As described in the introductory chapters, the term “molar incisor hypomineralization” (MIH) has existed since 2001. It is defined as hypomineralization of systemic origin affecting one or more first permanent molars and may be associated with the involvement of the permanent incisors.1 A review of the literature shows that even before MIH was first described in the early 2000s, standardized recording criteria were used to diagnose the occurrence of enamel defects in teeth. These criteria were initially also applied to MIH, but then turned out to be partially impractical. As a consequence, MIH-specific diagnostic criteria and classification systems have been developed in recent years. In the following sections, this development will be examined and discussed in more detail.
6.1 Diagnostics
6.1.1 Modified DDE index
In the early years of research of MIH, the modified DDE index (Index of Developmental Defects of Dental Enamel)2,3 was used in many prevalence studies. This index gives information on the type of defect, possible combinations, and the extent (Table 6-1). In this context, demarcated opacities, diffuse opacities, hypoplasia, or combinations can be distinguished.
Table 6-1 Modified DDE Index (FDI 1992)2
|
Type |
Defect |
Code |
|
Normal |
0 |
|
|
Demarcated opacity |
White/cream |
1 |
|
Yellow/brown |
2 |
|
|
Diffuse opacity |
Diffuse lines |
3 |
|
Diffuse patchy |
4 |
|
|
Diffuse confluent |
5 |
|
|
Confluent / patchy + staining + loss of enamel |
6 |
|
|
Hypoplasia |
Pits |
7 |
|
Missing enamel |
8 |
|
|
Any other defects |
9 |
|
|
Combinations |
Demarcated + diffuse |
K |
|
Demarcated + hypoplasia |
L |
|
|
Diffuse + hypoplasia |
M |
|
|
All three defects |
N |
|
|
Extent of defect |
Normal |
0 |
|
< 1/3 |
1 |
|
|
At least 1/3 < 2/3 |
2 |
|
|
At least 2/3 |
3 |
- Opacities are defined as a change in the translucency of the enamel. The defective enamel has a normal thickness and a smooth surface when the tooth erupts. Affected areas may be white, cream, yellow, or brown. Some of these enamel defects preserve their translucent surface, whereas others may become more opaque in appearance and can lead to more severe damage and even enamel loss.
- Demarcated opacities show an easily recognizable and clear demarcation to the adjacent, healthy enamel.
- Diffuse opacities do not show such an obvious demarcation and may appear linear, patchy, or diffuse confluent. They always appear in a white color.
- The possibility of hypoplasia mentioned in the index is characterized by reduced enamel thickness. The surface involved and the margins of the macroscopic defects are smooth and mostly regular.
However, for use in epidemiological MIH studies, this index was considered unsatisfactory and still too time-consuming. The lack of detection of posteruptive breakdowns, which can occur in MIH defects, and the possibility of atypical restoration or extraction were criticized.
6.1.2 Enamel Defect Index (EDI)
An alternative and widely used index, the EDI,4 also failed to establish itself for use in MIH studies. The EDI is assessed in three stages. Level 1 characterizes the defect type (opacity, hypoplasia, or posteruptive breakdown), level 2 describes more detailed subcategories of each of the three major categories allowing more detailed investigations when required, and level 3 scores each category independently as being absent or present. A positive aspect of the application is the extended registration of an enamel breakdown, which is a known characteristic of MIH and is identified as missing in the modified DDE described above. However, the problem with a possible application in MIH lies can be found in the description of the defect type of opacity. The index does not distinguish between demarcated and diffuse opacities. This is problematic in so far that in epidemiological studies there would theoretically be a risk of mixing demarcated opacities typical for MIH with diffuse opacities (which may be caused, for example, by high fluoride intake).
Another critical point of discussion is that the EDI index excludes all tooth surfaces affected by caries and large restorations. However, as will be explained in Chapter 16, hypomineralized molars may already become carious in young patients under certain circumstances (eg, due to poor oral hygiene and/or massive hypersensitivities) or may already be restored.
6.1.3 European Academy of Paediatric Dentistry (EAPD) criteria
The lack of suitability of the two indices mentioned above, which are still valid, resulted in an international group of experts meeting in Athens in 2003 to establish, among other things, criteria for the assessment of MIH.5 These are still internationally accepted today and are also widely used.
It is recommended that the child be examined around the age of 8, since at this age all four permanent first molars and the majority of permanent incisors have usually erupted.5 If needed, cotton-rolls may be used to clean tooth surface before to better visualize the teeth. Then, teeth should be examined wet. The first permanent molars and the permanent incisors are examined with regard to the following criteria5–7:
- Absence or presence of clearly demarcated opacities
- Post-eruptive enamel breakdown
- Atypical restorations
- Extractions of molars due to MIH
- Failure of eruption of a molar or an incisor.
Table 6-2 summarizes the diagnostic criteria and their description. Figures 6-1 to 6-4 illustrate these characteristics.
Table 6-2 Assessment criteria for the diagnosis of MIH according to Weerheijm et al1,5
|
Feature |
Description |
|
Demarcated opacity |
|
|
Posteruptive breakdown |
|
|
Atypical restoration |
|
|
Extraction of molars due to MIH |
|
|
Failure of eruption of a molar or an incisor |
|
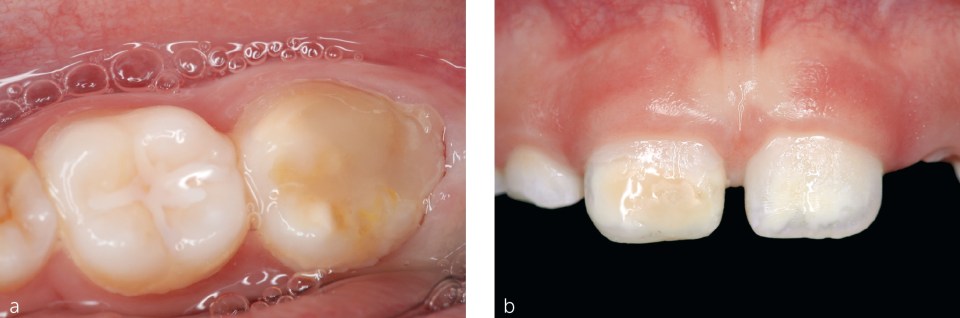
Fig 6-1 EAPD criterion “opacity.” a) Opacity on one molar. b) Opacities on two maxillary central incisors.
Fig 6-2 EAPD criterion “Posteruptive enamel breakdown.” a) Enamel breakdown of a molar. b) Enamel breakdown of tooth 21.
Fig 6-3 EAPD criterion “Atypical restoration.” a) Atypical restoration due to MIH with a posteruptive enamel breakdown of a molar. b) Atypical restoration due to MIH with a posteruptive enamel breakdown of tooth 11.
Fig 6-4 EAPD criterion “Extraction due to MIH.” a) Upper view of the patient from Figure 6-2b. The MIH molars were extracted. b) View of the mandibular jaw of the patient from Figure 6-2b. The mandibular MIH molars were also extracted. Teeth 43 and 44 are already in situ, tooth 33 is erupting.
In terms of differential diagnosis, various clinical presentations must be considered, which are explained in more detail in Chapter 7. These include hereditary anomalies of the tooth structure (amelogenesis imperfecta), postnatal developmental disorders (dental fluorosis, enamel defects due to tetracycline administration), and exogenous anomalies of the tooth structure (trauma, apical inflammation of the deciduous teeth [Turner tooth], caries).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses