction
The purpose of this study was to determine the ability of orthodontists and orthodontic residents to identify nonorthodontic incidental findings and false positives in cone-beam computed tomography scans.
Methods
Two groups of 10 cone-beam computed tomography scans containing equal numbers of scans with no, 1, or several abnormal nonorthodontic lesions were selected from a database. Eight orthodontists and 8 orthodontic residents screened the 2 groups of scans before and after a basic cone-beam computed tomography training course. The paired t test was used for statistical analyses.
Results
In the initial screening, the orthodontists and residents correctly identified 41.1% of the lesions. This lesion-detection rate improved significantly to a mean of 56.7% after the training course ( P <0.0005). In parallel with these findings, the mean percentage of correctly identified extragnathic lesions improved significantly, from 22% to 48% ( P <0.0005), and correctly identified temporomandibular joint lesions improved from 20% to 55% ( P = 0.01) after the training. In contrast, the rate of correctly identified dentomaxillofacial lesions remained largely unchanged before and after the training. Both groups of evaluators had approximately 5 false positives per 10 scans before training and demonstrated significant decreases in false positives after training.
Conclusions
Relative to known error rates in medical radiology, both groups of evaluators had high error rates for missed lesions and false positives before and after training. Given these findings and since the most frequent cause of medical radiology malpractice litigation is due to missed lesions, it is recommended that an appropriately trained radiologist should be involved in reading and interpreting cone-beam computed tomography scans.
Cone-beam computed tomography (CBCT) imaging has gained in popularity and use in orthodontics since its introduction to dentistry in 2001 because of its real and perceived advantages over 2-dimensional radiography. Some cases in which CBCT imaging has advantages over routine radiographs include localization of impacted teeth, visualization and quantification of maxillofacial skeletal discrepancies, and analysis of the temporomandibular joint and airway. Despite the lack of evidence of its efficacy for all routine orthodontic patients, CBCT scans are currently used in lieu of pretreatment cephalometric and panoramic radiographs by some orthodontists for all of their patients.
In deciding when to use CBCT in orthodontics, the clinician should perform a benefit-to-risk analysis. With CBCT, the 2 major risks to consider include the higher radiation dose to the patient over traditional 2-dimensional orthodontic views and the increased chance of missing significant findings in the larger scan volume. These potential sources of error include failure to identify incidental findings, detection of false positives, and failure to recognize a normal biologic variant.
On average, 3.5% to 8% of orthodontic and pediatric dental patients have significant incidental radiographic findings in panoramic and other 2-dimensional radiographs. Although most of these do not carry serious consequences for the patient, cases of unsuspected lesions of the cranial base and cervical spine have been reported in the literature. Since the CBCT scan has substantially more data than 2-dimensional radiographs and therefore is likely to capture more lesions both within and outside the dentomaxillofacial area, the rate of incidental findings is likely to be substantially higher in CBCT scans than in traditional radiographs. Indeed, approximately 25% of CBCT scans taken for various dental and orthodontic needs have incidental findings, including airway, temporomandibular joint, and endodontic findings. Another study showed 701 “reportable” findings in 381 CBCT cases, including pharyngeal masses, blocked ostia, suspected tumors, and undiagnosed fractures.
In parallel with the concern about missed lesions is the problem of overdiagnosis or the detection of false positives. A perceived abnormal lesion, which in reality is a normal biologic variant or artifact with no clinical significance, might prompt the orthodontist to prescribe further unnecessary follow-up. Thus, the negative sequela of a false-positive diagnosis includes the costs and complications that can arise from additional unnecessary diagnostic procedures or treatments, or both, and the emotional and financial toll on the patient and the patient’s family.
The lack of identification of an incidental lesion or a false-positive diagnosis exposes the clinician to substantial liability. Although at this time there are no legal cases reported against dentists for failure to diagnose from CBCT scans (Bernard Friedland, DMD, JD, personal communication), the standard of care for the profession is that images should be read in their entirety. Also, although no information is currently available on error rates for CBCT scans for radiologists and other dental professionals, the rates of missed lesions by nonradiology specialists using panoramic radiographs have been found to be higher than those of oral and maxillofacial radiologists. Considering the high volume of data in CBCT scans and orthodontists’ lack of optimal educational background and skill in reading images from these scans, it is likely that orthodontists have a high error rate in identifying incidental lesions or of false-positive diagnoses. However, no study to date has determined the capability of orthodontists to identify incidental findings and assess their false-positive error rates when screening CBCT scans.
