Studies have shown a growing trend toward increasing prevalence of dental erosion, associated with the declining prevalence of caries disease in industrialized countries. Erosion is an irreversible chemical process that results in tooth substance loss and leaves teeth susceptible to damage as a result of wear over the course of an individual’s lifetime. Therefore, early diagnosis and adequate prevention are essential to minimize the risk of tooth erosion. Clinical appearance is the most important sign to be used to diagnose erosion. The Basic Erosive Wear Examination (BEWE) is a simple method to fulfill this task. The determination of a variety of risk and protective factors (patient-dependent and nutrition-dependent factors) as well as their interplay are necessary to initiate preventive measures tailored to the individual. When tooth loss caused by erosive wear reaches a certain level, oral rehabilitation becomes necessary.
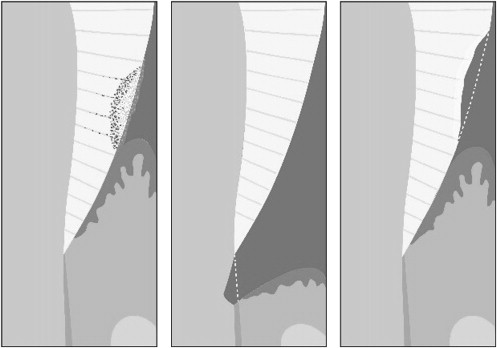
The pattern of oral disease has been influenced by the ever-changing human lifestyle. Tooth wear, especially tooth erosion, has drawn increasing attention as a risk factor for tooth damage or loss. Dental erosion and caries lesions result from acids on tooth structure. The acids causing caries lesions are produced by bacteria in the mouth. The acids that are responsible for tooth erosion, on the other hand, stem from extrinsic (eg, soft drinks, acidic foods) or intrinsic (eg, reflux fluid) sources. Structurally, caries lesions are characterized by a subsurface partial demineralization in which the subsurface lesion body is covered by an intact surface layer ( Fig. 1 , left ). By comparison, tooth erosion is characterized by initial surface softening and subsequent bulk material loss. In the early stage, acids diffuse into the tooth and remove calcium and phosphate ions from the outer few micrometers of hard tissues, forming a demineralized, weakened overlying layer. In the advanced stage, the apatite crystals of the tooth are destroyed and dissolved away layer by layer from the tooth surface, leading to a generalized loss of tooth volume ( Fig. 1 , right ).
There is some evidence that the prevalence of dental erosion is growing. In a study in the United Kingdom, 1308 adolescents of mixed ethnicities were examined at the age of 12 years and then 2 years later. Almost 5% of the subjects at baseline and more than 13% 2 years later had deep enamel or dentin lesions. In this study, approximately 12% of the erosion-free adolescents developed erosive lesions in the following 2 years. The spread of tooth erosion, especially in children, adolescents, and young adults, has been largely linked to the high consumption of acidic drinks and foods. However, it is impossible to avoid potentially erosive agents from contact with the teeth during a lifetime. After applying rehabilitation treatment, restorative materials also exhibit degradation in acids. Therefore, to prevent or inhibit further erosion, the emphasis should be on early diagnosis and adequate preventive strategies. Restorative measures should be taken only when tooth loss caused by erosive wear reaches a certain threshold.
Diagnosis
In the early stages, it is difficult to diagnose erosion, as erosion is associated with few signs and fewer, if any, symptoms such as pain or sensitivity. There is no device available in routine dental practice for the specific detection of dental erosion and its progression. Therefore, clinical appearance has to be applied as the most important feature for dental professionals to diagnose tooth erosion. In the more advanced stages, dentin may become exposed. To determine this condition, disclosing agents can be used to render dentin visible.
The appearance of smooth, silky-glazed, sometimes dull enamel with the absence of perikymata and intact enamel along the gingival margin are some typical signs of enamel erosion. An enamel ridge may persist at the crown margin. The presence of this phenomenon can be explained on the one hand by plaque residues, which can act as a diffusion barrier to acids, and on the other hand by sulcular fluid, which leads to neutralization of the acids in the gingival region. The initial features of erosion on occlusal and incisal surfaces are the same as described earlier. Further progression of occlusal erosion leads to a rounding of the cusps and restorations rising above the level of the adjacent tooth surfaces. In severe cases, the entire occlusal morphology disappears. Extensive loss of enamel can lead to dentin exposure and even lead to pulp exposure in some extreme cases. The exposed surface becomes sensitive to cold and warm foods and to tactile stimuli. To record the progress of the erosion, photographs or models should be taken periodically. Fig. 2 shows the typical pattern of dental erosions.

