Introduction
A new, highly filled primer is currently marketed as a fluoride delivery system effective in reducing white spot lesions in orthodontic patients. However, no studies in the literature support this claim. The purpose of this in-vivo study was to investigate the retention and the efficacy of this primer in reducing the formation of white spot lesions.
Methods
In each patient for whom premolar extractions were planned (n = 22), 1 premolar was randomly chosen as the experimental tooth for the application of the fluoride delivery system (Opal Seal; Ultradent Products, South Jordan, Utah), and the contralateral tooth was assigned as the control to receive the standard treatment (Transbond XT; 3M Unitek, Monrovia, Calif). After the bonding procedures, separators were placed around the premolar brackets to encourage plaque retention over 8 weeks. After the extractions, the tooth surfaces were evaluated visually and with microhardness techniques for demineralization. Primer retention was also investigated.
Results
There were no statistically significant differences in the numbers of white spot lesions between the 2 groups. The primer retention was calculated as 50%.
Conclusions
The results indicated no significant difference between the efficacies of the fluoride-releasing primer and the control primer in reducing demineralization over the duration of the study.
During orthodontic treatment, formation of white spot lesions (WSLs) around brackets has long been recognized as a potential risk. WSLs, a clinically detectable manifestation of subsurface enamel demineralization, represent the early stages of caries formation. WSLs exhibit up to 50% reduction in enamel mineral loss. Because of this mineral loss, there are changes in the hardness and refractive index of the enamel, causing scattering of light and giving the enamel a chalky, opaque appearance.
WSLs can develop in the gingival areas of teeth in as little as 4 weeks after bracket placement. The high incidence of WSLs is attributed to prolonged plaque retention around brackets, since it is more difficult for orthodontic patients to perform effective oral-hygiene measures with orthodontic attachments. Unfortunately, WSLs often persist and cause esthetic dissatisfaction at the end of orthodontic treatment.
Scientific evidence for the use of fluoride to prevent enamel demineralization is well established. Fluoride ions delivered through mouth rinses, varnishes, gels, and fluoride-releasing cements have been reported to reduce the extent and incidence of WSLs during orthodontic treatment with fixed appliances. However, regimens to administer fluoride by topical application or home rinse programs are limited because of unpredictable patient compliance.
One approach to minimize demineralization, without a need for patient compliance, is the application of a resin sealant to the enamel surfaces. Although unfilled or lightly filled resin sealants have been shown to be effective in reducing demineralization in vitro, subsequent clinical studies have not supported these results. Newer highly filled sealants are reported to resist toothbrush abrasion. Therefore, these materials are effective in reducing enamel demineralization.
Recently, a new glass ionomer primer (Opal Seal; Ultradent, South Jordan, Utah) has become commercially available for use in orthodontic patients with poor oral hygiene. Because of its high filler content (38%), this product is claimed to exhibit long-lasting coverage and superior fluoride release and recharge abilities. In a previous study, fluoride ion release from a novel glass ionomer containing polymer was reported. Although it is possible that Opal Seal has a similar profile over a period of time, in the literature there is only 1 study that investigated its release and recharge abilities in vitro at 24 hours. The application of acidulated phosphate fluoride to the Opal Seal disks resulted in recharging the fluoride ions into the primer composition that would be available for subsequent release. Currently, in the literature, no clinical studies have evaluated the efficacy of Opal Seal in the prevention of WSLs in patients undergoing orthodontic treatment with fixed appliances.
The aims of this in vivo study were to (1) compare the efficacy of a new, highly filled fluoride releasing orthodontic primer (Opal Seal) with a conventional nonfluoride orthodontic primer (control, Transbond; 3M Unitek, Monrovia, Calif) in preventing demineralization adjacent to brackets using visual examination and microhardness indentation techniques, and (2) evaluate the retention of Opal Seal on tooth surfaces using black-light detection.
Material and methods
Before the study, ethical approval was obtained from the Research Office of Virginia Commonwealth University. Orthodontic patients (10-20 years old) who were scheduled to have at least 2 premolars extracted for orthodontic purposes were identified. The sample size was determined using the data for μ1, μ2, and σ from the study by Pascotto et al. A power analysis indicated that 10 patients per group would result in a 90% chance of obtaining significance at the 0.05 level. Because of possible dropouts, 22 patients (11 per group) were enrolled.