The purposes of this study were to (1) determine and compare the current capabilities of orthodontists and orthodontic residents in identifying incidental nonorthodontic abnormalities and assess their false-positive diagnoses in CBCT scans, and (2) evaluate any improvement in lesion detection rates and false-positive diagnoses after basic CBCT training provided by an oral and maxillofacial radiologist. These findings provide insights into whether orthodontists have the skill set to optimally diagnose incidental findings, demonstrate methods to improve these capabilities in reading CBCT scans, and provide a sense of the appropriate management of CBCT data to minimize adverse consequences to patients or medicolegal risks to providers, or both.
Material and methods
This study was approved by the Institutional Review Board at the University of Michigan, Ann Arbor (approval number HUM00016717). Twenty scans were selected by an oral maxillofacial radiologist from a database of CBCT scans at the Department of Oral Radiology. All the scans were taken with the i-CAT (Xoran Technologies and Imaging Sciences International, Hatfield, Pa) CBCT scanner. The images were taken at 120 kVp, 18.66 mAs, with image resolution of 0.4 mm voxels. The 20 scans were divided into groups A and group B of 10 scans each, with each having equal numbers of scans with no, 1, or several abnormal, nonorthodontic incidental lesions that had previously been identified by a board-certified oral and maxillofacial radiologist (S.L.B.) ( Table I ). The lesions were selected to represent the types of conditions that might be expected to occur in a healthy population: typical patients visiting orthodontists. Lesions included rarefying osteitis, condensing osteitis, enlarged dental follicles, calcified pineal gland, mucous retention pseudocyst, generalized mucosal thickening in the maxillary sinus, tonsilloliths, carotid artery calcifications, periapical cemento-osseous dysplasia, thyroglossal duct cyst in the hyoid bone, and degenerative changes in the temporomandibular joints. No lesion was biopsied because treatment was not indicated in any patient. No malignant lesion was included in the sample because a malignant lesion would be an unlikely incidental finding in a healthy young patient.
| Lesions | Group A | Group B | |
|---|---|---|---|
| Total | 9 | 9 | |
| Location | Dentomaxillofacial | 4 | 4 |
| Extragnathic | 5 | 5 | |
| Temporomandibular joint ∗ | 2 | 2 |
∗ Temporomandibular joint lesions are included in extragnathic lesions and also shown separately.
Each group contained 9 lesions: 4 lesions were in the dentomaxillofacial complex and 5 were extragnathic lesions. Of these extragnathic lesions, 2 involved the temporomandibular joint. The radiologist established the gold standard for identification and location of the lesion by viewing multi-planar reconstructed and 3-dimensional views of all CBCT scans. Multi-planar reconstructed evaluation refers to the viewing of consecutive reconstructions of the images in the coronal, axial, and sagittal planes.
The ages of the subjects for the selected scans ranged from 9 to 53 years, with an average age of 22.6 years. Scans from patients with craniofacial anomalies or who were edentulous were not included in the study. Eighteen (90%) of the scans had a field of view covering the entire craniofacial complex (13 cm in height), and 2 (10%) of the scans had a field of view covering the maxilla and the mandible (6 cm in height). The CBCT scans were saved as deidentified Digital Imaging and Communication in Medicine (DICOM) format for import into the viewing software. Panoramic views, between 10 and 14 mm in thickness, were reconstructed from each scan and saved as JPEG files.
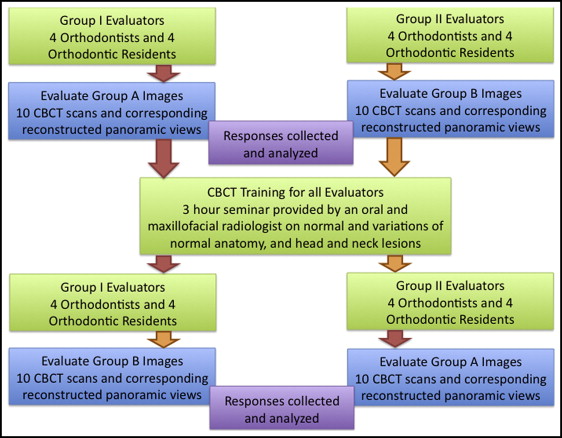
Sixteen evaluators, including 8 orthodontists trained in the United States and 8 orthodontic residents, were divided into 2 groups composed of equal numbers of orthodontists and residents and asked to evaluate the scans of either group A or group B ( Fig 1 ). The orthodontists had an average of 16.8 years in practice, and 75% were certified by the American Board of Orthodontics. The orthodontic residents, in their second year of residency, had all graduated from 4-year accredited American or Canadian dental schools. Before viewing any scans, each evaluator signed an informed consent.
