Bioceramics have been adopted in dental restorations for implants, bridges, inlays, onlays, and all-ceramic crowns. Dental bioceramics include glass ceramics, reinforced porcelains, zirconias, aluminas, fiber-reinforced ceramic composites, and multilayered ceramic structures. The process of additive manufacturing is ideally suited to dentistry. Models are designed using data from a computed tomography scan or magnetic resonance imaging. Since its development in 2001, direct ceramic machining of presintered yttria tetragonal zirconia polycrystal has become increasingly popular in dentistry. There are wide variety commercially available cements for luting all-ceramic restorations. However, resin cements have lower solubility and better aesthetic characteristics.
Key points
- •
Bioceramics have rapidly been adopted in dental restorations for implants, bridges, inlays, onlays, and all-ceramic crowns. The structure of dental bioceramics covers a wide spectrum of glass ceramics, reinforced porcelains, zirconias, aluminas, fiber-reinforced ceramic composites, and multilayered ceramic structures.
- •
The process of additive manufacturing is ideally suited to dentistry. Models are designed using data from a computed tomography scan or magnetic resonance imaging. The image is downloaded to a computer-aided design (CAD) machine and converted to a standard transformation language (STL) file.
- •
Since its development in 2001, direct ceramic machining of presintered 3 mol% yttria stabilized tetragonal zirconia ceramics has become increasingly popular in dentistry. The die or wax pattern is scanned, an enlarged restoration is designed by computer software (CAD), and a presintered ceramic blank is milled by computer-aided machining.
- •
There are wide variety commercially available cements for luting all-ceramic restorations, including zinc phosphate cements, conventional and resin-modified glass ionomer cements, resin cements, and self-adhesive resin cements. However, resin cements possess some advantages compared with the other classes of materials, because they have lower solubility and better aesthetic characteristics.
History of dental materials
Gold was one of the first dental materials known; its use has been traced to circa 500 bc. Its durability and lack of corrosion make it one of the best restorative materials available.
The first dental porcelain, which was used for making complete dentures and individual teeth, was introduced at the end of 1700s. One of the major benefits of ceramic as a dental restorative material was the resemblance to natural dentition.
Since the nineteenth century, other dental materials like high-copper amalgam, polymers including composite resins, elastic impression materials, base metal alloys, orthodontic wires, bonding agents, glass ionomer, and polycarboxylate cements were also developed, which enhanced treatment possibilities. Every year new versions of dental materials with better properties are developed and introduced to practitioners. Among them are all-ceramic restorations, better quality composite resin and bonding agents, flowable composites and sealants, resin-modified glass ionomers and resin cements, and more accurate impression materials.
The science of dental materials studies the composition and properties of materials and the way they interact with the environment. The selection of materials for any application can thus be undertaken with confidence and sound judgment. Dentists spend much of their professional careers handling materials. The success or failures of many treatments depend on the correct selection of materials and their manipulation. Dental biomaterials are the natural tissues or synthetic products that are used to restore or replace decayed, damaged, fractured, or missing teeth. The major synthetic dental material groups are metals, ceramics, and polymers, including composite structures ( Table 1 ).
| Metals | Alloys | Components of dentures, orthodontic wires, cast restorations |
| Ceramics | Crystalline ceramics | Al 2 O 3 , SiO 2 |
| Glasses | Dental porcelain | |
| Inorganic salts | Gypsum product, dental cements | |
| Polymers | Rigid | Denture bases, direct filling |
| Elastomers | Impression materials |
History of dental materials
Gold was one of the first dental materials known; its use has been traced to circa 500 bc. Its durability and lack of corrosion make it one of the best restorative materials available.
The first dental porcelain, which was used for making complete dentures and individual teeth, was introduced at the end of 1700s. One of the major benefits of ceramic as a dental restorative material was the resemblance to natural dentition.
Since the nineteenth century, other dental materials like high-copper amalgam, polymers including composite resins, elastic impression materials, base metal alloys, orthodontic wires, bonding agents, glass ionomer, and polycarboxylate cements were also developed, which enhanced treatment possibilities. Every year new versions of dental materials with better properties are developed and introduced to practitioners. Among them are all-ceramic restorations, better quality composite resin and bonding agents, flowable composites and sealants, resin-modified glass ionomers and resin cements, and more accurate impression materials.
The science of dental materials studies the composition and properties of materials and the way they interact with the environment. The selection of materials for any application can thus be undertaken with confidence and sound judgment. Dentists spend much of their professional careers handling materials. The success or failures of many treatments depend on the correct selection of materials and their manipulation. Dental biomaterials are the natural tissues or synthetic products that are used to restore or replace decayed, damaged, fractured, or missing teeth. The major synthetic dental material groups are metals, ceramics, and polymers, including composite structures ( Table 1 ).
| Metals | Alloys | Components of dentures, orthodontic wires, cast restorations |
| Ceramics | Crystalline ceramics | Al 2 O 3 , SiO 2 |
| Glasses | Dental porcelain | |
| Inorganic salts | Gypsum product, dental cements | |
| Polymers | Rigid | Denture bases, direct filling |
| Elastomers | Impression materials |
Ceramics
Teeth are complex organs of the human body and consist of several component tissues, both hard and soft. The tooth is subject to many damaging influences. Restorative dentistry is concerned with repairing damaged teeth and their supporting structures. Aesthetics are of paramount concern, and the only medical material that in any way provides a durable and satisfactory solution to the aesthetic repair of teeth is ceramic.