Erosion has to be distinguished from attrition and abrasion. For the latter, tooth surfaces are often flat, with glossy areas with distinct margins and corresponding features on the antagonistic teeth. It is not always possible to differentiate these wear lesions because they frequently occur simultaneously with different proportional effects. As the tooth enamel layer demineralizes and becomes softened it becomes more susceptible to abrasion and attrition. Facial erosion should be distinguished from wedge-shaped defects, which are located at, or apical to, the enamel-cementum junction, as shown in Fig. 3 . The coronal part of wedge-shaped defects ideally has a sharp margin and cuts at a right angle into the enamel surface, whereas the apical part bottoms out to the root surface. Thereby the depth of the defect exceeds its width. In addition, tooth surfaces of patients with active (unstained) erosion often have no caries lesions. However, caries lesions may occur in patients with erosion at sites where plaque accumulation is possible (eg, approximal; see Fig. 2 ).

The Basic Erosive Wear Examination (BEWE) was introduced to facilitate quantifying the risk of erosion. It can be used with the diagnostic criteria of most current indices and allows reanalysis and integration of results from existing studies. All teeth, except third molars, are examined in each case from the vestibular, occlusal, and palatinal aspects for acid damage. The most severely affected surface in a sextant is recorded with a 4-level score ( Table 1 ). The sum of the scores defines the severity of erosive wear and guides the further management of the condition ( Table 2 ). The maximum score per subject is 18. Management includes identification and elimination of the main causative factor(s), prevention, and monitoring, as well as symptomatic and operative intervention, where appropriate.
| Score | Criteria |
|---|---|
| 0 | No erosive tooth wear |
| 1 | Initial loss of surface texture |
| 2 a | Distinct defect, hard tissue loss <50% of the surface area |
| 3 a | Hard tissue loss ≥50% of the surface area |
| Susceptibility Level | Cumulative Score of All Sextants | Management |
|---|---|---|
| ≤2 | Routine maintenance and observation Repeat at 3-year intervals |
|
| Low | 3–8 | Oral hygiene and dietary assessment and advice. Identify the main causative factor(s) and develop strategies to eliminate their effects, routine maintenance, and observation. Repeat at 1- to 2-year intervals |
| Medium | 9–13 | As above plus Measures to increase the resistance of tooth surfaces Ideally, avoid the placement of restorations and monitor erosive wear with study casts, photographs, or silicone impressions Repeat at 6- to 12-month intervals |
| High | ≥14 | As above plus Especially in cases of severe progression consider special care, which may involve restorations Repeat at 6-month intervals |
Risk factors
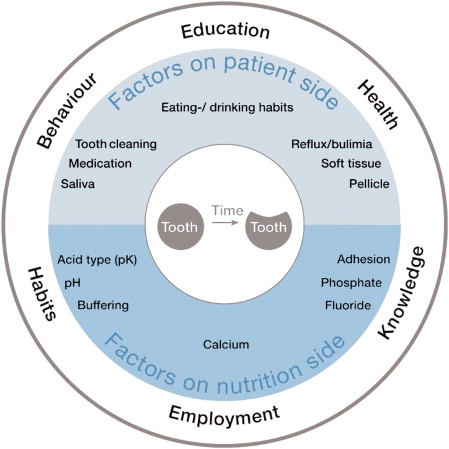
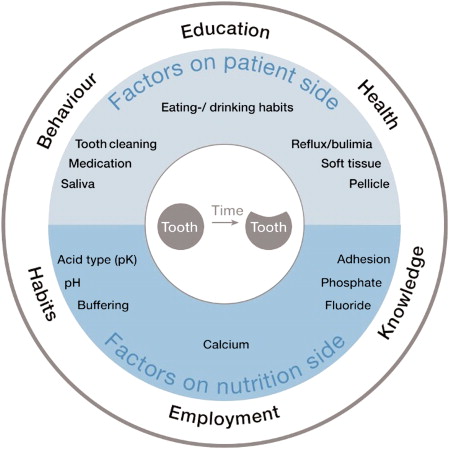
Tooth erosion is a multifactorial condition and has a complex etiology. Various factors involved in the generation and development of erosion may be patient dependent or nutrition dependent ( Fig. 4 ). Every factor plays a more or less important role in inducing or preventing erosion. With time, the interaction of all factors with the tooth surface may either wear tooth hard tissues away or indeed protect them, depending on their fine balance.
