This article reviews the current methods for detection and assessment of caries lesions focusing on applicability for daily clinical practice. The end point is to arrive at a diagnosis for each caries lesion. Visual inspection aided by a ball-ended probe is essential for caries lesions assessment and the method must be used for all patients. Use of indices, for example, the International Caries Detection and Assessment System (ICDAS), can improve the performance of this method. Using visual inspection, the clinician must decide about the presence, severity and activity of lesions. After this process, additional methods could aid the dentist in reaching a more appropriate treatment decision in some cases. The ICDAS, including the activity assessment system or the Nyvad system, seems to be the best option to reach final diagnoses for managing lesions. The radiographic method is the most recommended additional method available for daily clinical practice.
The word diagnosis (plural, diagnoses) is derived from the Greek “dia” meaning “through” and “gnosis” meaning “knowledge”. Thus, “to diagnose” implies that it is only through knowledge about the disease that a diagnosis can be established. Diagnosis can be a complicated process.
Caries disease diagnosis is not the classical hypothetical-deductive process that diagnosis often is in the medical world. When a patient visits a doctor, the patient tells his or her symptoms to the doctor. The doctor examines the patient and based on his diagnostic hypotheses (knowledge), the doctor chooses the diagnosis that best fits the patient’s signs and symptoms and the treatment that offers the best prognosis for the patient. This systematic approach permits thinking about all the possibilities available to solve the patient’s problem. Dentists, on the other hand, usually examine their patients thinking about how they will treat the patients’ teeth, rather than thinking about the condition (diagnoses) of the patients’ teeth. Thus, a great deal of information relevant to disease diagnosis can be lost and some treatment options (usually more conservative alternatives) can be underestimated during the final clinical decision making.
The examination and evaluation of carious lesions has traditionally been limited to physical criteria such as size, depth, and presence or absence of cavitation. The term for this is caries lesion detection. Caries lesion activity assessment is different from caries lesion detection. The assessment of lesion activity is, together with lesion detection, essential to arrive at the disease diagnosis and the appropriate clinical treatment decision. In addition to caries lesion detection, lesion or disease activity assessment must also consider etiologic factor evaluations, such as oral hygiene, count of cariogenic micro-organisms in plaque and saliva, use of fluoride, sugar intake, and also some socioeconomic aspects, such as family income and parents’ level of education. It becomes evident that caries disease diagnosis is a difficult task. This article focuses on caries lesion detection including evaluation of caries lesion severity. The authors explore conventional and advanced/modern methods of caries lesion detection, their properties, limitations, and indications. They discuss the interpretation of the results obtained by these methods. Finally, parameters to be used for assessing lesion activity in order to reach a final caries disease diagnosis and relate the treatment decision to this diagnosis are discussed. As caries risk assessment is covered in another article (see the article by Young and Featherstone elsewhere in this issue), the focus of attention in this article is on caries lesions (signs) and the related treatment decisions.
Visual inspection
Visual examination is the most commonly used method for detecting caries lesions, because it is an easy technique that is routinely performed in clinical practice. Visual examination has presented high specificity (proportion of sound sites correctly identified), but low sensitivity (proportion of carious sites correctly identified), and low reproducibility ; the latter because of its subjective nature.
The use of detailed visual indices, however, may improve sensitivity and be an important factor in minimizing the examiner’s interpretation of the clinical characteristics of a lesion, and thus improve reproducibility. Such indices may also describe the characteristics of all clinically relevant stages in the caries disease process, making them a cost-effective method of recording caries lesions. The use of indices has permitted early caries signs to be detected and recorded in a reliable and accurate way in visual examination. However, initial caries lesion stages have generated most of the disagreements between examiners in several studies, and their evaluation demands more training and more time for examination.