Historic Perspectives: Ceramics as Restorative Materials
Although routine use of ceramics in restorative dentistry is a recent phenomenon, the desire for a durable and aesthetic material is ancient. Most cultures through the centuries have acknowledged teeth as an integral facial structure for health, youth, beauty, and dignity. Teeth have routinely been designated with an equally powerful, if occasionally perverse, role in cultures in which dentitions were purposely mutilated as inspired by vanity, fashion, and mystical and religious beliefs. Therefore, it has been almost universal that unexpected loss of tooth structure, and particularly missing anterior teeth, creates physical and functional problems and often psychological and social disturbances as well. During the eighteenth century, artificial teeth were made of human teeth, animal teeth carved to the size and shape of human teeth, ivory, bone, or mineral (porcelain). John Greenwood carved teeth from hippopotamus ivory for at least one of the 4 sets of complete dentures he fabricated for George Washington.
Mineral teeth or porcelain dentures accelerated an end to the practice of transplanting freshly extracted human teeth and supplanted the use of animal products. Feldspathic dental porcelains were adapted from European triaxial white ware formulations (clay-quartz-feldspar), nearly coincident with their development. After decades of effort, Europeans mastered the manufacture of fine translucent porcelains, comparable with porcelains of the Chinese, by the 1720s. The use of feldspar to replace lime (calcium oxide) as a flux, and high firing temperatures, were critical developments in fine European porcelain. Around 1774, the first successful porcelain dentures were made at the Guerhard porcelain factory by Nicholas Dubois de Chemant.
In 1808, Giuseppangelo Fonzi formed individual porcelain teeth that contained embedded platinum pins, which provided a major advance in prosthetic dentistry. In 1723, Pierre Fauchard described the enameling of metal denture bases. Fauchard was credited with recognizing the potential of porcelain enamels and initiating research with porcelains to imitate color of teeth and gingival tissues.
Classification of Dental Ceramics
Ceramics are classified into 3 main composition categories:
- •
Predominantly glass, which has a regular pattern of atoms known as an amorphous structure. They are the best at mimicking the optical properties of enamel and dentin and therefore are highly aesthetic. The glass in this category is mainly made up of a mined mineral called feldspar and is based on silica and alumina. Glasses composed of feldspar are resistant to crystallization during firing, have long firing ranges, and are biocompatible.
- •
Particle-filled glass, in which filler particles like Lucite are added to the glass matrix to improve its mechanical properties and to control optical effects such as opalescence, color, and opacity. Another advantage of adding leucite as a filler to ceramics is that its index of refraction is close to feldspathic and maintain translucency. It also etches at a faster rate than the base glass and creates selective etching. This property allows the resin cements to attach and form a good micromechanical bond. Dispersion strengthening is when the fillers are added and uniformly dispersed throughout the glass, creating an increase in strength. Leucite filler allows this phenomenon to occur. All of these advantages help strengthen the material without compromising the aesthetics.
- •
Polycrystalline ceramics contain no glass, the matrix is aluminum oxide or zirconium oxide, and the fillers are not particles but modifying atoms called dopants. These dopants are packed into regular crystalline arrays that are more difficult to crack than the irregular networks found in glasses. In general, polycrystalline ceramics are therefore stronger than glass-based ceramics.
Dental Computer-aided Design/Computer-aided Manufacturing Technology
Bioceramics have rapidly been adopted in dental restorations for implants, bridges, inlays, onlays, and all-ceramic crowns. The structures of dental bioceramics cover a wide spectrum of glass ceramics, reinforced porcelains, zirconias, aluminas, fiber-reinforced ceramic composites, and multilayered ceramic structures. Bioceramics in dental restorations are essentially oxide-based glass-ceramic systems and other traditional ceramic materials. The materials cover mica-containing glass ceramics, feldspar-containing porcelains, leucite-containing porcelains, glass-infiltrated alumina, and yttria-stabilized tetragonal zirconia. With increasing interest in improving the aesthetic quality of restorations, a wide variety of ceramic structures and their composites have also been developed, including the ceramic whisker-reinforced composites and the damage-resistant brittle-coating bilayer or trilayer structures. Over the past 25 years, computer-aided design (CAD) and computer-aided manufacturing (CAM) have become increasingly popular parts of dentistry. Dental CAD/CAM technology has been used to replace the laborious and time-consuming conventional lost-wax technique for efficient fabrication of restorations. This technology enables dentists to produce complex shapes of ceramic prostheses under the computer-controlled manufacturing conditions directly from the simply shaped blocks of materials within 1 hour. However, dental CAD/CAM systems use abrasive machining processes in which machining damage is potentially induced, resulting in the reduction of the strength of ceramic prostheses and the need for final finishing in oral conditions using a dental handpiece and diamond burs. It is expected that a ceramic restoration should have a high longevity. However, wear and fatigue damage are often observed to cause the failures of bioceramic prostheses. With the CAD/CAM systems, restorations can be produced quicker, which eliminates the need for temporary restorations. Moreover, with CAD/CAM, it is possible to make prostheses with consistent quality.
