Introduction
White spot lesions are a common complication after orthodontic treatment. The aim of this systematic review was to investigate which remineralizing agents are effective for the treatment of white spot lesions after orthodontic treatment.
Methods
According to predetermined criteria, 4 databases were searched for appropriate studies. References of the selected articles and relevant reviews were searched for any missed publications.
Results
Seven randomized controlled trials were selected as eligible studies, and only qualitative analyses were performed because of the diversity of the interventions and outcome measures. Two studies showed significant effects of 2 different fluoride preparations: one with a small sample size and several methodologic deficiencies, and the other using only nonconventional detection methods (ie, DIAGNOdent pen, KaVo, Biberach, Germany) to assess white spot lesions. Two studies involved casein phosphopeptide-amorphous calcium phosphate, which seemed to be effective for the regression of white spot lesions. However, the statistical analysis in 1 study was based on the tooth surfaces instead of the patient, and the visual examination used in the other study to assess the white spots was not reliable.
Conclusions
Based on the literature, there is a lack of reliable evidence to support the effectiveness of remineralizing agents for the treatment of postorthodontic white spot lesions.
White spot lesions (WSLs) are defined as a “subsurface enamel porosity from carious demineralization” that presents as “a milky white opacity when located on smooth surfaces.” Since fixed orthodontic appliances were introduced, WSLs have become a particular clinical problem that can be attributed to the difficulties in performing oral hygiene procedures on bonded dental arches and the prolonged plaque accumulation on tooth surfaces. Despite many attempts at comprehensive prophylaxis, the prevalence of WSLs remains as high as 61% when debonding. It is generally believed that these lesions will recover through natural remineralization with saliva once the orthodontic appliances have been removed and oral hygiene is restored. However, the removal of stagnant plaque alone is not enough to achieve complete repair of WSLs, and some spots secondary to debonding can last from 5 to 12 years. Natural remineralization through saliva involving mineral gain in the surface layer of WSLs has little improvement on the esthetics and structural properties of the deeper lesions. Therefore, it is necessary to apply remineralizing agents to repair the deeper parts of WSLs for better esthetic results.
Although the treatment of postorthodontic WSLs differs from their prevention during orthodontic procedures, common interventions include fluoride and calcium phosphate-based remineralizing agents. Fluoride has been shown to arrest the development and progression of carious lesions during orthodontic treatment, but concentrated fluoride is not recommended for treatment of WSLs on the labial surfaces of teeth, since hypermineralization maintains the whiteness of the lesions. Casein phosphopeptide amorphous calcium phosphate is another agent that has garnered the most attention among the calcium phosphate-based technologies. It has been shown that casein phosphopeptides work by increasing the levels of calcium and phosphate ions in the subsurface lesions, and can be further enhanced by incorporating fluoride. Hence, this remineralizing system has the potential to achieve subsurface remineralization and to esthetically repair WSLs.
Compared with the evidence on the prevention of WSLs during orthodontic treatment, less is known regarding their treatment with remineralizing agents after orthodontic therapy. Presently, several randomized controlled clinical trials have shown the effects of remineralizing agents on postorthodontic WSLs; however, there have been no systematic evaluations of these results. Therefore, the purposes of this systematic review were to assess the direct evidence regarding the effect of remineralizing agents on postorthodontic WSLs and to evaluate which remineralizing agents are effective for the treatment of WSLs after orthodontic treatment.
Material and methods
The method for this review was according to Cochrane Oral Health Group’s Handbook for Systematic Reviews of Interventions ( http://ohg.cochrane.org ).
The inclusion criteria were (1) randomized controlled clinical trials regarding the application of remineralizing agents for the treatment of postorthodontic WSLs; (2) studies in which participants completed the fixed orthodontic treatment and had at least 1 clinically visible lesion on the labial enamel surface upon removal of the fixed orthodontic appliances; (3) studies in which interventions included remineralizing agents for the treatment of postorthodontic WSLs (ie, any fluoride or casein phosphopeptide-based system); (4) studies in which the control group consisted of patients subjected to different agents or not subjected to an intervention (either a placebo or no intervention); and (5) studies in which the primary outcome was the change in the severity of the lesions between the experimental and control groups, and the severity was expressed macroscopically in terms of the area over the whiteness of the lesion or microscopically by the amount of mineral loss or lesion depth.
The exclusion criterion was any study in which the participants underwent any nonremineralizing therapy (eg, bleaching, enamel microabrasion, or restoration) for WSLs after their orthodontic treatment.