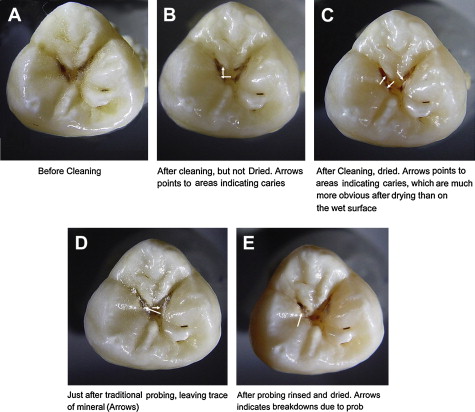
A review found 29 different visual criteria for detecting caries lesions. Each system has its own particularities and methodology of teeth/surface evaluation. Only about half of the technologies recommend teeth to be cleaned and/or dried before the examination process (14 criteria), which if not included will increase the risk of missing lesions ( Fig. 1 ). Further, caries lesion activity assessment is not considered by most of these indices, which is a limitation in clinical practice. In addition, some indices recommend tactile examination to be performed in conjunction with visual examination, and this has been considered questionable. Probing-related surface defects, enlargements, and damage to dental surfaces have been observed on surfaces with initial carious lesions (see Fig. 1 D and E). Some previous reviews have shown inconclusive results with regard to tactile examination performance, and a lack of information concerning the examiner’s training and manner of using the explorer (to remove plaque, to gently probe). The most recent trend is the use of the probe to evaluate enamel surface texture (smooth or rough for enamel lesions; hard or soft dentine for dentinal lesions). Another recommendation is evaluation of the presence of discontinuities in enamel or microcavitations by using the WHO probe, which is ball-ended with a sphere presenting 0.5 mm in the extremity, allowing this kind of evaluation.
In an attempt to propose an internationally accepted caries detection system, a new index for caries diagnosis, the International and Caries Detection Assessment System, was created in 2002 by a group of cariologists and epidemiologists, based on visual examination aided by a WHO probe. The short name of this system is ICDAS. This system is a modification of a previous visually ranked caries lesion scoring system that has been shown to detect occlusal lesions in permanent teeth and to assess their depth with acceptable accuracy and reproducibility.
ICDAS is a 2-digit identification system (X-Y). Firstly, the status of the surfaces is recorded as unrestored, sealed, restored, or crowned. After that, a second code is attributed (Y). This code ranges from measurement of first visual changes in the enamel to extensive cavitation. The description and examples of each code are presented in Fig. 2 . Before examination, teeth have to be carefully cleaned and examinations must be performed with light illumination, an air syringe, plane buccal mirror and, if necessary, a WHO periodontal probe.
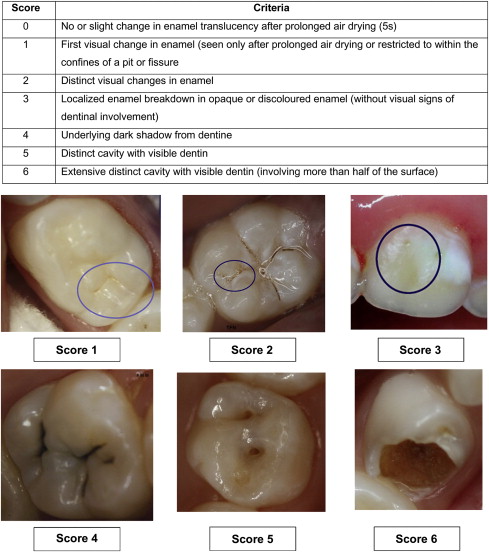
The validity of ICDAS has been tested and expressed in many ways. For example, ICDAS has presented content validity (the system is comprehensible for describing and measuring different degrees of severity of caries lesions). Further, a significant correlation with lesion depth in the histologic examination has been shown. Criterion validity of ICDAS, which means how well the system is correlated with the actual severity of the caries lesions, was also observed in vitro for permanent and primary teeth. Its performance has varied from moderate to good. In terms of figures, the sensitivity for occlusal surfaces have varied from 0.63 to 0.82 and specificity from 0.63 to 0.94.
In primary teeth, ICDAS cannot distinguish accurately between lesions related to the outer or inner half of the enamel ; this can be done fairly accurately in permanent teeth. One explanation for this difference in performance is that the enamel in primary teeth is much thinner compared with permanent enamel.
Few studies have been performed in proximal surfaces using ICDAS. In general, the interexaminer reproducibility has been similar to that observed for occlusal surfaces. The system has presented good performance (high sensitivity and specificity) for in vitro conditions. However, its sensitivity has been low for proximal caries in vivo, whereas the specificity has been high, even when considering the noncavitated threshold. These properties should encourage the use of ICDAS also in proximal caries detection, although other additional methods should be added to improve sensitivity on these surfaces.
