Orthodontic treatment is planned on an individual, case-by-case basis after thoroughly considering the patient’s overall facial and dental characteristics, the expected duration of treatment, costs, patient preferences, and the orthodontist’s experience. This article reports the treatment of a patient with a maxillary premolar-molar transposition in the permanent dentition that was successfully managed with orthodontic treatment. A girl, aged 10 years 2 months, came for treatment with an ectopic maxillary left premolar. Radiographic analysis indicated a developing complete transposition of the maxillary left premolar. The patient was treated with extraction of the deciduous molar and surgical exposure and ligation of the premolar. Eruption was properly guided, and the correct order of the 2 teeth was restored in the arch. This challenging treatment approach is described in detail, including the mechanics used to align the ectopic premolar. Early treatment can, in many cases, prevent a molar-premolar transposition.
Tooth transposition is defined as a type of ectopic eruption with a permanent tooth developing and erupting in the position normally occupied by another permanent tooth. A distinction is made between complete transposition (where the crown and entire root of the involved teeth exchange places in the dental arch and are fully parallel) and incomplete transposition (where the crowns are transposed, although the root apices remain in their relatively normal positions).
The etiology of tooth transposition has been the subject of much controversy and is still not completely understood. Several theories have been proposed to explain the phenomenon. Multifactorial genetic factors, such as an interchange in the position of the developing dental laminae of the involved teeth, have been suggested as a cause for the transposition of teeth. Environmental factors such as deciduous tooth trauma or even retained deciduous teeth might also contribute, and familial occurrence has been observed.
When transposition occurs, the involved teeth show a characteristic malposition and appearance. Moreover, other congenital dental anomalies such as hypodontia, peg-shaped or small maxillary lateral incisors, retained deciduous teeth, severe rotations, malpositions, dilacerations, or malformations of the adjacent teeth are often observed. Unilateral transposition has been reported more often than bilateral transposition, with the left side somewhat more frequently involved than the right. Transpositions can, according to some authors, affect both sexes equally, whereas others report that transpositions are more frequent in female patients or male patients.
Although transpositions can appear in both the maxilla and the mandible, the maxillary canine is the most frequently involved tooth, followed by the first premolar, and less often by the lateral incisor. Transposition of teeth without involvement of the maxillary canine is extremely rare.
In this article, we describe a particular clinical situation where an ectopic premolar was diagnosed early and treated. This probably prevented a complete maxillary left premolar-molar transposition, and the involved teeth were repositioned to their normal anatomic positions in the dental arch.
Diagnosis and etiology
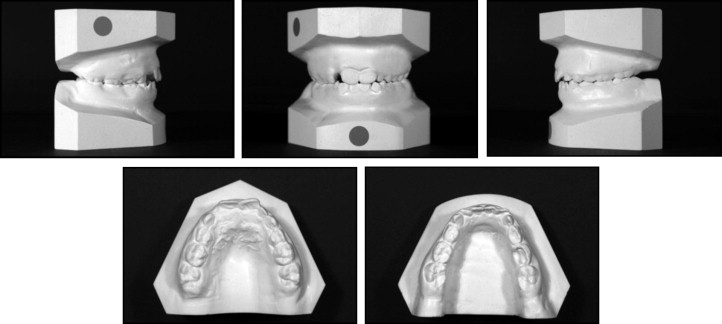
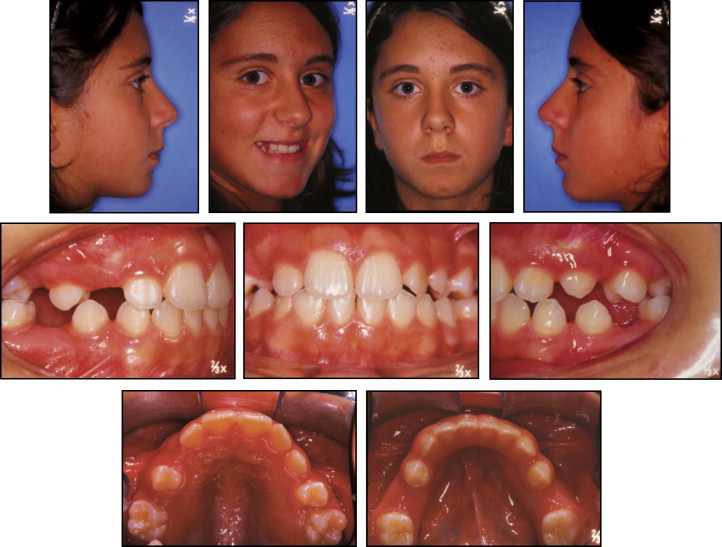
The physical examination of a 10-year-old girl showed a Class I dental relationship in the early mixed dentition: the maxillary arch was slightly constricted with no crossbite. Only maxillary central incisors were present, with no space for the unerupted lateral incisors, whereas all mandibular incisors were erupted. Mild crowding in both arches and a tendency to open bite were observed with a tongue thrust ( Figs 1 and 2 ).

