This case report describes the treatment of a 25-year-old woman with a skeletal Class I pattern and moderate bimaxillary dentoalveolar protrusion. The orthodontic treatment included distal movement of her maxillary and mandibular dentitions using 1-stage miniscrews. The total active treatment time was about 12 months. Her tooth alignment and profile were significantly improved by the orthodontic treatment. The 2-year posttreatment records show a stable occlusion and satisfactory facial esthetics.
Highlights
- ●
Distalization of the maxillary and mandibular dentitions was achieved.
- ●
Distal movement of the second molars was more than 3 mm.
- ●
The patient’s tooth alignment and profile were significantly improved.
Bimaxillary protrusion is characterized by proclined anterior teeth, protrusive lips, and a convex lower facial profile. It can occur in almost every ethnic group, although it is more prevalent in African American and Asian populations. Most patients with bimaxillary protrusion seek orthodontic or orthopedic treatment to decrease the protrusion and improve their facial profile and, consequently, facial esthetics.
The treatment of bimaxillary protrusion does not present many challenges, and the condition can be satisfactorily corrected by orthodontic or surgical treatment or a combination of both. Orthodontic treatment involves retraction of the anterior teeth with maximum anchorage, typically after extraction of the first premolars if required, thus correcting a dentoalveolar protrusion. Surgical treatment, on the other hand, involves repositioning of segments of the jaws in conjunction with orthodontic treatment, thus correcting a skeletal protrusion. Currently, anterior segmental osteotomy has become a popular procedure because it decreases the total treatment duration in adults who require orthodontic treatment.
All above-mentioned methods for decreasing the proclination associated with bimaxillary protrusion require extraction of the maxillary or mandibular first premolars. Some patients do not want extraction of healthy teeth for various reasons; however, they are also concerned about proclined anterior teeth and protruding lips. Consequently, the improvement of facial esthetics in these patients becomes a challenge.
In 2013, Ishida et al reported on a patient with an Angle Class II malocclusion corrected by asymmetric distalization of the maxillary molars using zygomatic arch anchorage, which, in fact, distalized the entire dentition. Furthermore, Tai et al reported on a patient with a Class III malocclusion corrected by distalization of the mandibular dentition using temporary skeletal anchorage devices. Generally, bimaxillary protrusion is characterized by a Class I malocclusion with protrusion of both the maxillary and mandibular dentitions. However, it remains debatable whether distalization of both dentitions for the correction of bimaxillary protrusion is a feasible alternative to premolar extraction.
Here, we report on a 25-year-old woman with a Class I skeletal pattern and moderate bimaxillary protrusion that was successfully corrected by the distalization of both dentitions with 1-stage miniscrews for anchorage.
Diagnosis and etiology
A 25-year-old woman with a convex lower facial profile came with a chief complaint of protruded maxillary front teeth. She required her treatment to be completed within a year because she was due to go abroad for further studies then. Furthermore, she was against extraction of any healthy teeth other than the third molars. Her medical and dental histories were unremarkable, with no previous maxillofacial or dental trauma or symptoms typically associated with the temporomandibular joint.
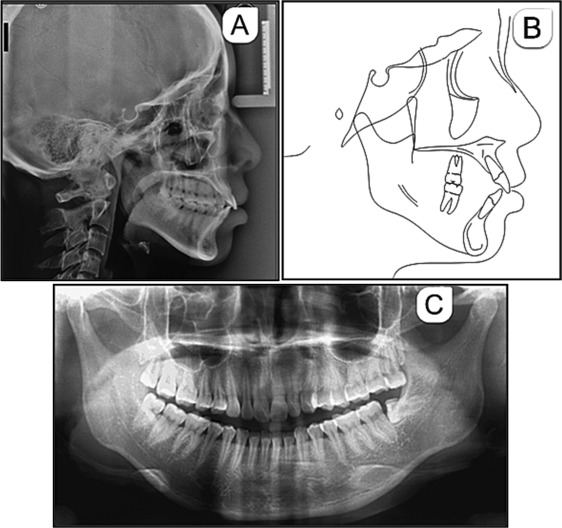
Her pretreatment facial photographs showed a near-normal nasolabial angle with a protruded lower lip. The chin was on the facial midline, and her face was generally symmetric. Intraorally, her molar and canine relationships were considered Class I, with a 5-mm overjet and a normal overbite. There was mild spacing in the maxillary anterior region and mild crowding in the mandibular anterior region, with a moderate curve of Spee on both sides. The dental midlines were aligned with the facial midline. All third molars were present, and the mandibular left third molar was horizontally impacted ( Figs 1 and 2 ).