Initially, ICDAS was devised as a detection system for primary caries. Adjunct criteria have recently been devised for activity assessment. Thus, the system can be used for caries lesion activity assessment (LAA) also. The LAA is based on the combined knowledge of clinical appearance (ICDAS) of the lesion, whether or not the lesion is in a plaque stagnation area, and the tactile sensation when a ball-ended WHO probe is gently drawn across the surface of the tooth. Such criteria related to activity receive an individual score (points) based on predictive value in determining activity status, and the sum of these points is judged based on a cut-off point ( Table 1 ). These individual criteria have presented moderate to good intra- and interexaminer reproducibility values, as well as good reproducibility results for the system overall. This system also presented construct validity (ie, the system is able to reflect theoretical concepts regarding the caries process).
| Criterion | Description | Activity Score |
|---|---|---|
| Clinical parameter 1 (Visual appearance: severity score) | ||
| ICDAS score 1, 2 (brown lesions) | 1 | |
| ICDAS score 1, 2 (white lesions) | 3 | |
| ICDAS score 3, 4, 5, or 6 | 4 | |
| Clinical parameter 2 (Plaque stagnation) | ||
| Plaque stagnation area (PSA) | Plaque stagnation area (PSA) along the gingival, below or above the contact area on proximal surfaces, entrance to the pits and fissures and cavities with irregular borders | 3 |
| Non plaque stagnation area (non-PSA) | Flat pits and fissures | 1 |
| Clinical parameter 3 (Surface texture) | ||
| Rough or soft surface on gentle probing | 4 | |
| Smooth or hard surface on gentle probing | 2 | |
Two studies have already used the ICDAS+LAA system in caries activity assessment. One of these studies concluded that areas of plaque stagnation were more associated with caries lesion activity status than surface texture. The other study used the system successfully to verify an association between caries lesion activity and some biologic parameters. Results have suggested that the use of this system could overestimate caries lesion activity status for primary teeth, because cavitated lesions invariably would be considered active, which is not certain in all cases. However, validity parameters could be improved if new cut-off points were adopted. New studies should be encouraged to reevaluate the importance attributed to each clinical parameter or to revise the cut-off point used to classify caries lesion activity in primary teeth.
Using the ICDAS in combination with the LAA criteria described here, it is possible to detect a lesion, estimate its depth or severity, and assess its activity, which are all fundamental prerequisites for the diagnosis and management of the individual lesion.
Nyvad’s System
Nyvad’s system ( Table 2 ) is another reliable option for activity assessment of noncavitated and cavitated caries lesions. This system has presented construct and predictive validity (the different status of caries lesions can be predictive of different outcomes) concerning caries lesion activity status. According to this system, a score can be attributed to all observed characteristics of the lesion, eventually classifying the lesion as inactive or active. If a lesion presents at least 1 feature compatible to an active lesion, the examiner should classify the lesion as active. The original system used plaque as an indicator for caries lesion activity and used standard probes to assess roughness. Some recent studies have performed examinations using Nyvad’s scoring criteria exactly as published. However, to standardize the methodology used in the examinations, the Nyvad system was modified in several ways compared with the original version, adopting inspection after prophylaxis and the use of the WHO probe.
| Score | Category | Criteria |
|---|---|---|
| 0 | Sound | Normal enamel translucency and texture (slight staining allowed in otherwise sound fissure) |
| 1 | Active caries (intact surface) | Surface of enamel is whitish/yellowish, opaque with loss of luster; feels rough when the tip of the probe is moved gently across the surface; generally covered with plaque. No clinically detectable loss of substance. Intact fissure morphology; lesion extending along the walls of the fissure |
| 2 | Active caries (surface discontinuity) | Same criteria as score 1. Localized surface defect (microcavity) in enamel only. No undermined enamel or softened floor detectable with the explorer |
| Active caries (cavity) | Enamel/dentine cavity easily visible with the naked eye; surface of the cavity feels soft or leathery on gentle probing. There may or may not be pulpal involvement | |
| 4 | Inactive caries (intact surface) | Surface of enamel is whitish, brownish, or black. Enamel may be shiny and feel hard and smooth when the tip of the probe is moved gently across the surface. No clinically detectable loss of substance. Intact fissure morphology; lesion extending along the walls of the fissure |
| 5 | Inactive caries (surface discontinuity) | Same criteria as score 4. Localized surface defect (microcavity) in enamel only. No undermined enamel or softened floor detectable with the explorer |
| 6 | Inactive caries (cavity) | Enamel/dentine cavity easily visible with the naked eye; surface of the cavity feels shiny and feels hard on gentle probing. No pulpal involvement |
| 7 | Filling (sound surface) | |
| 8 | Filling + active caries | Caries lesion may be cavitated or noncavitated |
| 9 | Filling + inactive caries | Caries lesion may be cavitated or noncavitated |
Although it was not its original purpose, the Nyvad index worked well in assessing the depth of lesions on primary teeth. As observed for ICDAS, microcavities, that is, cavitation limited to enamel (scores 2 and 5 in the Nyvad system, score 3 in ICDAS), usually involve dentin demineralization in primary teeth.