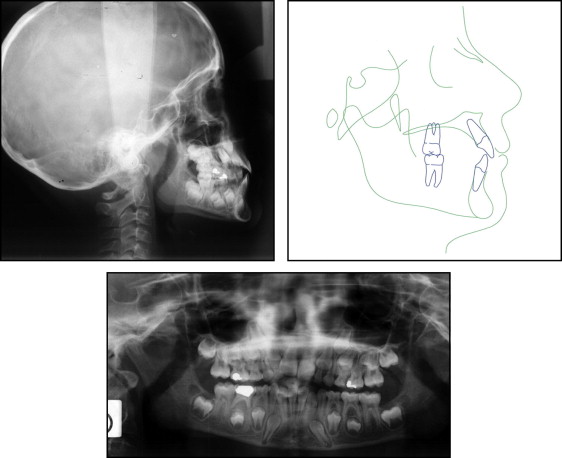
The lateral cephalometric evaluation showed a Class I skeletal malocclusion (ANB, 3°), vertical facial pattern (SnGoGn, 37°), retroclined maxillary incisors (1/SN, 99°), and proclined mandibular incisors (IMPA, 98°). The facial profile was slightly convex. The panoramic radiograph showed a developing ectopic premolar ( Fig 3 ). The erupting maxillary left permanent premolar was observed between the roots of the first molars. Moreover, all developing permanent teeth, except the mandibular third molars, were present.
The patient’s medical and dental histories were unremarkable, with no trauma to the deciduous teeth, and no familial occurrences were reported.
Treatment alternatives
We considered the following treatment alternatives.
- 1.
Extract the ectopic maxillary premolar and restore it with a fixed prosthesis or an implant.
- 2.
Extract the ectopic maxillary premolar and close the space with mesial movement of the first molar, which would then be carried into a Class II relationship.
- 3.
Extract the ectopic maxillary premolar along with the other 3 premolars, as the tendency to open bite, the vertical facial pattern, and the convex vertical profile might suggest. However, the arch-length discrepancy required no tooth extractions, nor did the facial profile.
- 4.
Surgically expose the ectopic maxillary premolar to move it into the proper position.
Treatment alternatives for the ectopic maxillary premolar could not include the traditional options to align the involved teeth in their transposed position, because this alternative was not favorable for masticatory function.
Treatment progress
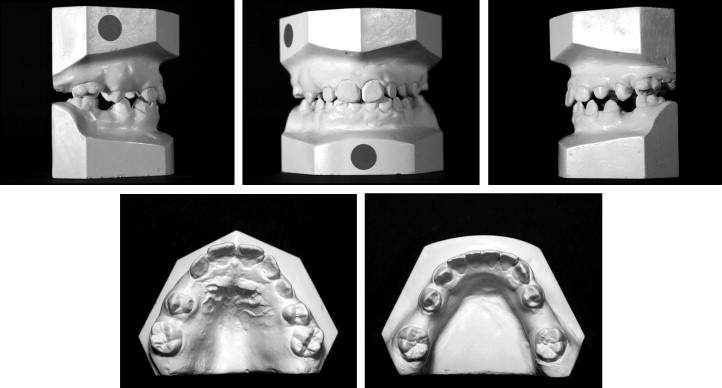
The first option seemed to be the easiest and more rational choice. The treatment started with an interceptive first phase, including a transpalatal bar in the maxillary arch and a lip bumper in the mandibular arch. After 2 years of treatment, the crowding was resolved, and the molars were derotated; consequently, the shapes of both arches were changed ( Figs 4 and 5 ). The panoramic radiograph showed the recovery of the space for erupting teeth in the mandibular arch. However, in the maxillary arch, space was still needed for eruption of the right canine and both second premolars. The panoramic radiograph confirmed an ectopic maxillary left permanent premolar located between the maxillary first and second molars with the root parallel to the roots of the second molar ( Fig 6 ).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