Nutritional Factors
Excessive consumption of acidic foods and drinks is regarded as an important factor leading to tooth erosion. In recent years, the total amount and frequency of consumption of acidic foods and drinks has increased as a result of changes in lifestyles. In 2007, the worldwide annual consumption of soft drinks reached 552 billion liters, the equivalent of just less than 83 L per person per year, and this is projected to increase to 95 L per person per year by 2012. However, the figure has already reached an average of 212 L per person per year in the United States in 2009. The erosion potential of a drink or food is codetermined by its chemical and physical properties, such as the pH value, the levels of calcium, phosphate, and to a lesser extent fluoride, and the titratable acidity (buffering capacity), as well as the adhesiveness and displacement of the potentially erosive substances.
The pH value is an important but not the only variable in the erosive potential of drinks and foods. Apart from its pH value, the ability of an acidic solution to dissolve enamel or dentin depends on its ability to keep pH unaffected by the dissolution of tooth mineral and dilution with saliva (ie, its buffering capacity). Buffering capacity is associated with the undissociated acid in drinks and foods. Undissociated acid is not charged and can diffuse into the hard tissues of the teeth and act as a buffer to maintain the H + concentration. Consequently, the driving force for demineralization at the site of dissolution is maintained. This parameter, therefore, may be a good indicator of the erosive potential of a food or drink, especially after exposure for a certain time. The greater the buffering capacity of the drink, the longer it will take for saliva to neutralize the acid and then the more apatite may be dissolved before an higher pH value is reached and dissolution ceases.
The concentration of calcium (Ca), phosphate (P), and fluoride (F) ions in a drink or food also plays a key role in tooth erosion. Combined with the pH value, they determine the degree of saturation with respect to enamel or dentin, which is the driving force for dissolution. Solutions supersaturated with respect to enamel or dentin will not dissolve it. A low degree of undersaturation leads to an initial surface demineralization, which is followed by a local increase in pH and increased mineral ions content in the liquid surface layer adjacent to the tooth surface. This layer then becomes saturated with respect to tooth mineral and does not demineralize the tooth further. Yoghurt is a good example of a food with low pH value (pH ∼4) leading to no erosion. This fact can be attributed to its supersaturation with respect to tooth mineral resulting from the high Ca and P concentration. Modified diets with minerals (eg, Ca, P, or casein phosphopeptide-amorphous calcium phosphate [CPP-ACP]), showed a reduced erosive capacity and therefore were recommended to patients at risk of erosion. However, the addition of minerals to the diet may only retard enamel dissolution, rather than completely prevent its progression.
Common extrinsic dietary acids include citric acid, phosphoric acid, ascorbic acid, malic acid, and carbonic acid. Citric acid is known to exhibit a greater erosive potential than the others. The greater erosive potential of citric acid might be related to its ability to form chelating complexes with Ca and/or high buffering capacity. A study by Meurman and ten Cate (1996) showed that up to 32% of the Ca in saliva could be complexed by citrate at concentrations common in fruit juices, thus reducing the supersaturation of saliva and increasing the driving force for dissolution with respect to tooth mineral. Therefore, acids such as citric acid have a twofold effect and may be very damaging to the tooth surface. The erosive potential of acidic dietary substances may be decreased by replacing highly erosive acids (eg, citric acid) with acids with lower erosive potential.
The adhesiveness and displacement of the liquid are other factors to be considered in the erosive process. There seem to be differences in the ability of beverages to adhere to enamel based on their thermodynamic properties. However, further research is needed to understand this phenomenon better.
Patient Factors
In tooth erosion, risk factors such as lifestyle, oral hygiene habits, and health condition are patient modifiable.
The manner in which dietary acids are introduced into the mouth (sipping, sucking, with/without drinking straw), which determines the duration and the localization of the acid attack, influences the appearance of the erosions. The frequency and duration of acid attacks are also closely associated with erosion and, therefore, very important for the adoption of prophylactic measures. Contact of the teeth with acids during the night can also lead to erosion because of the reduced production of saliva. Thus, for example, apart from cariogenesis there can be massive erosive tooth structure destruction as a result of the consumption of acidic sweet drinks, which some infants drink from their bottles continuously during the night.
Another risk factor on the patient side is stomach acid, which enters the mouth as a consequence of vomiting or reflux. Vomiting is the forceful expulsion of the contents of one’s stomach through the mouth and sometimes the nose. This phenomenon normally results from psychological disorders such as anorexia and bulimia nervosa. Reflux is defined as the involuntary movement of the gastric contents from the stomach into the mouth, caused by some abnormality in the gastrointestinal tract. In general, acidic gastric content entering the mouth may, in time, erode the teeth. Unlike dietary acids, the pH and titratability of gastric juice is significantly greater and so the level of destruction is normally more severe. Because the clinical manifestation of dental erosion does not occur until gastric acid has acted on the dental hard tissues regularly over some time, dental erosion caused by gastric acid has been observed only in those diseases that are associated with chronic vomiting or persistent gastroesophageal reflux, also known as gastroesphageal reflux disease (GERD), over a long period. Intrinsic tooth erosion usually takes place in the region of the occlusal and palatal tooth surfaces of the maxillary teeth. Often the dentist is the first person to detect these diseases and should treat them accordingly.
Saliva is of the essence in the tooth erosion process. Several salivary protective mechanisms come into play during an erosive challenge: dilution and clearance of an erosive agent from the mouth, neutralization and buffering of acids, slowing down the rate of enamel dissolution through the common ion effect by salivary Ca and P, and involvement in the formation of the pellicle. The acquired pellicle is an organic film free of bacteria that covers oral hard and soft tissues. It is composed of mucins, glycoproteins and proteins, including several enzymes. The acquired pellicle may protect against erosion by acting as a diffusion barrier or a selectively permeable membrane preventing direct contact between the acids and the tooth surface, thus reducing the dissolution rate of dental hard tissues.
Practical experience demonstrates the importance of saliva in patients suffering from salivary flow impairment. Studies have shown that erosion may be associated with low salivary flow or low buffering capacity. The dry mouth condition is usually related to aging, even though some other studies have not identified this correlation. It is well established that patients taking medication can also present decreased salivary output, as well as those who have received radiation therapy for head and neck cancer. Tests of the stimulated and unstimulated flow rate, as well as the buffering capacity of saliva may provide some information about the susceptibility of an individual to dental erosion. However, these parameters are only 2 aspects of a multifactorial condition. Sialometric evaluations should be performed at a fixed time point or in a limited time interval in the morning, to avoid intra-individual variation as a result of the circadian cycle. Studies have shown that sour foodstuffs have strong influences on the anticipatory salivary flow, which can be significantly increased compared with the normal unstimulated flow rate. Hypersalivation also occurs in advance of vomiting as a response from the vomiting center of the brain, as frequently seen in individuals suffering from anorexia and bulimia nervosa, rumination, or chronic alcoholism. It is suggested that this could minimize the erosion caused by acids of gastric origin. On the other hand, patients with symptoms of GERD should not expect salivary output to increase before gastric juice reflux, because this is an involuntary response that is not coordinated by the autonomic nervous system. Therefore, there may be insufficient time for saliva to act before erosion occurs.
Millward and colleagues monitored the pH at the surface of teeth in healthy volunteers after drinking 1% citric acid. They observed that the pH recovered to more than pH 5.5 within 2 minutes at a site adjacent to the palatal surface of the upper central incisor and within 4 to 5 minutes at another palatal surface on the upper first molar. Thus, the clearance rate of erosive agents may be influenced by the anatomy of the teeth and soft tissues, by the movement of the tongue and buccal mucosa, as well as by the swallowing pattern. In addition, the mechanical abrasion caused by the tongue was considered to be a contributing factor in erosion.
Apart from the risk factors discussed earlier, occupation and sport may also lead to erosive wear. Employees in the chemical industry or professional wine tasters have a higher risk of suffering erosion as a result of the increased acid-tooth contact. Tooth erosion associated with professional athletes or excessive exercise has also been reported. Excessive exposure to water or sports drinks with low pH, or increased gastroesophageal reflux resulting from strenuous exercise may be responsible for the sport-induced erosion. In the occurrence and development of erosion, occupation and sport can only be considered as cofactors rather than isolated factors, because erosion is a multifactorial condition.