It is inherent that visual examination must be the main method for caries detection, whereas the methods described below tend to act as adjuncts, depending on the purpose of the examination. It is worth emphasizing that visual examination is the only effective method available to assess caries lesion activity. The use of the indices to assess caries lesion activity described in this article ,should be considered in daily clinical practice.
Additional methods to detect caries lesions
Radiographic Methods
In permanent teeth, sensitivity values of visual examination obtained in clinical studies in detecting proximal caries lesions have been around 0.30. A study by Novaes and colleagues obtained similar figures in detecting cavitated lesions in the proximal surfaces of primary molars. Therefore, around 70% of cavitated caries lesions would be missed using visual inspection.
The use of a bitewing radiography as an adjunct to the clinical examination could permit more sensitive detection of proximal and occlusal caries lesions in dentin and a better estimation of the lesion depth than the visual inspection performed alone. Moreover, the monitoring of caries lesions could be more reliable and accurate than using the conventional clinical examination alone.
Bitewing projection is the most appropriate radiographic technique for caries detection. This technique requires a film-holder with a wing for the patient to bite. A good technique is necessary to avoid overlapping surfaces, cone cuts, and missing surfaces. In such conditions, the bitewing radiographs provide valuable information to complete the clinical diagnosis.
Some disadvantages, however, are present and must be considered when making treatment decisions, mainly on proximal surfaces. First, radiographic images underestimate the actual lesion depth (measured histologically), and are unable to show accurately the early stages of enamel caries lesions. Furthermore, this method is technique-sensitive and unavoidably exposes the patient to the hazards of ionizing radiation. Another factor is that radiographs do not indicate caries lesion activity and they are not able to detect the presence of cavitations (cavities), which is an important point in making a decision about treatment, mainly regarding proximal surfaces. Nevertheless, the risk-benefit ratio of radiographic examination as an additional method for caries detection justifies its use and is now discussed in more detail.
The bitewing method can aid the dentist in reaching an appropriate decision in both occlusal and proximal surfaces. In fact, in occlusal surfaces, if a tooth presents an ICDAS score of 0, 1, or 2, a radiograph is not necessary in most cases. If a site is classified as score 5 or 6 by visual inspection, a bitewing radiograph is not necessary to aid detection (periapical radiography can be indicated to check the proximity of the caries lesion to the pulp and to evaluate the condition of the periapical tissues). However, if the clinician scores the teeth as 3 or 4 in an occlusal site, a radiograph could be used to confirm the detection and to help in clinical decision making (nonsurgical or surgical treatment). Detection of caries lesions not detected by clinical examination, mainly early dentin caries lesions, favors the use of radiographic examination because the method has presented high sensitivity in detecting dentinal caries lesions. Missed advanced dentin caries lesions could cause some discomfort for patients until the subsequent appointment, whereas nondetected enamel caries lesions do not pose any problem for the patient. Thus the radiographic method is beneficial, despite poor performance in detecting enamel caries lesions.
On occlusal surfaces, the radiographic method has been useful in detecting caries lesions not detected by visual inspection. These lesions have been termed hidden caries lesions. However, it is mostly acknowledged that if a thorough clinical examination on cleaned and dried teeth has been done, “hidden” caries do not exist.
For proximal surfaces, the benefits of radiographs are more evident. Teeth with an intact marginal ridge, and sound to visual examination, can have both enamel caries lesions and dentine caries lesions. In this instance, the presence of cavitation drives the decision to surgically restore rather than study the histologic lesion depth. In 1992, Pitts and Rimmer correlated bitewing radiography with cavitation. Pitts and Rimmer demonstrated that when the radiographic image shows radiolucency restricted to the enamel, the caries lesion is usually noncavitated. Therefore, the dentist should opt for nonsurgical treatment if the lesion is active; for example, as judged by gingival status. If the lesion reaches the internal half of dentin in the radiographic image, probably this lesion will present a cavitation. Thus, surgical treatment is the best choice. However, when the radiographic image is an initial dentin caries lesion at the proximal surface, some caries lesions will present cavitation; but many of these surfaces will not have cavitation. In these cases, therefore, the clinician could provide the temporary separation of the tooth with orthodontic rubbers, to check if the surface is cavitated and determine the correct treatment decision. More common is the decision to plan for a new examination including a radiograph a year later, to monitor the progression and success of nonsurgical interventions.
