Introduction
Our aim was to determine differences between the outcomes of treatment using microimplant anchorage compared with headgear anchorage in adult patients with bimaxillary protrusion treated with self-ligating brackets.
Methods
Thirty-one adult orthodontic patients (13 men, 18 women; age, 25.87 ± 3.37 years) who were diagnosed with bimaxillary protrusion were selected. All patients were treated with self-ligating brackets and maximum anchorage after extraction of 4 first premolars. Group 1 received microimplant anchorage, and group 2 received headgear. Lateral cephalometric radiographs were obtained before and after treatment. Differences in the skeletal and dental parameters between and within groups were analyzed.
Results
No significant difference was observed in the mean treatment times between the groups (21.93 ± 3.10 vs 23.88 ± 2.68 months). There was no significant difference in skeletal measurements before or after treatment in patients who received microimplant anchorage. Patients who received headgear anchorage had an increase of the mandibular plane angle. The microimplant anchorage group had greater anterior tooth retraction and less maxillary molar mesialization than did the headgear group.
Conclusions
In both the anteroposterior and vertical directions, microimplant anchorage achieved better control than did the traditional headgear appliance during the treatment of bimaxillary protrusion.
Highlights
- •
Self-ligating brackets with implant anchorage might not shorten orthodontic treatment time.
- •
Microimplant anchorage achieved better control in both the anteroposterior and vertical directions.
- •
Microimplants may result in more retraction of the maxillary incisors.
- •
Microimplants may result in less anchorage loss of the maxillary first molar.
Bimaxillary protrusion is a condition characterized by protrusive and proclined maxillary and mandibular incisors, and increased procumbency of the lips. It is seen commonly in African-American and Asian populations. In bimaxillary protrusion patients, the major orthodontic treatment goal includes retraction and retroclination of the maxillary and mandibular incisors with a resultant decrease in soft tissue procumbency. It is rather well accepted by clinicians that extraction of the 4 first premolars followed by retraction of the anterior teeth with maximum anchorage mechanics can be effective in the treatment of bimaxillary protrusion.
Maximum anchorage to prevent forward movement of the maxillary posterior teeth during anterior tooth retraction can be provided with different approaches. Extraoral headgear appliances are commonly used to reinforce posterior anchorage during anterior tooth retraction or are directly applied to retract anterior teeth. However, wearing headgear full time is too demanding for most patients, and thus some anchorage loss and mesial movement of the maxillary molars are usually observed. Patient cooperation is an important factor for the effectiveness of extraoral appliances. Microimplants are increasingly used as orthodontic anchorage sources. It has been reported that implant anchorage can provide stable bony anchorage and overcome problems of anchorage loss during extraction space closure, which usually occurs with traditional anchorage preparations. Application of implant anchorage also makes teeth move more efficiently, without depending on patient cooperation in wearing an extraoral appliance, and consequently reducing treatment duration. However, in the treatment of bimaxillary protrusion in adults, only a few studies to date have statistically investigated the effectiveness of the implant anchorage system, with little statistical evaluation of the treatment effects of the implant anchorage system compared with the effects of headgear.
Orthodontics, just as any other science, has undergone advances in technology that aim to improve treatment efficacy with a view to reducing treatment time, providing patients with comfort and achieving the expected, yet rarely obtained, long-term stability. Recently, there has been increased use of the self-ligating brackets (SLBs) in orthodontic clinics worldwide. SLBs are popular in orthodontics because of their proposed superior properties including low static frictional resistance, full and stable archwire engagement, improved oral hygiene, preserved anchorage, reduced chair time and therapeutic time, and prolonged therapeutic intervals. Several researchers compared therapeutic efficiency, friction, speed of archwire changes, therapeutic time, and initial alignment of the mandibular arch between self-ligating and conventional brackets.
Although more patients were treated with SLBs, there is little research about whether there are significant clinical differences between microimplant anchorage and headgear anchorage in patients with bimaxillary protrusion malocclusion treated with SLBs. The objective of this study was to assess, in adults with bimaxillary protrusion, the effectiveness of orthodontic anchorage when using either microimplants or extraoral headgear with the SLB system.
Material and methods
Ethical approval was obtained from the ethics committee of the Guanghua College of Stomatology in China. A letter was sent to the subjects to seek consent for their participation in the study. This letter also informed them about the examination procedures and assured them of confidentiality of any information collected. Only patients who actively consented were included.