Risk factors
Tooth erosion is a multifactorial condition and has a complex etiology. Various factors involved in the generation and development of erosion may be patient dependent or nutrition dependent ( Fig. 4 ). Every factor plays a more or less important role in inducing or preventing erosion. With time, the interaction of all factors with the tooth surface may either wear tooth hard tissues away or indeed protect them, depending on their fine balance.
Nutritional Factors
Excessive consumption of acidic foods and drinks is regarded as an important factor leading to tooth erosion. In recent years, the total amount and frequency of consumption of acidic foods and drinks has increased as a result of changes in lifestyles. In 2007, the worldwide annual consumption of soft drinks reached 552 billion liters, the equivalent of just less than 83 L per person per year, and this is projected to increase to 95 L per person per year by 2012. However, the figure has already reached an average of 212 L per person per year in the United States in 2009. The erosion potential of a drink or food is codetermined by its chemical and physical properties, such as the pH value, the levels of calcium, phosphate, and to a lesser extent fluoride, and the titratable acidity (buffering capacity), as well as the adhesiveness and displacement of the potentially erosive substances.
The pH value is an important but not the only variable in the erosive potential of drinks and foods. Apart from its pH value, the ability of an acidic solution to dissolve enamel or dentin depends on its ability to keep pH unaffected by the dissolution of tooth mineral and dilution with saliva (ie, its buffering capacity). Buffering capacity is associated with the undissociated acid in drinks and foods. Undissociated acid is not charged and can diffuse into the hard tissues of the teeth and act as a buffer to maintain the H + concentration. Consequently, the driving force for demineralization at the site of dissolution is maintained. This parameter, therefore, may be a good indicator of the erosive potential of a food or drink, especially after exposure for a certain time. The greater the buffering capacity of the drink, the longer it will take for saliva to neutralize the acid and then the more apatite may be dissolved before an higher pH value is reached and dissolution ceases.
The concentration of calcium (Ca), phosphate (P), and fluoride (F) ions in a drink or food also plays a key role in tooth erosion. Combined with the pH value, they determine the degree of saturation with respect to enamel or dentin, which is the driving force for dissolution. Solutions supersaturated with respect to enamel or dentin will not dissolve it. A low degree of undersaturation leads to an initial surface demineralization, which is followed by a local increase in pH and increased mineral ions content in the liquid surface layer adjacent to the tooth surface. This layer then becomes saturated with respect to tooth mineral and does not demineralize the tooth further. Yoghurt is a good example of a food with low pH value (pH ∼4) leading to no erosion. This fact can be attributed to its supersaturation with respect to tooth mineral resulting from the high Ca and P concentration. Modified diets with minerals (eg, Ca, P, or casein phosphopeptide-amorphous calcium phosphate [CPP-ACP]), showed a reduced erosive capacity and therefore were recommended to patients at risk of erosion. However, the addition of minerals to the diet may only retard enamel dissolution, rather than completely prevent its progression.
Common extrinsic dietary acids include citric acid, phosphoric acid, ascorbic acid, malic acid, and carbonic acid. Citric acid is known to exhibit a greater erosive potential than the others. The greater erosive potential of citric acid might be related to its ability to form chelating complexes with Ca and/or high buffering capacity. A study by Meurman and ten Cate (1996) showed that up to 32% of the Ca in saliva could be complexed by citrate at concentrations common in fruit juices, thus reducing the supersaturation of saliva and increasing the driving force for dissolution with respect to tooth mineral. Therefore, acids such as citric acid have a twofold effect and may be very damaging to the tooth surface. The erosive potential of acidic dietary substances may be decreased by replacing highly erosive acids (eg, citric acid) with acids with lower erosive potential.
The adhesiveness and displacement of the liquid are other factors to be considered in the erosive process. There seem to be differences in the ability of beverages to adhere to enamel based on their thermodynamic properties. However, further research is needed to understand this phenomenon better.
Patient Factors
In tooth erosion, risk factors such as lifestyle, oral hygiene habits, and health condition are patient modifiable.
The manner in which dietary acids are introduced into the mouth (sipping, sucking, with/without drinking straw), which determines the duration and the localization of the acid attack, influences the appearance of the erosions. The frequency and duration of acid attacks are also closely associated with erosion and, therefore, very important for the adoption of prophylactic measures. Contact of the teeth with acids during the night can also lead to erosion because of the reduced production of saliva. Thus, for example, apart from cariogenesis there can be massive erosive tooth structure destruction as a result of the consumption of acidic sweet drinks, which some infants drink from their bottles continuously during the night.