At baseline, oral hygiene status was determined using the plaque and bleeding indexes. The presence and absence of WSLs was also evaluated with the visual examination technique. Patients with good overall health and good oral hygiene (with no bleeding after 30 seconds and no plaque, or having a discontinuous band of plaque at the gingival margin) were selected. In addition, the first premolars had to be fully erupted and intact without visible defects on the buccal surfaces. The patients who met all inclusion criteria were enrolled, and informed consent was obtained. A split-mouth study design was used; in each patient, 1 premolar was randomly chosen as the experimental tooth, and the contralateral tooth was assigned as the control.
Before bonding, the tooth surfaces in both groups were cleaned with a rubber prophy cup and fluoride-free pumice, etched for 15 seconds with 37% phosphoric acid gel (3M Unitek), rinsed with water for 5 seconds, and dried with an oil-free air-water syringe. Opal Seal was applied to the experimental teeth according to the manufacturer’s instructions. The control teeth received a nonfluoride conventional orthodontic primer (Transbond XT moisture insensitive primer; 3M Unitek). To standardize the amount of adhesive used for bonding of each bracket, precoated premolar brackets were used (APC II Mini Twin Bicuspid; 3M Unitek). After positioning and firmly pressing the bracket on the enamel surface, the excess adhesive was removed with a periodontal probe. The adhesive was then light cured for 3 seconds from the mesial aspect and 3 seconds from the distal aspect using a plasma arc visible light-curing unit (Ortholite; 3M Unitek). All bonding procedures were carried out by the same clinician (D.R.P.). Subsequently, elastomeric spacers were placed around the bracket wings to encourage plaque accumulation so that the ideal environment for the development of WSLs could be provided. At subsequent orthodontic appointments, the accumulation of the plaque was visually confirmed on the teeth around the spacers. The patients were not told which tooth received the experimental orthodontic primer. All patients were instructed to brush twice a day with an over-the-counter fluoride-containing toothpaste. However, they were asked not to use any other fluoride-containing products including antibacterial or fluoride mouth rinse.
The patients were asked to have their teeth extracted approximately 12 weeks after the initial bracket placement and were given bottles containing 1% chloramine T solution for tooth storage. An extraction referral letter asking the dentist to leave the bracket on the tooth surface while performing the extractions, if possible, was also given.
Upon collection from the patients, the teeth were cleaned and placed into bottles filled with fresh 1% chloramine T solution for further disinfection until the visual examinations to evaluate the presence or absence of WSLs.
Visual examination was carried out independently by 2 clinicians (E.T., D.R.P.) who were blinded to the experimental protocol. These evaluators were previously trained and calibrated.
Each tooth was randomly removed from its storage bottle and air dried for 5 seconds, and the buccal surface was examined visually for enamel demineralization with the unaided eye in the portion of the crown gingival to the bracket using the following scale.
-
0, No visible white spots or surface disruption (no decalcification)
-
1, Visible white spot without surface disruption (mild decalcification)
-
2, Visible white spot with a roughened surface but not requiring restoration (moderate decalcification)
-
3, Visible WSL requiring restoration (severe decalcification)
If the bracket was inadvertently debonded during the extraction procedures, the area gingival to the middle third of the tooth surface was examined for demineralization.
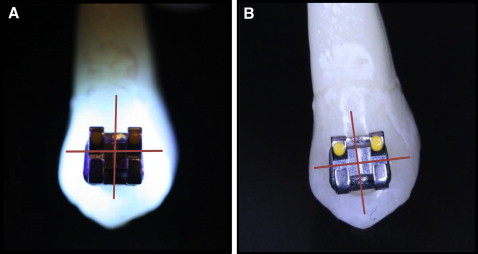
After the visual examination, the teeth were selected in a random order, air dried for 5 seconds, and examined under a hand-held black light. Since Opal Seal has a fluorescing agent in its composition, the tooth surfaces were examined to evaluate primer retention. The tooth surface was divided into mesiogingival, distogingival, mesioclusal, and distoclusal quadrants ( Fig 1 ). The amount of remaining primer was recorded as 100%, 75%, 50%, 25%, or 0%. A score of 100% was assigned if all 4 quadrants fluoresced under the black light, indicating full coverage, whereas a score of 0% indicated the complete absence of the material with no fluorescence in any of the 4 quadrants.