A consecutive sample of adults seeking orthodontic care at a state-funded hospital clinic was recruited. We excluded those who lacked the data required for our research, missed 3 or more appointments, and had unclear pretreatment or posttreatment lateral cephalograms. Patients were diagnosed with bimaxillary protrusion based on cephalometric evaluations and study models, which required the extraction of 4 first premolars and maximum anchorage to obtain a satisfactory treatment. They were divided into 2 groups according to the type of anchorage preparation. The choice of microimplant or headgear anchorage was made by each patient according to his or her own judgment on compliance, because both modes of anchorage preparation were available. In group 1 (15 patients; 6 men, 9 women; age, 26.53 ± 3.54 years), titanium microimplants were used for anchorage. Each patient received implantation of microimplants on the buccal aspect of the bilateral maxillary posterior teeth. After administration of local anesthesia, OrthoEasy (Forestadent, Pforzheim, Germany) orthodontic microimplants (length, 9.0 mm; diameter, 1.6 mm) were placed between the maxillary second premolars and the first molars without flap elevation at the apical level. In group 2 (16 patients; 7 men, 9 women; age, 25.25 ± 3.19 years), the patients received traditional anchorage preparation with a headgear appliance (Shinye Odontological Materials, Hangzhou, China). The force level exerted by the headgear was 300 to 350 g. The directional pull of the headgear was adjusted according to the mandibular plane angle. All subjects received passive SLBs (Forestadent) brackets. In both groups, nickel-titanium wires for aligning and leveling were used with the same sequence of archwires beginning with 0.014-in, 0.016-in, and 0.018-in, until a 0.018 × 0.025-in base archwire was inserted. In both groups with either traditional extraoral anchorage or microimplant anchorage, the extraction space was closed by sliding mechanics with en-masse retraction after partial canine distalization to resolve the anterior crowding and to achieve good alignment of the 6 anterior teeth. All treatments and anchorage preparations were conducted after obtaining the patient’s informed consent. Treatment procedures were taught and monitored by 1 clinical instructor (D.-W.W.) so that consistent mechanical principles were maintained.
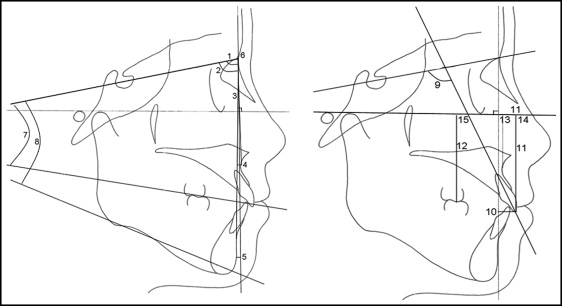
Lateral cephalometric radiographs were taken immediately before and after treatment for all subjects. Tracing, superimposition, and measurement were undertaken manually by 2 examiners (M.C., Z.-C.F.). Bilateral structures were bisected, and their midsagittal points were identified. The cephalometric parameters, including 8 skeletal measurements and 7 dental measurements used in this study, are shown diagrammatically according to the study of Yao et al ( Fig 1 ).
Statistical analysis
Descriptive and analytical statistical analyses were performed with the Statistical Package for the Social Sciences (version 15.0; SPSS, Chicago, Ill) for Windows. To assess intraexaminer and interexaminer reliabilities, the cephalometric radiographs were retraced and remeasured by the same 2 examiners after a period of 3 months. The results of the analysis indicated no statistically significant differences between the original and repeated measurements at the 0.05 level. Statistical analysis was undertaken to determine whether any significant differences existed between groups 1 and 2 before treatment. For the microimplant and headgear groups, the means and standard deviations of the pretreatment and posttreatment cephalometric measurements were calculated and compared using paired-samples t tests. Differences in treatment changes between the 2 groups were evaluated with the independent-samples t test. A P value less than 0.05 was considered statistically significant.
Results
No significant differences were found for any measurements before treatment in either group ( Table I ). The mean treatment duration of the microimplant group (21.93 ± 3.10 months) was less than that of the headgear group (23.88 ± 2.68 months). However, the difference did not reach statistical significance ( P = 0.07).