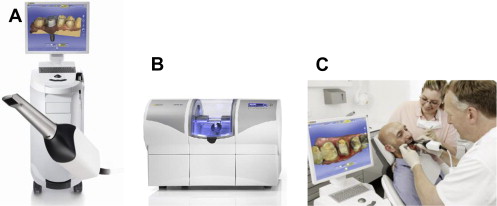
At present, there are 2 major CAD/CAM systems, one for machinable bioceramics, the other for materials that are difficult to machine. In the first system, the computer-assisted milling process can be used to machine the machinable ceramics directly from their blanks ( Fig. 1 ). In the second system, the milling process is first conducted from the presintered blanks of the difficult-to-machine ceramics, and then the sintering is followed to harden the ceramic prostheses, compensating for shrinkage during sintering in a special high-temperature furnace. In the CAD of prostheses, there are 2 digital image-generation systems for data acquisition. The three-dimensional (3D), noncontact, optical/laser scanning systems are most widely applied in dentistry.
The quality and the speed of intraoral imaging of the CAD/CAM process still need improvement.
CAD/CAM Components
There are 3 main sequences to CAD/CAD systems. The first sequence is to capture or record the intraoral condition to the computer. This sequence involves the use of a scanner or intraoral camera. Once the data have been recorded to the computer, a software program (CAD) is used to complete the custom design of the final desired restoration, which may involve a full contour design of the restoration or just the internal coping or substructure of the final restoration. The final sequence requires a milling device to fabricate the restoration from the design data in the CAD program. At present, the most common technique is a wet grinding subtractive milling process during which a preformed block of material is shaped by cutting instruments.
Results with in-office milling machines seem to be as good as those from laboratory milling machines. A systematic review of 16 articles that comprised 1957 restorations found no significant differences in 5-year survival rates between chairside CEREC (Chairside Economical Restoration of Esthetic Ceramics) restorations (90.2%–93.8%) and Celay laboratory restorations (82.1%).
Scanner
There are 2 different scanning possibilities:
- •
Optical scanner. This scanner uses the collection of 3D structures, for which the source of light and the receptor unit are in a definite angle in their relationship to one another. Through this angle the computer can calculate a 3D data set from the image on the receptor unit. Either white light projections or a laser beam can serve as a source of illumination.
- •
Mechanical scanner. In this scanner variant, the master cast is read mechanically line by line by means of a ruby ball and the 3D structure measured. The Procera Scanner from Nobel Biocare is one of the mechanical scanners in dentistry. This type of scanner is distinguished by a high scanning accuracy, whereby the diameter of the ruby ball is set to the smallest grinder in the milling system, with the result that all data collected by the system can also be milled. The drawbacks of this data measurement technique are in the highly complicated mechanics, which make the apparatus expensive with long processing times compared with optical systems.
Design software
Special software is provided by the manufacturers for the design of various kinds of dental restorations. With such software, crown and fixed partial denture (FPD) frameworks can be constructed. Some systems also offer the opportunity to design full anatomic crowns, partial crowns, inlays, inlay retained FPDs, as well as adhesive FPDs and telescopic primary crowns. The software of CAD/CAM systems presently available on the market is being continuously improved. The latest construction possibilities are continuously available to the user by means of updates. The data for the construction can be stored in various data formats. The basis is often standard transformation language (STL) data. However, many manufacturers use their own specific data formats, with the result that data for the construction programs are not compatible with each other.
CAD/CAM Development in Dentistry
The development of CAD/CAM is based around the data acquisition, data processing, and digital fabrication processes.
Digital data acquisition methods
The oral information for the patient can be directly extracted from a patient’s mouth or indirectly by means of a stone model generated through making an impression. The data acquisition techniques were originally developed for reverse engineering and intensively used in manufacturing industries. Their strengths were gradually recognized and these techniques are also applied in the medical field. The acquisition systems are divided into 2 basic categories: contact and noncontact digitizers.
The digital data acquired through various techniques and instruments are converted into a standard format so that the data can be processed using the capabilities of a CAD/CAM system.
This process is exemplified by the recent introduction of intraoral scanners, a number of which are now on the market: Lava COS (chairside oral scanner) from 3M, Trios from 3Shape and iTero from Cadent, and CEREC from Sirona.
A further development in the CAD/CAM technologies used in dentistry was the transition from closed to open access systems. Although in the past the digitizing, designing, and manufacturing came as a closed system (eg, CEREC), the technology is increasingly being opened up and the component parts of a CAD/CAM system can be purchased separately, which creates greater flexibility because data can be acquired from a range of sources (intraoral scanner, contact or laser model digitizer, computed tomography, magnetic resonance imaging). Another important consequence of the transition from closed to open systems is that this opens up access to a wider range of manufacturing techniques such that the most appropriate manufacturing processes and associated materials can be selected. Thus, clinicians are no longer constrained by the computer numerically controlled machining technologies that are currently used in most dental CAD/CAM systems.