Another risk factor on the patient side is stomach acid, which enters the mouth as a consequence of vomiting or reflux. Vomiting is the forceful expulsion of the contents of one’s stomach through the mouth and sometimes the nose. This phenomenon normally results from psychological disorders such as anorexia and bulimia nervosa. Reflux is defined as the involuntary movement of the gastric contents from the stomach into the mouth, caused by some abnormality in the gastrointestinal tract. In general, acidic gastric content entering the mouth may, in time, erode the teeth. Unlike dietary acids, the pH and titratability of gastric juice is significantly greater and so the level of destruction is normally more severe. Because the clinical manifestation of dental erosion does not occur until gastric acid has acted on the dental hard tissues regularly over some time, dental erosion caused by gastric acid has been observed only in those diseases that are associated with chronic vomiting or persistent gastroesophageal reflux, also known as gastroesphageal reflux disease (GERD), over a long period. Intrinsic tooth erosion usually takes place in the region of the occlusal and palatal tooth surfaces of the maxillary teeth. Often the dentist is the first person to detect these diseases and should treat them accordingly.
Saliva is of the essence in the tooth erosion process. Several salivary protective mechanisms come into play during an erosive challenge: dilution and clearance of an erosive agent from the mouth, neutralization and buffering of acids, slowing down the rate of enamel dissolution through the common ion effect by salivary Ca and P, and involvement in the formation of the pellicle. The acquired pellicle is an organic film free of bacteria that covers oral hard and soft tissues. It is composed of mucins, glycoproteins and proteins, including several enzymes. The acquired pellicle may protect against erosion by acting as a diffusion barrier or a selectively permeable membrane preventing direct contact between the acids and the tooth surface, thus reducing the dissolution rate of dental hard tissues.
Practical experience demonstrates the importance of saliva in patients suffering from salivary flow impairment. Studies have shown that erosion may be associated with low salivary flow or low buffering capacity. The dry mouth condition is usually related to aging, even though some other studies have not identified this correlation. It is well established that patients taking medication can also present decreased salivary output, as well as those who have received radiation therapy for head and neck cancer. Tests of the stimulated and unstimulated flow rate, as well as the buffering capacity of saliva may provide some information about the susceptibility of an individual to dental erosion. However, these parameters are only 2 aspects of a multifactorial condition. Sialometric evaluations should be performed at a fixed time point or in a limited time interval in the morning, to avoid intra-individual variation as a result of the circadian cycle. Studies have shown that sour foodstuffs have strong influences on the anticipatory salivary flow, which can be significantly increased compared with the normal unstimulated flow rate. Hypersalivation also occurs in advance of vomiting as a response from the vomiting center of the brain, as frequently seen in individuals suffering from anorexia and bulimia nervosa, rumination, or chronic alcoholism. It is suggested that this could minimize the erosion caused by acids of gastric origin. On the other hand, patients with symptoms of GERD should not expect salivary output to increase before gastric juice reflux, because this is an involuntary response that is not coordinated by the autonomic nervous system. Therefore, there may be insufficient time for saliva to act before erosion occurs.
Millward and colleagues monitored the pH at the surface of teeth in healthy volunteers after drinking 1% citric acid. They observed that the pH recovered to more than pH 5.5 within 2 minutes at a site adjacent to the palatal surface of the upper central incisor and within 4 to 5 minutes at another palatal surface on the upper first molar. Thus, the clearance rate of erosive agents may be influenced by the anatomy of the teeth and soft tissues, by the movement of the tongue and buccal mucosa, as well as by the swallowing pattern. In addition, the mechanical abrasion caused by the tongue was considered to be a contributing factor in erosion.
Apart from the risk factors discussed earlier, occupation and sport may also lead to erosive wear. Employees in the chemical industry or professional wine tasters have a higher risk of suffering erosion as a result of the increased acid-tooth contact. Tooth erosion associated with professional athletes or excessive exercise has also been reported. Excessive exposure to water or sports drinks with low pH, or increased gastroesophageal reflux resulting from strenuous exercise may be responsible for the sport-induced erosion. In the occurrence and development of erosion, occupation and sport can only be considered as cofactors rather than isolated factors, because erosion is a multifactorial condition.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