| Group 1 | Group 2 | P | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (y) | 26.53 | 3.54 | 25.25 | 3.19 | 0.30 |
| Treatment duration (mo) | 21.93 | 3.10 | 23.88 | 2.68 | 0.07 |
| Sex (male/female) | 6/9 | 7/9 | |||
| Skeletal measurements | |||||
| SNA (°) | 81.53 | 2.70 | 80.31 | 3.20 | 0.26 |
| SNB (°) | 78.60 | 3.09 | 78.19 | 1.80 | 0.65 |
| ANB (°) | 2.93 | 2.52 | 2.13 | 2.47 | 0.38 |
| A-Nv (mm) | −0.83 | 0.20 | −1.00 | 0.37 | 0.13 |
| Pog-Nv (mm) | −12.94 | 2.04 | −12.09 | 2.09 | 0.26 |
| NAPog (°) | 11.00 | 2.04 | 9.75 | 2.07 | 0.10 |
| SN-OP (°) | 17.10 | 3.69 | 17.56 | 3.43 | 0.72 |
| SN-MP (°) | 33.60 | 5.45 | 34.75 | 6.38 | 0.60 |
| Dental measurements | |||||
| U1-SN (°) | 113.27 | 5.70 | 117.13 | 5.40 | 0.06 |
| U1-NPog (mm) | 17.93 | 3.99 | 19.00 | 3.69 | 0.45 |
| U1-FH (mm) | 60.33 | 4.19 | 63.06 | 3.60 | 0.06 |
| MFH (mm) | 51.30 | 3.00 | 53.19 | 2.64 | 0.07 |
The original dentofacial characteristics and treatment changes measured from the paired pretreatment and posttreatment cephalograms of the 2 groups are shown in Table II . There were no significant differences in the skeletal measurements before or after treatment in group 1. In the dental measurements, the mean decreases were 11.87° in the proclination of the maxillary incisor (U1-SN angle) and 8.37 mm in the sagittal measurements of U1 (U1-NPog distance) ( P <0.01). The tip of the maxillary incisor (UU′) was retracted by 10.27 mm ( P <0.01), and mesial movement of the maxillary first molar (MM′) was 0.87 mm ( P <0.05). In group 2, the SN-MP angle was significantly increased (1.19°, P <0.01) after treatment, but there were no significant treatment changes of other skeletal measurements. In dental measurements, the maxillary incisors were retroclined by a mean of 11.13° (U1-SN angle) and retracted by a mean of 6.63 mm (U1-NPog), whereas the tip of the maxillary incisor was retracted by 6.88 mm, and mesial movement of the maxillary first molar was 2.19 mm ( P <0.01).
| Microimplant group | P | Headgear group | P | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment | Posttreatment | Difference | Pretreatment | Posttreatment | Difference | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Skeletal measurements | ||||||||||||||
| SNA (°) | 81.53 | 2.70 | 81.33 | 2.74 | −0.20 | 0.41 | 0.08 | 80.31 | 3.20 | 80.06 | 2.95 | −0.25 | 0.58 | 0.10 |
| SNB (°) | 78.60 | 3.09 | 78.47 | 3.04 | −0.13 | 0.35 | 0.16 | 78.19 | 1.80 | 78.00 | 1.79 | −0.19 | 0.66 | 0.27 |
| ANB (°) | 2.93 | 2.52 | 2.87 | 2.39 | −0.07 | 0.46 | 0.58 | 2.13 | 2.47 | 2.06 | 2.43 | −0.06 | 0.44 | 0.58 |
| A-Nv (mm) | −0.83 | 0.20 | −0.91 | 0.30 | −0.07 | 0.18 | 0.13 | −1.00 | 0.37 | −1.03 | 0.35 | −0.03 | 0.07 | 0.10 |
| Pog-Nv (mm) | −12.94 | 2.04 | −12.92 | 2.05 | −0.02 | 0.08 | 0.33 | −12.09 | 2.09 | −12.19 | 2.05 | 0.09 | 0.20 | 0.08 |
| NAPog (°) | 11.00 | 2.04 | 10.80 | 2.28 | −0.20 | 0.77 | 0.33 | 9.75 | 2.07 | 10.17 | 1.93 | 0.42 | 0.93 | 0.09 |
| SN-OP (°) | 17.10 | 3.69 | 17.37 | 3.74 | 0.27 | 0.59 | 0.10 | 17.56 | 3.44 | 18.06 | 3.80 | 0.50 | 1.03 | 0.07 |
| SN-MP (°) | 33.60 | 5.45 | 33.33 | 5.56 | −0.27 | 0.59 | 0.10 | 34.75 | 6.38 | 35.94 | 6.81 | 1.19 | 1.33 | 0.00 ∗ |
| Dental measurements | ||||||||||||||
| U1-SN (°) | 113.27 | 5.70 | 101.40 | 5.77 | −11.87 | 1.51 | 0.00 ∗ | 117.13 | 5.40 | 106.00 | 5.11 | −11.13 | 1.82 | 0.00 ∗ |
| U1-NPog (mm) | 17.93 | 3.99 | 9.57 | 3.13 | −8.37 | 1.96 | 0.00 ∗ | 19.00 | 3.69 | 12.38 | 2.78 | −6.63 | 2.55 | 0.00 ∗ |
| U1-FH (mm) | 60.33 | 4.19 | 60.20 | 4.16 | −0.13 | 0.52 | 0.33 | 63.06 | 3.60 | 63.25 | 3.82 | 0.19 | 0.54 | 0.19 |
| MFH (mm) | 51.30 | 3.00 | 51.20 | 3.08 | −0.10 | 0.21 | 0.08 | 53.19 | 2.64 | 53.25 | 2.77 | 0.06 | 0.31 | 0.43 |
| AA′ (mm) | −0.27 | 0.55 | 0.08 | −0.22 | 0.54 | 0.13 | ||||||||
| UU′ (mm) | −10.27 | 3.51 | 0.00 ∗ | −6.88 | 2.55 | 0.00 ∗ | ||||||||
| MM′ (mm) | 0.87 | 1.46 | 0.04 ∗ | 2.19 | 1.68 | 0.00 ∗ | ||||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