Data processing and remodeling
CAD software is often used to edit and manipulate the point cloud data generated by a digitizer. After the point cloud data are converted into a representation of a surface or solid, the next step involves a digital design process for the dental part.
The shape design of the 3D dental restoration is one of the core elements of successfully fabricating restorations. In these systems the basic models of teeth are available in their own libraries. However, general forms of teeth geometry provided by these CAD/CAM systems can only give raw shapes. There are always some manual alterations and modifications required because every patient is unique and every tooth has its own topological features.
Digital fabrication processes
This is the last phase of the dental CAD/CAM process. It involves transforming a CAD model into a physical part that is later postprocessed and polished before being inserted into the patient’s mouth.
Industrial 3D printers have existed since the early 1980s, and have been used extensively for rapid prototyping and research purposes. These printers are generally large machines that use proprietary powdered metals, casting media (ie, sand), plastics, or cartridges, and are used for many rapid prototyping uses by universities and commercial companies. Several methods can be used to fabricate the physical parts. These methods can be additive or subtractive.
Subtractive manufacturing
Subtractive manufacturing removes material from a raw block to form an object of the desired shape and size, which can be done by conventional machining (eg, milling) and unconventional machining (eg, electrical discharge machining (EDM), laser machining).
CAD/CAM in dentistry is now primarily based around the process of subtractive manufacturing. The technology most people are familiar with is computer numerically controlled machining, which is based on processes in which power-driven machine tools, such as saws, lathes, milling machines, and drill presses, are used with a sharp cutting tool to mechanically cut the material to achieve the desired geometry, with all the steps controlled by a computer program. This method of manufacturing is wasteful because more material is removed than is used in the final product. The main advantage of this type of manufacturing is the ability of the technique to create fine detail such as undercuts, voids, and complex internal geometries. Another limitation of the current dental CAD/CAM systems is that the process does not easily lend itself to mass production, such as crowns and bridges, because only 1 part can be machined at a time.
Additive manufacturing
Additive manufacturing describes technologies that can be used anywhere throughout the product life cycle from preproduction (ie, rapid prototyping) to full-scale production (also known as rapid manufacturing) and even for tooling applications or postproduction customization. 3D printing is achieved using additive processes, in which laying down successive layers of material creates an object. The primary advantage of additive construction is its ability to create parts of almost any geometry, and the capability to spatially grade composition and/or microstructure (eg, porosity) to meet specific designs or needs, without requiring a previous mold. Also, this fabrication technology permits internal morphology, shape, distribution, and connectivity to be controlled more precisely. Another benefit from this system is the ability to print with multiple materials at one time as well as to create graded structures.
Modalities of Rapid Printing
The process of additive manufacturing is ideally suited to dentistry. Models are designed using data from a computed tomography scan or magnetic resonance imaging. The image is downloaded to a CAD machine and converted to an STL file. Various rapid prototyping technologies can be used to produce anatomic models:
- •
Stereolithography (SLA), which builds models by laser fusing a photopolymer layer by layer. SLA is now routinely used to produce surgical guides for the placement of dental implants. Its use is gradually being extended to include the manufacture of temporary crowns and bridges and resin models for loss wax casting.
- •
Laminated object manufacturing, which uses a laser to cut and fuse successive layers of bonded sheet material.
- •
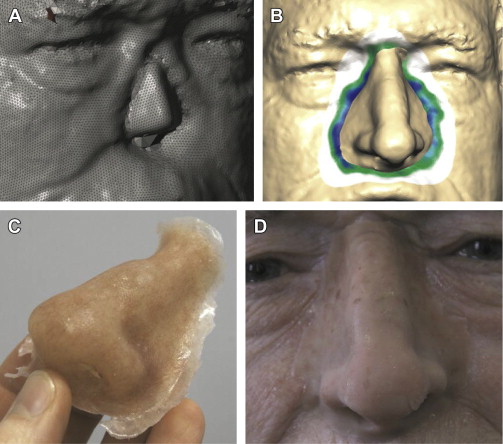
Laser powder forming techniques. Laser-based additive manufacturing, such as selective laser melting (SLM) and selective laser sintering (SLS), is accomplished by directing a high-power laser using mirrors at a substrate consisting of a fine layer of powder. Where the beam hits the powder it creates a melt pool and the powder particles fuse together. Compared with other methods of additive manufacturing, SLS/SLM can produce parts from a wide range of commercially available powder materials, including a wide range of polymers such as polyamide to produce a facial prosthesis, ultrahigh-molecular-weight polyethylene, polycaprolactone to provide functionally graded scaffolds, mixtures of polymers such as polycaprolactone and drugs to act as drug delivery devices, and composites such as mixtures of hydroxyapatite and polyethylene and polyamide to produce customized scaffolds for tissue engineering. A range of metal powders can be used that include steel, titanium, titanium alloys, and Co/Cr alloys.
