Introduction
The postretention stability of open-bite treatment is a controversial topic in orthodontics.
Methods
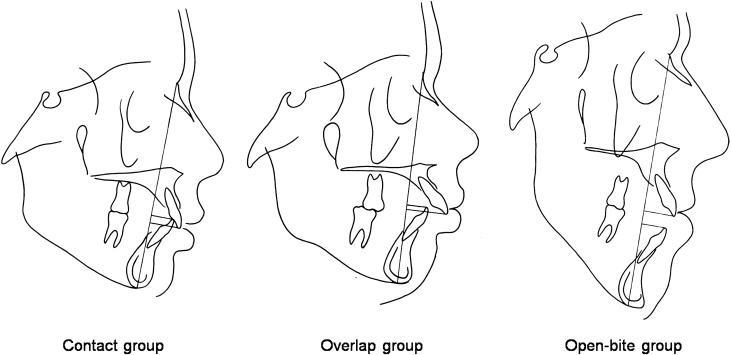
In this study, the lateral cephalometric radiographs of 64 patients treated with orthodontics alone were evaluated to determine the amount of postretention change. The mean postretention interval was 14 years. The sample was divided into 3 groups based on the amounts of pretreatment overbite: (1) the contact group (n = 24), incisal overlap and incisal contact; (2) the overlap group (n = 25), incisal overlap and no incisal contact; and (3) the open-bite group (n = 15), no incisal overlap. The headfilms were digitized, and the values were analyzed.
Results
The 3 groups reacted differently. During the postretention period, mean overbite deepened in all groups, with the contact group deepening significantly more than the open-bite group. Overjet increased significantly more in the open-bite group than in the contact group. Pretreatment overjet correlated mildly with postretention overjet relapse in the open-bite group.
Conclusions
All 64 subjects had positive incisal overlap at the postretention recall.
Editor’s summary
The next time you see a new patient with a malocclusion characterized by anterior open bite, I predict you will be hesitant to promise long-term closure of the open bite, even if the patient agrees to follow through with any treatment approach you recommend. Why is this? Have you been stung once too often, or is it that you have not seen many good studies to prove the contrary?
The purposes of this study from the University of Washington were to (1) assess the long-term stability of anterior open bite treated orthodontically, (2) review skeletal changes, (3) compare postretention changes in patients with differing amounts of vertical incisor overlap before treatment, and (4) search for correlations between preretention and postretention cephalometric changes.
To establish a basis for comparison, 64 subjects were divided into 3 groups based on the original overbite or incisal contact: contact group (n = 24), overlap group (n = 25), and open-bite group (n = 15). All patients were treated with conventional edgewise appliances, and most vertical problems were treated with high-pull extraoral traction as needed. Final records were taken from 9.5 to 33.0 years postretention.
Following treatment over this lengthy period of time showed vertical relapse in only 1 of the 24 contact subjects, but in 7 of the 25 overlap subjects and 3 of the 15 open-bite subjects. “However,” noted the authors, “even though some subjects displayed decreased overbite from T2 to T3, none had a negative incisal overlap at T3.”
To be more specific, (1) 4% of the contact group relapsed from contact to overlap status, (2) 20% of the overlap group relapsed from contact to overlap status, and (3) 40% of the open-bite group relapsed from contact to overlap status.
Although no subjects in the open-bite group showed negative overbite at T3, the group had considerable relapse when incisal contact was the criterion used. So what do you tell your next open-bite patient to expect after treatment? Based on what we know at this time, it is not possible to predict whether treatment results will be stable or unstable. However, it is likely that the patient will have a positive overbite at his or her postretention recall. Just remember that 60% of the open-bite group lacked incisal contact.