Previous studies have shown a strong correlation between the hardness values and the mineral content of the enamel. Therefore, cross-sectional microhardness testing, an accepted reproducible and reliable analytic method, was used to assess the mineral loss on the enamel surface.
The teeth were embedded in clear epoxy resin (Epoxicure; Buehler, Lake Bluff, Ill) and sectioned parallel to the long axis buccolingually through the brackets using a water-cooled diamond wafering blade on a low-speed rotary saw (Accutom-5; Struers, Westlake, Ohio). If brackets debonded during the sectioning process, these teeth were discarded because it would be difficult to determine distances gingival to the bracket without a reference point. Subsequently, the sections were serially polished through 4000 grit silicon carbide polishing paper.
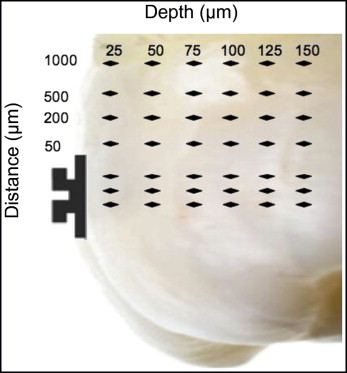
On each tooth, 42 indentations (Knoop hardness: Duramin-5; Struers) were made at distances of 0, 50, 200, 500, and 1000 μm from the bracket edge and at depths of 25, 50, 75, 100, 125, and 150 μm from the external surface of the enamel ( Fig 2 ). The average value of 3 indentations made in the isolated enamel directly beneath the bracket at the distance of 0 at the depths of 25, 50, 75, 100, 125, and 150 μm was used as the reference Knoop hardness number of the sound enamel at that specific depth. Therefore, the values obtained at 50, 200, 500, and 1000 μm from the bracket at 6 depths were compared with the baseline value (average Knoop hardness number value at distance, 0) to determine the changes in the mineral content of the tooth. Negative differences reflected Knoop hardness number values lower than the reference values.
Statistical analysis
A chi-square test was used to determine whether there were differences between the percentages of visible WSLs observed in the Opal Seal group compared with the Transbond XT group (control). A repeated-measures logistic regression was used to test for the effect of the study variables on the presence of WSLs. Enamel hardness was analyzed using a repeated-measures mixed-model analysis of covariance (ANCOVA) to evaluate the effect of materials, depths from the enamel surface, positions, and their interactions. We used SAS software (version 9.3; SAS Institute, Cary, NC) for all analyses, and the statistical significance was set at P <0.05.
Results
The patients were asked to have their teeth extracted at about 12 weeks (84 days) after the initial bracket-bonding appointment. However, because of a lack of compliance with the instructions, the average length of time that the teeth remained in the oral environment (days in vivo) was 67 ± 28 days.
A total of 72 teeth were evaluated for WSLs by 2 calibrated clinician examiners (E.T., D.R.P.). In 14 subjects, 4 teeth (4 premolar extraction patients with both maxillary and mandibular premolars), and in 8 subjects, 2 teeth (2 premolar extraction patients with either maxillary or mandibular premolars) were observed to have WSLs.
Overall, the results of the visual examination indicated that 46% of the control teeth vs 29% of the experimental teeth exhibited demineralization ( Table I ). The 2 raters agreed 86% of the time. The chance-corrected kappa coefficient was 0.71, indicating a high level of agreement. Statistical analyses indicated no significant difference in the incidence of WSLs between the experimental and control groups during the study ( P = 0.106).
| WSLs | P value | |||
|---|---|---|---|---|
| No | Yes | % yes | ||
| Pairs | 0.106 | |||
| Transbond XT | 39 | 33 | 46 | |
| Opal Seal | 51 | 21 | 29 | |
Opal Seal remained on an average of 50% of the tooth surfaces at 90 days. Regression analysis indicated no correlation between the percentage of Opal Seal remaining on the tooth surfaces and the number of days the teeth were in the mouth (r = −0.06; P >0.6).