- •
Solid ground curing, which laser polymerizes successive layers of resin through a stencil.
- •
Fused deposition modeling, which builds models by depositing layers of molten thermoplastic materials.
- •
Selective electron beam melting, which is a type of additive manufacturing for producing near net shape metal parts. The technology manufactures parts by melting metal powder layer by layer with an electron beam in a high vacuum. This technology has already found wide application in orthopedics and maxillofacial surgery for the construction of customized implants.
- •
3D ink-jet printing, which selectively deposits binding material through a print head to fuse a thin layer of powder to a previously fused layer. In direct ink-jet printing, a ceramic suspension provides the possibility of generating dense green bodies at a high resolution and in complex shapes.
With the improvements in the speed, reliability, and accuracy of the hardware, additive manufacturing will compete with traditional manufacturing in creating end-use products. One advantage with additive manufacturing is that it eliminates much of the expensive and highly skilled labor associated with traditional manufacturing. It can also make any number of complex products simultaneously so long as the parts fit within the build envelope of the machine. Thus the production of some 50 dental crown units that would normally take a considerable amount of time using loss wax casting can be done within a day, which has a profound influence on the dental technology community ( Fig. 2 ).
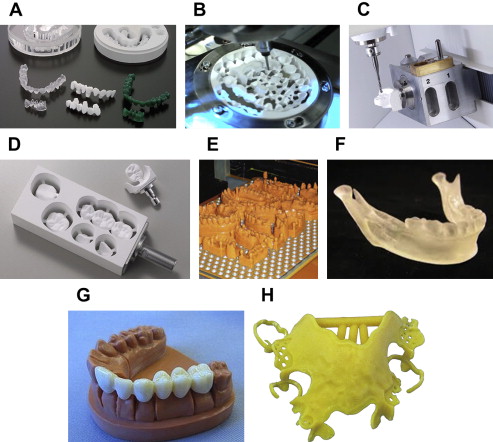
It is possible to build up dense 3D components of the size and shape of a dental crown out of high-strength zirconia ceramics by this technology. Although the microstructures of the printed and fired samples were not completely free of process-related defects, the obtained density was at 96.9% of the theoretic density required to provide mechanical properties. The shrinkage caused by drying or sintering can be a critical issue in individually made dental ceramic prostheses.
Two key challenges to successful printing of ceramic crowns by the robocasting technique are the development of suitable materials for printing and the design of printing patterns for assembly of the complex geometry required for a dental restoration.
Solid Free-form Fabrication Concept: Robocasting
Robocasting is a rapid prototyping (RP) that fabricates objects based on layering techniques. Robocasting uses computer-controlled extrusion of colloidal pastes (slurries, gels, or inks) onto a flat substrate without using molds or tooling. Unlike milling, in which blocks are cut back to create a form, robocasting uses a computer-generated scan from computed tomography of a SLA file to create a strategically printed 3D structure.
This process has been used in orthopedics for bone and tissue engineering. Robocasting in the dental setting is a new development with limited information or practice. The advantages of printing versus milling are the ability to make microstructure as needed for the prosthesis without requiring a previous mold; that it allows internal morphology, shape, distribution, and connectivity to be controlled more precisely; and a significant decrease in waste of materials.
To achieve its full potential as a dental restoration production process, robocasting must improve the use of support materials to produce better tolerance for occlusal surfaces. In addition, the digital nature of the layer printing process leads to a stair-stepped surface that may need to be improved for commercial acceptance. The step size is a function of the nozzle diameter used for printing. The issue of support materials/structures seems to be a tractable problem; however, the stair stepping may require some postprocessing (eg, a dip-coating process) before final sintering. Drying issues, such as cracks, sometimes occur ( Fig. 3 ).
Digital Imaging in Different CAD/CAM Systems
The following are a few of the currently available products for digital impressions in the dental office: CEREC AC (Sirona, Charlotte, NC), E4D Dentist (D4D Technologies, Richardson, TX), iTero (Cadent, Carlstadt, NJ), Lava COS (3M ESPE, St Paul, MN), and 3Shape TRIOS (3Shape, Copenhagen, Denmark). The CEREC and E4D devices can be combined with in-office design and milling, whereas the iTero and Lava COS devices are reserved for image acquisition only. In-office milling allows same-day restorations.
The CEREC system
CEREC, introduced in 1987, was the first dental system to combine digital scanning with a milling unit. The first grinding trials with a simple device on bodies made of feldspathic ceramic (Vita Zahnfabrik, Bad Säckingen, Germany) showed that this material could be removed with a grinding wheel in a few minutes without damaging the rest of the bulk. Then the ceramic block could hold on the block carrier with a spindle and feed it against the grinding wheel, which ground from the full ceramic a new contour with a different distance from the inlay axis at each feed step. This solution proved itself in a prototype implemented in the same year in the CEREC 1 unit (Sirona Dental Systems GmbH, Bensheim, Germany). A CEREC team at Seimens (Munich, Germany) equipped the CEREC 2 with an additional cylinder diamond enabling the form grinding of partial and full crowns. CEREC 3 skipped the wheel and introduced the 2-bur system. The step bur, which was introduced in 2006, reduced the diameter of the top one-third of the cylindrical bur to a small-diameter tip, enabling high precision form grinding with reasonable bur life.