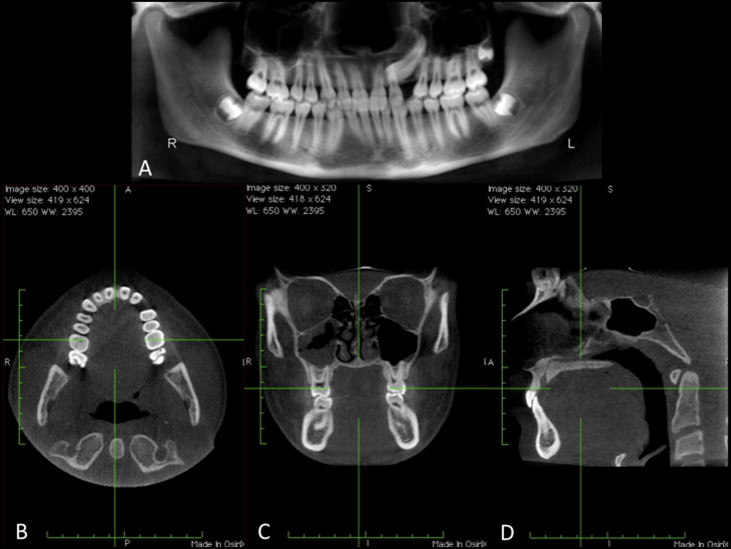
The scans were viewed dynamically by using Osirix X (3.2.1 32-bit version; Openware, Geneva, Switzerland) for the multi-planar reconstructed views, and the panoramic reconstructions were viewed with PowerPoint (Microsoft, Redmond, Wash) ( Fig 2 ). All images were examined on a MacBook Pro laptop with a 17-in screen (Apple, Cupertino, Calif). A CBCT scan, not among the ones used in the study, was used to demonstrate the operation of the Osirix X software. The evaluators were allowed to view the multi-planar reconstructed images from this scan until they were comfortable in manipulating the scans and the software. All scans were viewed by the evaluators as multi-planar reconstructed sections in the axial, sagittal, and coronal planes, as well as the reconstructed panoramic view ( Fig 2 ). The evaluators were permitted to scan through all 3 planes in the entire scan, toggle back and forth between any views as needed, and ask operational questions about the Osirix X software throughout the screening. Osirix, as does all other currently available software, enables the examiner to view and scroll through multi-planar reconstructions in all 3 planes of space. Since no examiner had previously used any commercially available imaging software including iCATvision, and because the examiners were guided in the use of Osirix by the investigator (F.A.) throughout their evaluations of the scans, the effects of the use of this software relative to those available commercially was considered to have a minimal impact on the outcome of the study.
For the pretraining evaluation, each evaluator was randomly assigned to either group A or group B scans with equal numbers of evaluators per group of scans ( Fig 1 ). The evaluators were asked to screen the images in all planes (axial, coronal, and sagittal as well as the reconstructed panoramic view) for any lesions that were not directly related to orthodontic diagnosis and treatment planning that they thought required either further follow-up by another health care provider or observation by himself or herself. The evaluators were informed that their goal was only to detect any abnormality, not to diagnose it. The evaluators were asked to identify the orientation (axial, coronal, sagittal sections) and slice numbers where the lesion was visible if seen in the multi-planar reconstruction view, or to describe the anatomic location if seen on the panoramic view. The information on lesion location was necessary to compare with the gold standard to ensure that the evaluator had identified the correct lesion in the scan.
Approximately 4 weeks after evaluation of the first set of scans, the evaluators were given a 3-hour course on screening CBCT images by an oral and maxillofacial radiologist (S.L.B.). The course provided instructions on how to read CBCT scans and information about the appearance of normal anatomy and normal variations of the anatomy in the head and neck regions on a CBCT scan. The evaluators were also trained in identifying lesions in the scans by using several examples of radiolucent and radiopaque anomalies and pathologies in the dentomaxillofacial complex, maxillary sinus, temporomandibular joint area, neck, and brain. The training course did not include any CBCT scan used in the study. The evaluators could ask questions during the course.
Within 8 weeks after the training course, each evaluator assessed either the group A or group B scans that he or she had not previously examined. The scans were viewed under the same settings and conditions as before the training course. The primary investigator (F.A.) then tallied the evaluators’ correct responses and false positives against the gold standard.
Statistical analysis
The data were reported as mean numbers and percentages (±SD) of correctly identified lesions, types and locations of lesions, and false positives. The percentage of correctly identified lesions was also calculated by using the following formula:
% correct lesions detected = number of correctly identified lesions number of lesions present × 100
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