Another possibility is digital radiography. In this technique, a digital sensor is used instead of conventional film and the radiographic image is stored in a computer. Digital radiographs usually expose patients to lower radiation doses than conventional methods. Digital radiographs permit the use of computer facilities, such as the possibilities of image enhancement and processing of the images, and of sending the images to other colleagues. In general, conventional radiographic methods have presented sensitivity values around 0.50 to 0.60 and specificity values usually higher than 0.90 in detecting proximal caries lesions in primary and permanent teeth.
For occlusal surfaces, the sensitivity values of conventional radiography have been between 0.50 and 0.80, and specificities around 0.80. Digital methods have performed similarly.
Novel tools, however, have been created for digital radiographic images to improve the process of caries detection or monitoring. Methods of digital subtraction can be used in 2 radiographic images of the same site recorded in different periods. This method would allow for monitoring caries lesion progression, because the 2 radiographs are taken with partly controlled projection angles. Computed tomography techniques have been recommended for caries detection and seems a promising tool for this issue, but further studies are necessary to check the performance and real benefits of the method.
In the use of the radiographic method as an adjunct of clinical examination in detecting caries, one can summarize that the conventional bitewing image can aid the dentist in reaching a treatment decision, mainly on proximal surfaces or occlusal sites scored as 3 or 4 by the ICDAS (see Fig. 2 ). Digital radiography has not presented a better performance, but the method exposes the patients to lower doses of ionizing radiation and could offer some assistance to the clinician.
Fiber Optic Transillumination
When a tooth is illuminated by a light, the carious tissue, because of the porosity, scatters the light and the enamel shows as a whiter, opaque area in visual inspection. Likewise, when the dentin is involved in the caries process, a shadow is observed in the underlying dentin. This phenomenon is observed in lesions classified as score 4 of the ICDAS.
The fiber optic transillumination (FOTI) method uses a high-intensity white light to enhance these effects. Thus, carious enamel and dentin appear as shadows with the use of the FOTI method. The method is more appropriate for proximal surfaces but can be used for all surfaces. The device usually is portable and easy to use, but it is not quantitative and the diagnostic and treatment decisions depend on the dentist’s interpretation. Therefore, low-reliability values are expected. A digital version of the technique, named digital fiber optic transillumination (DIFOTI), has been introduced, whereby the device records the images on a computer. These images can be archived and assessed in recalls. This property could permit monitoring of surface demineralizations, but this use of DIFOTI has not been tested as yet. One important property of DIFOTI is worth mentioning. Because the CCD camera takes an image of the surface only, it shows demineralization and does not correlate with cavitation; therefore, it should not be interpreted in the same manner as a bitewing radiograph.
With regard to the performance of the FOTI method in detecting caries lesions, several studies have presented high specificities but low sensitivities for both occlusal and proximal surfaces. The method does not use ionizing radiation. However, apart from this advantage, FOTI or DIFOTI methods have not presented more benefits than visual or radiographic methods.
Electronic Caries Monitor
The electronic caries monitor (ECM) device uses alternating current and measures the bulk resistance of tooth tissue. The porosity of caries lesions is filled with fluids with high concentration of ions from the oral environment, and this more porous tissue decreases electrical resistance or impedance more than the sound dental tissue. ECM is able to detect and quantify this difference.
The method presents a probe that is directly applied in an occlusal site, and the device shows a number that translates the electrical resistance of the site. Higher numbers indicate deeper caries lesions. As the method is quantitative, high-reproducibility values would be expected. Nevertheless, only fair reliability has been reported, probably due to technical problems. With regard to validity, higher sensitivity values (around 0.90) have been obtained compared with conventional methods, in detecting occlusal dentin caries lesions. However, lower specificity values (around 0.80) have been observed. The decision about the activity status of the tooth should not be made using ECM alone, but the method could be useful as an adjunct to visual inspection. For use in daily clinical practice, however, the method has not presented advantages compared with conventional methods. Further, the method cannot yet be applied to proximal surfaces.