In 2009, the newest model known as CEREC AC powered by BlueCam (Sirona, Charlotte, NC) was introduced, which has the ability to take half-arch or full-arch impressions and create crowns, veneers, and bridges. The current acquisition system uses intense blue light from blue light emitting diodes (LEDs). The camera records a series of overlapping single images that the software converts into a 3D virtual model. The camera projects blue light onto the teeth, which reflect it back at a slightly different angle. This method of visualization is referred to as active triangulation.
To use the system, the tooth preparation to be scanned is coated with a layer of special titanium dioxide powder, which makes translucent areas of the teeth opaque and permits the camera to register all of the tissues. Several optical impressions are then taken from an occlusal orientation. The shorter wavelength of the LED blue light has been measured to have a higher resolution compared with that of a red laser.
After the impression is complete, a 3D rendering of the tooth to be restored appears on the monitor. The dentist is able to mark where the die should begin and end based on this image. The software program then generates a proposed restoration based on comparisons with the surrounding teeth, which can then be altered or fine tuned as needed. After the design is approved, the milling process can begin. A block of ceramic or composite material in the correct color is inserted into the milling unit.
As an alternative, the dentist can obtain a digital impression and send the data to a dental laboratory. The laboratories can then design and mill the restoration using CAD/CAM technology. They can also use the digital image to fabricate a hard resin model based on the data and proceed to fabricate the restoration in the conventional manner.
The E4D dentist system
E4D was introduced by D4D Technologies LLC (Richardson, TX) in early 2008 and it is presently the only other system besides CEREC that permits same-day in-office restorations. The system consists of a cart containing the design center and laser scanner, a separate milling unit, and a job server and router for communication. The scanner, termed the intraoral digitizer, has a shorter vertical profile than that of the CEREC, so the patient is not required to open as wide for posterior scans. The E4D does not require the use of reflected agent powder to enable capture of fine detail on the target site in most cases. Therefore, scanning begins by simply placing the intraoral digitizer directly above the prepared tooth. The scanner must be held a specific distance from the surface being scanned; this is achieved with the help of rubber-tipped boots that extend from the head of the scanner. It is not necessary to scan the opposing arch. Occlusal registration is created with an impression material, trimmed, and then placed on top of the prepared tooth; the scanner captures a combination of the registration material and the neighboring teeth that are not covered by the material. These data are used to design restorations with proper occlusal heights. Once the final restoration is approved, the design center transmits the data to the milling machine. Using blocks of ceramic or composite mounted in the milling machine, and with the aid of rotary diamond instruments that are capable of replacing themselves when worn or damaged, the dentist is able to fabricate the completed restoration.
The Cadent iTero
Cadent introduced iTero in 2007 as the first digital impression system for conventionally manufactured crowns and bridges. Unlike the other systems, which acquire images using triangulation, iTero uses a parallel confocal white light and laser light camera to record a series of single images to create a 3D model. The cadent iTero scanner captures 100,000 points of red laser light and has perfect focus images of more than 300 focal depths of the tooth structure. An advantage of the iTero camera is the ability to scan without the need of any agent powder, resulting in a camera with a larger head than the other systems.
Once the digital impression has been completed the dentist can select from a series of diagnostic tools to evaluate the preparation and complete the impression. The occlusal reduction tool shows in vivid color how much clearance has been created in the preparation for the restoration selected by the dentist. A margin line tool is available to assist in viewing the clearly defined margin. The completed digital impression can be sent through a Health Insurance Portability and Accountability Act (HIPAA)-complaint wireless system to a Cadent facility and the dental laboratory. The model is milled from a property-blended resin and is pinned, trimmed, and articulated based on the digital impression created by the dentist. Cadent uses an industrial 5-axis milling machine to ensure the precision of the milled model and dies.
Lava COS
Lava was created at Brontes Technologies (Lexington, MA) and was acquired by the 3M ESPE (St Paul, MN) in October 2006. The Lava COS system consists of a mobile cart, a touch screen display, and a scanner with a camera at the end. The camera tip of the wand contains 192 lens data system (LDS) and 22 lens systems.
The method used for capturing 3D impressions involves active wave front sampling.
The Lava COS concept of 3D in motion incorporates revolutionary optical design, image processing algorithms, and real-time model reconstruction to capture 3D data in a video sequence and model the data in real time. The scanning wand contains a complex optical system composed of multiple lenses and blue light-emitting diode (LED) cells. The Lava COS is therefore able to capture approximately 20 3D data sets per second or close to 2400 data sets per arch, for an accurate and high-speed scan. After the preparation of the tooth and gingival retraction, the arch is dried and lightly dusted with powder. The Lava COS only requires enough agent powder to allow the scanner to locate reference points, not heavy powdering as with the CEREC. When all the scans have been reviewed for accuracy, the dentist fills out a 1-screen laboratory prescription. The data are wirelessly sent to the laboratory technician, who then uses customized software to digitally cut the die and mark the margin, and also to create an articulated SLA model that a dental laboratory uses to design any type of restoration, such as crowns, inlays, onlays, and bridges, and not just Lava.