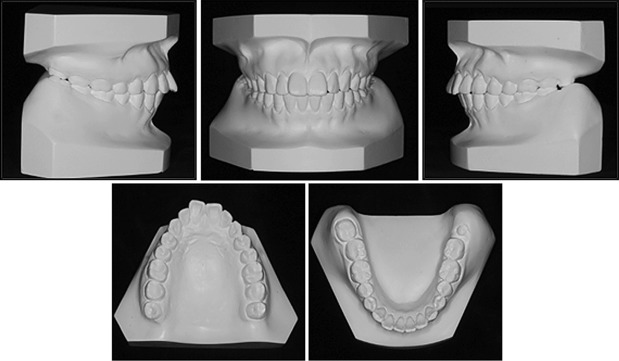
A lateral cephalogram and an orthopantomogram were obtained ( Fig 3 ). Figure 3 , C , shows the absence of caries, with pulp calcification in the maxillary left central incisor identified from the absence of a visible pulp canal. Her mandibular left third molar showed mesioangular impaction. The lateral cephalometric analysis (including a tracing) indicated a Class I skeletal pattern (ANB, 2.3°; Wits appraisal, 0.2 mm) with a steep mandibular plane angle (SN-MP, 43.5°). The maxillary and mandibular incisors were proclined (U1-PP, 119.4°; IMPA, 99.1°), and the interincisal angle (143.0°) was increased ( Table I ). A diagnosis of bimaxillary dentoalveolar protrusion was made.
| Parameter | Standard | Pretreatment | Posttreatment |
|---|---|---|---|
| SNA (°) | 82.8 ± 4.0 | 73.7 | 74.5 |
| SNB (°) | 80.1 ± 3.9 | 71.4 | 71.1 |
| ANB (°) | 2.7 ± 2.0 | 2.3 | 3.4 |
| A-NFH (mm) | 0.0 ± 3.7 | −9.5 | −5.4 |
| Wits (mm) | −1.1 ± 2.9 | 0.2 | 0.6 |
| MP2/SN (°) | 32.5 ± 5.2 | 43.5 | 43.6 |
| U1-AP (mm) | 7.2 ± 2.2 | 10.2 | 3.5 |
| L1-AP (mm) | 4.9 ± 2.1 | 6.6 | 1.5 |
| U1/PP (°) | 115.8 ± 5.7 | 119.4 | 97.7 |
| L1/MP (°) | 93.9 ± 6.2 | 99.1 | 90.5 |
| Interincisal angle (°) | 130.0 ± 7.6 | 112.1 | 143.0 |
Treatment objectives
The treatment objectives for this patient were as follows: (1) distalization of the proclined maxillary anterior teeth, her chief complaint; (2) correction of the mandibular and maxillary anterior crowding and spacing, respectively; (3) creation of an ideal overbite and overjet; and (4) improvement of her facial profile and, consequently, esthetics.
Treatment objectives
The treatment objectives for this patient were as follows: (1) distalization of the proclined maxillary anterior teeth, her chief complaint; (2) correction of the mandibular and maxillary anterior crowding and spacing, respectively; (3) creation of an ideal overbite and overjet; and (4) improvement of her facial profile and, consequently, esthetics.
Treatment alternatives
To correct the moderate anterior proclination, extraction of the 4 second premolars would have been ideal for this patient. However, this course of treatment would require over 2 years; in addition, the patient had refused extraction of healthy teeth other than the third molars. Therefore, we decided to use miniscrew anchorage for distalization of the maxillary and mandibular dentitions to correct the dentoalveolar protrusion.
Treatment progress
The patient was referred to a periodontist to rule out periodontal problems and an oral and maxillofacial surgeon for the third molar extractions. Preadjusted appliances with 0.022 × 0.028-in slots were bonded to her teeth in both arches for leveling and alignment; 0.014-in and 0.016-in nickel-titanium archwires were used for leveling in the maxillary and mandibular arches, respectively.
Once leveling was complete, 4 miniscrews (Ci Bei, Zhejiang, China) were implanted between the second premolars and the first molars in both arches. The integrity of the interradicular bone in this region in all 4 quadrants was checked on an orthopantomogram before miniscrew implantation. All miniscrews were implanted close to the root of the first molar to provide enough space for distalization of the second premolar. Cone-beam computed tomography was performed to check the position of the miniscrews ( Fig 4 ). The miniscrews were left unloaded for a week to allow soft tissue healing; then 0.019 × 0.025-in stainless steel archwires were used for distalization of both dentitions. Elastics were applied from the neck of the miniscrews to the crimpable hooks between the lateral incisors and the canines for distalization of the maxillary dentition ( Fig 5 ). The initial force of the tie-backs was between 1.5 and 2.5 N, and the interval between visits was 4 weeks. The distalization process lasted for approximately 8 months.