The results of the repeated-measures mixed-model ANCOVA showed a statistically significant change in hardness difference across the 6 depths from the enamel surface in both groups ( Table II , Fig 3 ). The hardness values were low at the depths of 25 and 50 μm, and they increased as the depth increased for both the control and experimental groups ( P <0.001). When compared with the hardness values directly under the bracket (0-mm distance), a significant decrease in the hardness value was observed for the indentations at 50, 200, 500, and 1000 μm from the bracket base toward the cervical portion in both the experimental and control teeth ( P <0.001). There were no statistically significant differences overall between the 2 groups across the indentation locations ( P >0.8).
| Depth (μm) | Transbond XT control | Opal Seal experimental | ||
|---|---|---|---|---|
| Hardness | 95% CI | Hardness | 95% CI | |
| Distance = 0 μm | ||||
| 25 | 302.2 | 294.3-310.2 | 303.1 | 295.8-310.4 |
| 50 | 302.2 | 294.2-310.2 | 303.6 | 296.2-310.9 |
| 75 | 303.1 | 295.1-311.0 | 304.1 | 296.8-311.4 |
| 100 | 303.9 | 296.0-311.9 | 305.7 | 298.3-313.1 |
| 125 | 305.5 | 297.5-313.6 | 305.8 | 298.4-313.2 |
| 150 | 305.6 | 297.6-313.6 | 308.5 | 301.0-316.0 |
| Distance = 50 μm | ||||
| 25 | 287.1 | 274.1-300.2 | 276.9 | 264.9-288.9 |
| 50 | 284.6 | 271.5-297.6 | 283.1 | 271.1-295.1 |
| 75 | 298.9 | 285.9-312.0 | 299.1 | 287.1-311.1 |
| 100 | 301.5 | 288.5-314.6 | 295.7 | 283.7-307.7 |
| 125 | 293.0 | 280.0-306.1 | 299.3 | 287.2-311.3 |
| 150 | 302.6 | 289.5-315.6 | 304.3 | 292.2-316.4 |
| Distance = 200 μm | ||||
| 25 | 279.9 | 266.8-292.9 | 285.1 | 273.1-297.1 |
| 50 | 279.9 | 266.9-293.0 | 295.7 | 283.7-307.6 |
| 75 | 288.2 | 275.2-301.2 | 292.7 | 280.7-304.7 |
| 100 | 294.1 | 281.0-307.1 | 299.1 | 287.1-311.1 |
| 125 | 301.8 | 288.7-314.8 | 308.8 | 296.8-320.8 |
| 150 | 296.1 | 283.1-309.2 | 293.3 | 281.2-305.4 |
| Distance = 500 μm | ||||
| 25 | 282.0 | 269.0-295.1 | 274.1 | 262.1-286.1 |
| 50 | 299.4 | 286.4-312.4 | 281.9 | 269.9-293.9 |
| 75 | 293.6 | 280.6-306.6 | 299.5 | 287.5-311.5 |
| 100 | 305.5 | 292.5-318.6 | 299.8 | 287.8-311.8 |
| 125 | 302.8 | 289.7-315.8 | 309.7 | 297.7-321.7 |
| 150 | 304.4 | 291.4-317.5 | 303.5 | 291.4-315.6 |
| Distance = 1000 μm | ||||
| 25 | 284.6 | 271.6-297.6 | 284.7 | 272.7-296.7 |
| 50 | 287.4 | 274.4-300.5 | 288.0 | 276.0-299.9 |
| 75 | 301.0 | 288.0-314.1 | 296.6 | 284.6-308.6 |
| 100 | 303.5 | 290.5-316.6 | 302.8 | 290.8-314.8 |
| 125 | 302.8 | 289.7-315.8 | 308.8 | 296.7-320.8 |
| 150 | 304.7 | 291.6-317.7 | 298.1 | 286.0-310.2 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