3M True Definition scanner
The True Definition scanner delivers powerful 3D video-based scanning technology and provides scanning precision, accuracy, and repeatability for taking digital impressions. The technology is contained in a small, ergonomic, lightweight wand the size of a dental headpiece. The system also offers users the 3M connection center, which is built on a secure, cloud-based architecture that provides both trusted and integrated connections to third-party systems, along with the flexibility of open STL file systems. The wand part does not require calibration, and the monitor and computer have been built through a partnership with Hewlett-Packard.
Lava Ultimate Restorative
Lava Ultimate Restorative is a combination of 3M ESPE’s Lava COS, Lava Design software, and resin nano ceramic. This combined technology allows clinicians and laboratory technicians to work together as a team to create high-quality restorations. Lava COS provides accuracy in scanning and Lava Design software offers exceptional marginal fit in zirconia and other materials.
3Shape TRIOS
3Shape’s Ultrafast Optical Sectioning technology enables dentists to rapidly and easily achieve accurate scans with minimum discomfort for the patient. Unlike most other scanners, 3Shape TRIOS is a no-spray solution.
This technology captures more than 3000 two-dimensional images per second; 100 times faster than conventional video cameras. It combines hundreds or thousands of 3D pictures to create the final 3D digital impression based on real data rather than interpolated artificial surfaces. There is no need to hold the scanner at a specific distance or angle for focus, and dentists can rest the scanner on the teeth for support as they scan. 3Shape TRIOS provides optimized scanning for an extensive range of dental indications including inlays/onlays, crowns (with subgingival preparations), bridges, temporaries, diagnostic wax-ups, veneers, and implant cases.
Influence of Scan Spray Systems on Human Gingival Fibroblasts
Chairside CAD/CAM devices, which can produce ceramic restorations of high durability combined with excellent aesthetic results, usually require opaque surfaces.
Standardized spray systems, which coat the teeth with a titanium dioxide powder to enhance their opacity, represent a necessary and vital part of some systems.
Willershausen and colleagues tested 3 different spray systems (ScanDry, Scan Spray Luer Classic, and CEREC Optispray) to determine their effects on proliferation, viability, and adenylate kinase (ADK) release of human periodontal fibroblasts. Any potential toxic effect would be reflected in the release of ADK after cellular contact of the used materials. The aforementioned results suggest that when scan spray particles are accidentally left in the oral cavity after the spraying process they are not likely to result in increased ADK levels, which showed no harmful effect in vitro.
Dental Materials and CAD/CAM
With the introduction of advanced CAD/CAM technologies, various high-strength ceramic materials were developed and are increasingly used in dentistry.
However yttria-stabilized tetragonal zirconia polycrystalline (Y-TZP) frameworks exhibit unsurpassed mechanical properties, reflected by high survival rates in clinical application. Because of the high reported veneer failure rates with zirconia-based fixed dental prostheses (FDPs), high-strength glass-ceramic systems in monolithic and bilayer applications have regained increased consideration for anterior and posterior restorations.
Lithium Disilicate
Lithium disilicate has been indicated for use in thin veneers, minimally invasive inlays and onlays, crowns, implant superstructures, and FPDs. At present there are 2 methods to fabricate a restoration from lithium disilicate glass ceramic. The first method, or the original technique, is the lost-wax/heat-pressing method. A wax pattern is hand made and then the heated ceramic ingot is forced through a heated tube into a mold. More recently, a restoration from lithium disilicate glass-ceramic blocks has been designed and milled from a ceramic block, using CAD/CAM.
Lithium disilicate ceramic (IPS Empress II, Ivoclar Vivadent, Schaan, Liechtenstein) using the lost-wax press technique was introduced in 1998 as an enhanced glass-ceramic system for single tooth and anterior 3-unit FDP restorations. Although this all-ceramic system was successful in anterior and posterior crown indications, heterogeneous survival rates ranging from 50% after 2 years to 70% after 5 years were reported for bilayer FDP applications.
In 2001, IPS e.max Press (Ivoclar Vivadent, Schaan, Liechtenstein) was released to the market with significantly improved mechanical and optical properties. Higher translucency and augmented shade variety enabled this lithium-disilicate glass-ceramic material in posterior indication for monolithic full anatomic restoration fabrication with subsequent staining characterization. A promising survival rate of 87.9% after 10 years has been reported for monolithic posterior 3-unit FDP applications.
Silica-based ceramic blocks are offered by several CAD/CAM systems. In addition to monochromatic blocks, various manufacturers now offer blanks with multicolored layers (Vitablocs TriLuxe [Vita], IPS Empress CAD Multi [Ivoclar Vivadent]), for the purpose of full anatomic crowns. Because of their higher stability values, lithium disilicate ceramic blocks are particularly important in this group; they can be used for full anatomic anterior and posterior crowns, for copings in the anterior and posterior region, and for 3-unit FPD frameworks in the anterior region because of their high mechanical stability of 360 MPa. Glass ceramics are particularly well suited to chairside application as a result of their translucent characteristics, similar to that of natural tooth structure; they provide aesthetically pleasing results even without veneering. Lithium disilicate is also biocompatible, provides diminished plaque accumulation, low thermal conductivity, and color stability.