For the identification of studies included in or considered for this review, the following databases were searched: PubMed (from 1966 to week 4 of July 2012), Ovid MEDLINE (from 1946 to week 4 of November 2011), Web of Science (from 1980 to week 4 of July 2012), and the Cochrane Library (to week 4 of July 2012). To locate additional studies, the references of the selected articles and relevant reviews were also checked. The search strategies included a combination of controlled vocabulary and free text terms (refer to the full strategy in Appendix I ). No limits were set on year, publication status, or language of the trials.
According to the predetermined inclusion and exclusion criteria, all titles and abstracts were examined by 1 reviewer (H.C.) to find relevant studies; the full texts of the relevant studies were scrutinized by 2 reviewers (H.C. and T.G.) independently to select eligible studies. Any disagreement was discussed, and the opinion of a third reviewer (Y.D.) was sought if necessary.
Data from all eligible studies were extracted by 2 reviewers (H.C. and T.G.) independently, in duplicate, using a specially designed data extraction form that was piloted in several articles and modified as required before use. Any disagreement was discussed, and a third reviewer (Y.D.) was consulted when necessary.
For each included study, descriptive and quantitative information was extracted, including citation author, year of publication, experimental treatment (number of subjects), control treatment (number of subjects), treatment duration, assessment method, results of baseline and follow-up visits, authors’ conclusions, and all information needed for quality evaluation criteria. Authors were contacted for clarification or missing information.
Each study’s methodologic quality was assessed by using the domain-based evaluation described in the Cochrane Handbook for Systematic Reviews of Interventions 5.0.2. Using the guidelines in the Cochrane Handbook, 2 reviewers (H.C. and X.L.) independently assessed the quality of the identified studies. If their opinions differed, the articles were referred to the third reviewer (Z.J.) for independent review and recomparison of the results. The consensus approach was used for any disagreement.
The reviewers categorized the following 6 quality items as “yes” (low risk of bias), “unclear” (uncertain risk of bias), or “no” (high risk of bias): sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias. The level of risk for each study was then classified as low (all quality items were met), medium (1 or 2 quality items were not met), or high (3 or more quality items were not met).
Statistical analysis
For studies with continuous outcomes that used patient units for statistical comparison, mean differences between the experimental and control groups and 95% confidence intervals (CIs) were used to summarize the data. For a study that used the tooth surface unit for statistical analysis, we could not calculate the mean differences and 95% CIs because the patient unit data could not be obtained. The clinical methodologies of all studies were assessed by examining the types of interventions and outcomes. A meta-analysis was planned to combine the data of studies with sufficient similarities in their methodologies.
Results
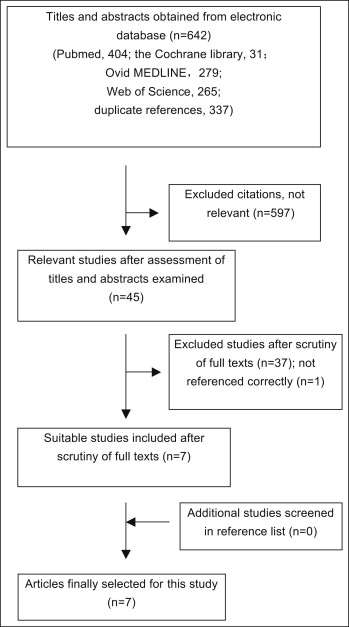
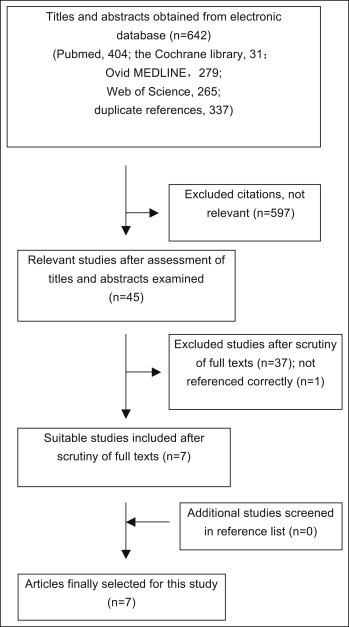
The electronic and hand searches retrieved 642 unique citations, which were entered into a flow chart ( Fig 1 ) to illustrate the path for selecting the final trials. After evaluating titles and abstracts, we obtained 45 relevant studies (1 study could not be located). After evaluating the full texts, we selected 7 studies as eligible ; 37 articles were excluded from the study. A list of the excluded articles and the reasons for exclusion is in Appendix II . After searching the references of the selected articles and relevant reviews, we identified no additional eligible studies. Finally, 7 studies, all in English, were used for the systematic review, and a description of each is given in Table I .