Fluorescence-Based Methods
The knowledge that the presence of a caries lesion provokes changes in the fluorescence properties of dental tissues has allowed the development of several fluorescence-based methods for detection and quantification of caries lesions. The first fluorescence-based method introduced onto the market was quantitative light-induced fluorescence (QLF). A QLF device uses a high-intensity halogen lamp, which emits a blue light (λ = 370 nm) to excite the tooth. When exposed to a light with this wavelength, dental tissues emit a fluorescence (in green spectrum), which is detected by the system, and the image is recorded in a computer. Mineral loss in this tooth causes a decrease in the fluorescence. This fluorescence reduction is analyzed by computer software and the mineral loss is quantified.
The QLF method permits early detection of enamel demineralization (earlier than other methods). Furthermore, this method has presented a strong correlation with mineral loss of enamel caries lesions assessed by gold standard analytical methods (microradiography, for instance). Because of this property associated with high reliability values and a video repositioning software, which facilitates the acquisition of identical images on different occasions, the device is an excellent method for monitoring enamel caries lesions to assess whether preventive measures are able to arrest or remineralize the lesion. Some clinical studies have used the QLF method to measure the effectiveness of preventive measures for initial caries lesions. Nevertheless, the device is recommended more for smooth-surface caries lesions restricted to the enamel. The strong correlation with mineral content of the tooth decreases when the assessments are performed in dentin caries lesions.
The method has been also tested in detecting occlusal caries lesions. However, the results have been disappointing, with low values of specificity (0.11–0.55) and sensitivity (0.64–0.96), according to the different cut-off points used. Furthermore, acquisition of images from occlusal surfaces have been time consuming in the clinical setting.
Another fluorescence-based method consists of a diode laser fluorescence device (LF), named DIAGNOdent (KaVo, Charlotte, NC). With the LF method, a diode laser emits a red light (λ = 655 nm), which is absorbed by bacterial by-products such as porphyrins. This light is partially reemitted as near-infrared fluorescence. The device captures this fluorescence and translates it on a numerical scale from 0 to 99: the higher the number, the deeper the caries lesions.
The first version of the LF device (DIAGNOdent) was designed for the detection of caries lesions in occlusal and smooth surfaces. For this purpose, the method has been extensively studied and has demonstrated the high reliability of the device in detecting occlusal caries lesions and a moderate correlation with mineral loss in smooth-surface caries lesions.
With regard to validity, studies have demonstrated good sensitivity and specificity values, but the magnitudes of these values have been variable due to different cut-off points used in the different studies. Another possible explanation for the high variability found in these studies could be due to several possible factors that can alter the LF readings. The drying time of the site before the LF assessment, presence of plaque or pigmentation, and some toothpastes or prophylaxis pastes are possible factors that influence the LF readings.
The sensitivity values for detection of occlusal caries lesions have been higher than the specificities, and the values have been usually described between 0.80 and 0.90. The specificity values obtained in different studies have been between 0.60 and 0.70. These results, therefore, indicate that the device could be used as an adjunct to visual inspection, and could be an alternative for radiography. However, the older version of the device is not designed for proximal caries detection, and thus a radiograph would be necessary to check the proximal surfaces.
Due to this limitation, a new version of the method was designed and introduced, named DIAGNOdent pen (LFpen). This new version permits the assessment of both occlusal and proximal surfaces. The device works on the principles of the old version, but the design is different. The tip is rotatable around the axis of its length, enabling the operator to assess mesial and distal surfaces from both sides (buccal and lingual). The tip designed for proximal surfaces is made of sapphire fiber with a prismatic shape, and the light is directed laterally to the longitudinal axis of the tip. Another cylindrical tip is recommended for occlusal surfaces, and the direction of its light is perpendicular to the axis of the length of the tip. After excitation, the tip collects the fluorescence and translates it into a numerical scale from 0 to 99.
The LFpen method has been tested for occlusal caries detection but the focus here is on the studies of proximal surfaces. Some studies have demonstrated a slight superiority of the new device in detecting proximal caries lesions in the in vitro setting. Other studies, however, have observed that the device has performed similarly to radiographic methods in detecting cavitated proximal lesions in primary molars. In these studies, sensitivities were around 0.60 and the specificities were almost 1.0.
The LFpen device could be an alternative to the radiographic method to aid the dentist in the decision-making process after visual inspection. Nevertheless, the evidence concerning the use of the method in clinical practice is limited, and further studies are necessary to evaluate whether the method could be useful.
Summarizing the discussion about ECM and fluorescence-based methods, higher reproducibility values and the possibility of monitoring caries lesions could be expected due to the quantitative nature of these methods. However, these methods have shortcomings, for example, lack of LAA, which do not justify use in daily clinical practice without including the conventional visual inspection and bitewing radiography.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