In certain clinical situations, lithium disilicate restorations should not be placed, such as a limited interocclusal distance and in patients with parafunctional habits. Disadvantages of lithium disilicate restorations include the brittleness of the ceramic and their low to moderately high flexural strength and fracture toughness. Because lithium disilicate has these properties, its use and placement should be restricted to low-stress to moderate-stress environments and adequate thickness of the ceramic should be provided to avoid the fracture of the restoration. Another major disadvantage to lithium disilicate is the damaging wear it can cause to the opposing tooth structure. Under certain conditions, the damage can increase, especially when a roughened surface (created through parafunctional habit, premature occlusal contact, and/or inadequate occlusal adjustments) contacts tooth enamel or dentin under high occlusal forces. To decrease this chance of occlusal wear, the clinician should ensure cuspid-guided disclusion.
A dry field and good moisture control from saliva should be maintained during final cementation to ensure a positive outcome when using lithium disilicate restorations. In terms of surface treatment of the ceramic material before final cementation, etch with hydrofluoric acid, application of a silane primer, and using adhesive systems have been recommended and showed improved bond strengths.
Infiltration ceramics
These blocks are processed in porous, chalky conditions and then infiltrated with lanthanum glass. They originate from the Vita In-Ceram system (Vita) and are offered in 3 variations:
- •
Vita In-Ceram Alumina (Al 2 O 3 ): suitable for crown copings in the anterior and posterior regions, and 3-unit FPD frameworks in the anterior region.
- •
Vita In-Ceram Zirconia (70% Al 2 O 3 , 30% ZrO 2 ): suitable for crown copings in the anterior and posterior regions, and 3-unit FPD frameworks in the anterior and posterior regions. Because of its superior masking ability, this ceramic is suitable for discolored abutment teeth.
- •
VITA In-Ceram Spinell (Mg Al 2 O 4 ): has the highest translucency of all oxide ceramics and is thus recommended for the production of highly aesthetic anterior crown copings, in particular on vital abutment teeth and in young patients.
Oxide high-performance ceramics
At present, aluminum oxide and zirconium oxide are offered as blocks for CAD/CAM technology.
Al 2 O 3
This oxide high-performance ceramic is ground in a presintered phase and is then sintered at a temperature of 1520°C in the sintering furnace. Aluminum oxide is indicated in the case of crown copings in the anterior and posterior area, primary crowns, and 3-unit anterior FPD frameworks. The ground frames can be individually stained in several colors with Vita In-Ceram AL Coloring Liquid. Examples of aluminum oxide blocks include In-Ceram AL Block (Vita) and inCoris Al (Sirona), which are available in an ivorylike color.
Yttrium stabilized zirconium oxide (ZrO 2 , Y-TZP)
Zirconium dioxide is a high-performance oxide ceramic with excellent mechanical characteristics. It has high flexural strength and fracture toughness compared with other dental ceramics, which offers the possibility of using this material as a framework for crowns and FPDs, and, in appropriate indications, for individual implant abutments.
Zirconia
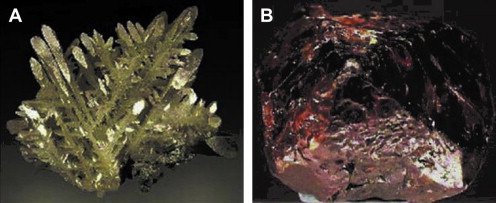
Zirconium minerals were discovered decades ago but are still referred to as jargon, jacinth, and hyacinth. The name zirconium (Zr) comes from the Arabic word zargon (golden in color), which in turn derives from 2 Persian words: zar (gold) and gun (color). The metal dioxide zirconia was discovered by the German chemist Martin Heinrich Klaproth in 1789 and was isolated by the Swedish chemist Jons Jacob Berzelius in 1824.
Zirconium dioxide (ZrO 2 )
Known as zirconia, this is a white crystalline oxide of zirconium. Although pure zirconium oxide does not occur in nature, it is found in the minerals baddeleyite and zircon (ZrSiO 4 ) ( Fig. 4 ). Zirconium oxide crystals are arranged in crystalline cells that are categorized in 3 crystallographic phases: (1) the cubic (C) in the form of a straight prism with square sides, (2) the tetragonal (T) in the form of a straight prism with rectangular sides, and (3) the monoclinic (M) in the form of a deformed prism with parallelepiped sides. The cubic phase is stable at more than 2370°C and has moderate mechanical properties; the tetragonal phase is stable between 1170°C and 2370°C and allows a ceramic with improved mechanical properties to be obtained; whereas the monoclinic phase, which is stable at room temperatures up to 1170°C, presents reduced mechanical performance and may contribute to a reduction in the cohesion of the ceramic particles and thus of the density.