Diagnostics of Orofacial Pain and Temporomandibular Disorders
Thomas List and Richard Ohrbach
Temporomandibular disorders (TMDs) and orofacial pain occur in about 5–12% of the adult population and in approximately 4–7% of youth and adolescents (Drangsholt, 1999; Nilsson et al., 2005; NIDCR, 2014). About half of the individuals with TMD and orofacial pain perceive a need for treatment and seek consultation (Nilsson et al., 2009; NIDCR, 2014). The consequences of TMD and orofacial pain for the patient are often a limitation in daily activities, lower quality of life, and personal suffering; the consequences for society include high economic costs for treatment and loss of productivity (NIDCR, 2014).
Although several professional groups routinely encounter patients with TMD and orofacial pain, it is the general practicing dentist who will initially manage the care of these patients. One problem is that general dentists are often unsure about diagnosing patients with TMD and orofacial pain (Tegelberg et al., 2001). Thus, there is great need for a simplified and reliable diagnostic classification with clear instructions on how to conduct the clinical examination and which questions to ask in the history to get an overall picture of the patient’s difficulties and choose suitable therapy. In addition to determining diagnoses through the examination of subjective symptoms and clinical findings, it is important to assess the patient’s psychosocial status, including the consequences of chronic pain, in order to reveal an overall picture of the patient. The clinical condition (Axis I) and the psychosocial assessment (Axis II) together provide the information necessary for planning and executing suitable therapy with an optimal prognosis.
Diagnostic Classifications
There are many diagnostic systems for TMD and orofacial pain (Dworkin and LeResche, 1992; de Leeuw and Klasser, 2013; Headache Classification Committee of the International Headache Society (IHS), 2013; Peck et al., 2014; Schiffman et al., 2014). Of these, the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) and the American Academy of Orofacial Pain (AAOP) diagnostic criteria for TMD-related masticatory disorders have been the ones most used internationally (Dworkin and LeResche, 1992; de Leeuw and Klasser, 2013). The RDC/TMD standardized assessment of the most common TMD diagnoses and the AAOP criteria, while not as strictly defined, covered a larger range of conditions.
The RDC/TMD has been translated into more than 20 languages, and the publication that introduced it is one of the most cited in the dental literature (Dworkin and LeResche, 1992; List and Greene, 2010). After identification of some limitations of the system, the RDC/TMD was revised and the new classification system Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) (Schiffman et al., 2014) was developed, which was also incorporated into the newest edition of the AAOP guidelines (de Leeuw and Klasser, 2013), thereby bringing research and clinical practice together.
The most common temporomandibular disorders
The DC/TMD is based both on extensive multicenter clinical studies, including studies funded by the National Institutes of Health in the USA, and on international consensus conferences (Schiffman et al., 2014). It is important to point out here that the DC/TMD only covers the most commonly occurring TMD conditions. The DC/TMD is comprised of two domains: a physical Axis I and a psychosocial Axis II.
The strength of the DC/TMD Axis I protocol includes reliable and valid diagnostic criteria for the common pain-related disorders and for the intraarticular disorders. The Axis I protocol provides standardized evaluation of subjective symptoms, contains clearly defined examination methods, and utilizes specific diagnostic criteria based on the clinical findings. The Axis II protocol, a psychosocial assessment, is simplified compared with the RDC/TMD version and has two options: a brief assessment and a comprehensive set of instruments for expanded assessment. The AAOP guidelines, in parallel, include the 12 common DC/TMD diagnoses.
Less common temporomandibular disorders: the expanded taxonomy
The DC/TMD covers the most common TMD conditions for which data were readily available. This created a need to expand the taxonomy to cover less common but still clinically relevant conditions. The expanded taxonomy (Peck et al., 2014) is a consolidation of the common disorders in the DC/TMD and the less common disorders described in the fourth edition of the AAOP guidelines for TMD (De Leeuw, 2008). The expanded taxonomy defines the diagnostic criteria for the less common TMD conditions and includes a total of 37 disorders; for example, temporomandibular joint (TMJ) arthritis in cases of systemic inflammatory diseases, local TMJ arthritis, ankylosis, myositis, and orofacial dyskinesia (Peck et al., 2014) (Table 1.1). Note that while the diagnostic criteria for the less common disorders are clearly stated such that each disorder is defined without overlap, the criteria have not yet been operationalized; in addition, there is at present no information regarding the sensitivity, specificity, reliability, or validity of the diagnoses for these less common conditions (Peck et al., 2014).
Table 1.1 Expanded taxonomy of the DC/TMD
|
|
* DC/TMD with sensitivity and specificity.
Other orofacial pain conditions
Other orofacial pain conditions – such as trigeminal neuropathic pain, persistent idiopathic orofacial pain, and burning mouth syndrome – are not included in the expanded taxonomy because they are considered to be orofacial pain conditions, not TMDs. Other classification systems should be consulted in order to diagnose these conditions.
Trigeminal neuropathic pain is caused by injury or diseases of the peripheral or central somatosensory nervous system. The pain is usually constant with variations in intensity over several days, but, in rare cases, it may also occur intermittently throughout the day. Pain from normally nonpainful stimuli (such as touch, pressure, or cooling) can be a significant part of suffering in trigeminal neuropathic pain.
Treede and colleagues have published a frequently used diagnostic algorithm for neuropathic pain, proposing three levels of pain (Treede et al., 2008; Geber et al., 2009).
Possible neuropathic pain
This requires both of the following:
- i. Pain distribution is neuroanatomically plausible.