| Authors | Participants, test/control | Follow-up | Test vs control | Assessment method | Start, test/control (SD) | End, test/control (SD) |
|---|---|---|---|---|---|---|
| Willmot | 15/11 | Debond, 12 w, 26 w | 50 ppm NaF rinse ∗ vs control rinse ∗ | Photographs | Difference of 0-26 w: ADPR 54.3% (12.3)/66.1% (15.5) | |
| Du et al | 55/55 | Debond, 3 m, 6 m | 5% NaF varnish vs saline solution | DIAGNOdent | DR 17.66 (5.36)/16.19 (5.70) | DR 10.10 (4.86)/13.10 (5.19) |
| Baeshen et al | 19/18 Sites 152/140 |
Deband, 2 w, 4 w, 6 w | 0.5% NaF Miswaks † vs control Miswaks † | DIAGNOdent, clinical scores | DR 13.2 (5.6)/11.5 (6.1) Clinical scores 2.4 (0.8)/2.0 (0.9) |
DR 4.5 (2.9)/9.4 (5.3) Clinical scores 1.0 (0.8)/1.7 (1.0) |
| Andersson et al | 13/13 Sites 70/62 |
Debond, 1 m, 3 m, 6 m, 12 m | CPP-ACP (Topacal) vs fluoride rinse † | DIAGNOdent, clinical scores | DR 7.4 (10.2)/9.4 (9.5) | DR 4.4 (5.2)/6.4 (7.5) Difference of 0-12 m: PCS (score 0, 1): 64%/23% |
| Bröchner et al | 30/30 | Deband, 4 w | CPP-ACP (tooth mousse) vs fluoride toothpaste | Clinical scores, QLF | PCS (score 1) 15.4%/14.9% ΔF 6.68 (0.58)/7.04 (1.65) A 0.12 (0.16)/0.19 (0.43) |
PCS (score 1) 47.7%/52.7% ΔF4.45 (1.82)/4.51 (2.46) A 0.05 (0.09)/0.14 (0.31) |
| Bailey et al | 23/22 Sites 207/201 |
Deband 4 w, 8 w, 12 w | CPP-ACP (tooth mousse) † vs control cream † | Clinical scores | Difference of 0-12 w: PCS (score 0, 1): 8.6%/8.5% PWT (score 2, 3): 76.8%/58.6% | |
| Beerens et al | 35/30 | Debond, 6 w, 12 w | CPP-ACFP (MI-Paste) † vs control paste † | QLF | ΔF 8.45 (1.17)/9.10 (1.75) A 5.07 (5.69)/7.29 (7.91) |
ΔF 7.52 (1.78)/7.96 (2.76) A 5.05 (6.98)/7.17 (7.76) |
Among the 7 included studies, 3 randomized controlled trials evaluated the effects of 3 fluoride preparations: 50-ppm sodium fluoride mouth rinse, 5% sodium fluoride varnish, and 0.5% sodium fluoride chewing sticks. The remaining 4 studies compared the effects of remineralizing agents containing casein phosphopeptide amorphous calcium phosphate or casein phosphopeptide amorphous calcium fluoride phosphate; 2 studies had an inactive control, and 2 used a fluoride control. No significant similarities in methodologies could be found in these studies. Casein phosphopeptide amorphous calcium phosphate was included in 3 studies, with varying criteria for the visual examination. Two studies used quantitative light-induced fluorescence, but with different interventions (one with casein phosphopeptide amorphous calcium phosphate alone, and the other with a combination of casein phosphopeptide amorphous calcium phosphate and fluoride). Based on the circumstances, it was not feasible to create a pool of data to perform a meta-analysis. Thus, a qualitative analysis was undertaken.
All studies had methodologic problems after examination and contact with the authors ( Table II ). Whether the randomization had been blinded was not reported in 4 studies, and the blinding procedure was unclear in 2 studies. Whether the operator and the evaluator were separate persons was unclear in 2 studies. Two studies did not report the data based on patients, and 1 study did not report a prespecified primary outcome measured by quantitative light-induced fluorescence. Statistical analyses of 2 studies were based on the number of teeth, and the assessment methods of 2 studies were only through technology-based methods (DIAGNOdent pen [KaVo, Biberach, Germany] or quantitative light-induced fluorescence).
| Author | Adequate sequence generation | Allocation concealment | Blinding of outcome assessors | Incomplete outcome data addressed | Selective outcome reporting | Free of other bias | Level of risk for bias |
|---|---|---|---|---|---|---|---|
| Willmot | Yes | Yes | Yes | No | Yes | No | Medium |
| Du et al | Yes | No | Yes | No | Yes | No | High |
| Baeshen et al | Yes | No | Unclear | Yes | Yes | No | High |
| Andersson et al | Yes | No | Unclear | No | No | No | High |
| Bröchner et al | Yes | No | Yes | No | No | No | High |
| Bailey et al | Yes | Unclear | Yes | Yes | No | No | High |
| Beerens et al | Yes | Unclear | Yes | No | Yes | No | High |
The included studies were grouped into 3 comparisons according to the strategy of the interventions.
One study assessed the effect of 50 ppm of fluoride for the treatment of WSLs by using computerized image analysis to measure the lesion sizes. In a 26-week follow-up, the value of the average difference in the percentage of reduction of lesion size was not significantly decreased in the test group compared with the control group (mean difference, −0.12; 95% CI, −0.25, 0.01). Another study tested the efficacy of fluoride varnish (5% sodium fluoride) assessed with laser fluorescence (DIAGNOdent), and indicated that the DIAGNOdent readings were significantly different between the fluoride-treated group and the control group (mean difference, −4.47; 95% CI, −6.59, −2.35). The third study compared 0.5% sodium fluoride chewing sticks with nonfluoridated chewing sticks by using visual inspection (International Caries Detection and Assessment System II index criteria) and DIAGNOdent. At the end of treatment, both the DIAGNOdent readings and the International Caries Detection and Assessment System II index were significantly decreased in the intervention group compared with the control group (mean difference, 6.60; 95% CI, 4.68, 8.52; mean difference, 1.10; 95% CI, 0.77, 1.43; respectively).
One study was performed by visual scoring (0-4) and laser fluorescence (DIAGNOdent). After 12 months, the laser fluorescence readings were not significantly decreased in the casein phosphopeptide amorphous calcium phosphate group (mean, 4.4; SD, 5.2) compared with the fluoride group (mean, 6.4; SD, 7.5). The proportion of the visual scoring of 0 (no white spots) to 1 (slight white spot only visible after air drying) was significantly increased in the casein phosphopeptide amorphous calcium phosphate group compared with the fluoride group (64% vs 23%). Another study was carried out through visual inspection (Gorelick criteria) of digital photographs and quantitative light-induced fluorescence for 4 weeks. At the end of treatment, there were no significant differences in fluorescence loss (mean difference, −0.02; 95% CI, −0.17, 0.13) and lesion areas (mean difference, 0.3; 95% CI, −0.75, 1.35) between the groups. The proportions of WSLs with a score of 1 were 47.7% in the intervention group and 52.7% in the control group; this was not a significant difference.
One study used the International Caries Detection and Assessment System II index criteria to compare the effect of casein phosphopeptide amorphous calcium phosphate cream with a placebo cream for 12 weeks. The results showed that, compared with baseline scores, the proportion of the visual scoring of 0 or 1 did not increase to a greater extent in the casein phosphopeptide amorphous calcium phosphate group compared with the control group (8.6% vs 8.5%). With regard to the lesions with visual scores of 2 (white spot visible when wet) and 3 (loss of enamel surface integrity), the significant regression of the proportion of WSLs with a score of 2 or 3 to 0 after 12 weeks was detected in the casein phosphopeptide amorphous calcium phosphate group compared with the placebo group (76.8% vs 58.6%). Another study used quantitative light-induced fluorescence to compare casein phosphopeptide amorphous calcium fluoride phosphate paste with a control paste for a 3-month intervention period. No statistically significant differences between the groups were observed with regard to the sizes of the lesion areas (mean difference, 0.10; 95% CI, −3.72, 3.92) or the fluorescence loss (mean difference, 0.21; 95% CI, −0.88, 1.30).
Results
The electronic and hand searches retrieved 642 unique citations, which were entered into a flow chart ( Fig 1 ) to illustrate the path for selecting the final trials. After evaluating titles and abstracts, we obtained 45 relevant studies (1 study could not be located). After evaluating the full texts, we selected 7 studies as eligible ; 37 articles were excluded from the study. A list of the excluded articles and the reasons for exclusion is in Appendix II . After searching the references of the selected articles and relevant reviews, we identified no additional eligible studies. Finally, 7 studies, all in English, were used for the systematic review, and a description of each is given in Table I .