- ii.
History suggests lesion or disease of the somatosensory system.
Possible neuropathic pain indicates that the condition is not confirmed and requires further investigation.
Probable neuropathic pain
Requires (i) and (ii) with one of the following two clinical confirmatory tests being positive:
- iii. Negative or positive sensory signs confined to the innervation territory of the lesioned nervous structure (according to qualitative or quantitative sensory tests).
- iv.
Diagnostic tests confirming lesion or disease explaining neuropathic pain (imaging, biopsy, neurophysiological, or laboratory tests).
Definite neuropathic pain
Requires (i) and (ii) with both clinical confirmatory tests (iii) and (iv) positive.
If a patient does not meet the criteria for any of these three levels, it is unlikely that the patient has neuropathic pain.
Figure 1.1 provides recommendations for which classification to use for orofacial pain/TMD. In summary, it is best to use the DC/TMD for the most common types of TMDs. For less common TMDs, use the expanded taxonomy of the DC/TMD. And finally, for other orofacial pain conditions, consult the classifications published by the International Association for the Study of Pain or the International Headache Society (Headache Classification Committee of the International Headache Society (IHS), 2013).
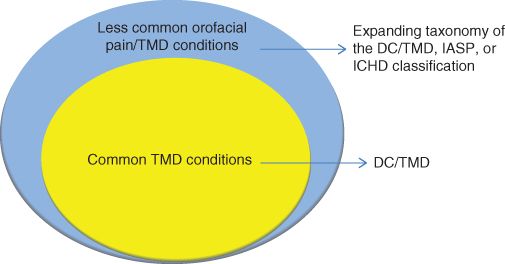
Figure 1.1 Orofacial pain and TMD conditions and the application of different diagnostic classifications.
Clinical Assessment for the Most Common Temporomandibular Disorders/Orofacial Pain Conditions
It is necessary to conduct an interview to collect a comprehensive history in order to guide the clinician to make a relevant and accurate examination and provide a diagnosis, prognosis, and treatment plan for the patient. The following three steps have been recommended to simplify the clinical assessment of patients: (i) screening of all patients at general dental clinics or by other care providers to identify patients with possible orofacial pain/TMD, (ii) a brief and focused examination by the general dentist of patients identified in the screening, and (iii) a comprehensive examination by a specialist.
Since the following chapters in this book are based on diagnoses within the expanded taxonomy of DC/TMD, the focus of this chapter is to help explain the steps leading to a diagnosis. It will provide an overview of how to establish an Axis I diagnosis (physical diagnosis) and an Axis II evaluation of psychosocial distress in orofacial pain/TMD patients.
Readers who seek more detailed information on history data collection, clinical procedures, and laboratory tests in the examination of orofacial pain patients should refer to the Schiffman et al. (2014), Svensson et al. (2014), Goulet et al. (2014), and Ohrbach et al. (2014, 2015).
Screening
Screening instruments can help simplify identification of patients with TMD and orofacial pain (Nilsson et al., 2006; Gonzalez et al., 2011; Zhao et al., 2011). One of these instruments consists of a questionnaire with a long version (six items) and a shorter version (three items) to detect individuals with TMD pain (Gonzalez et al., 2011) (Table 1.2). The long version of this instrument is also integrated into the Symptom Questionnaire of the DC/TMD. All the screening instruments demonstrate good reliability and validity (Nilsson et al., 2006; Gonzalez et al., 2011; Zhao et al., 2011), and have been used in epidemiological studies (Nilsson et al., 2006).
Table 1.2 Screening questions for TMD
A positive score of 2 or more indicates a high probability of pain-related TMD. |
There are several screening instruments developed to detect neuropathic pain (Mathieson et al., 2015). They are most likely useful for trigeminal neuropathic pains, but none have been validated for these conditions yet.
Screening questionnaires are an important first step in detecting patients with TMD pain in the general practice, but they do not replace the need for a physical examination.
Clinical examination
Axis I diagnostics require a patient history including questionnaires and a structured clinical examination that is described below. Assessment of the patient’s psychosocial situation and pain consequences are based on validated instruments (questionnaires), which are described under Axis II below. The DC/TMD distinguishes two levels of inquiry in assessing the patient. The first level is designed for the general practitioner using a brief questionnaire, and the second, more advanced, level uses a more comprehensive questionnaire and is designed for the specialist. At either level it is important to evaluate both clinical status and psychosocial factors in order to get as complete a picture of the patient, given the level of assessment, when making a diagnosis, determining the best therapy, or deciding upon possible referral. Table 1.3 illustrates this through two cases. Since most patients presenting in a dental setting with a facial pain complaint will have a common TMD, we will explain the standardized protocol leading to a diagnosis and psychosocial assessment of the patient with a TMD (DC/TMD).
| Anna | Cecilia | |
| Case history | Anna is a 19-year-old girl with frequent headaches and pain in the jaw and ear region. The pain is recurrent and greater in the morning. She has been examined by her physician and her ENT status is normal. Her physician asked her to be examined by her dentist to see if the pain could be related to orofacial pain. | Cecilia is 51 years old and has had pain for 8 years in the face, head, neck, back and arms. The average pain intensity is NRS 5. The pain started after a neck trauma. She previously received several treatments (e.g., occlusal appliance, instructions in jaw exercises, and occlusal grinding) with limited improvement. She is listless and appears to be slightly depressed. |
| Diagnosis (Axis I) | Myalgia Arthralgia |
Myalgia Arthralgia |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


