If the eyes are “windows to the soul,” in an analogous manner the maxillary sinus is a window into the maxilla. The maxillary sinus graft has been the subject of more animal and clinical research trials than any other single bone-grafting site in the maxillofacial region. For their part, the maxillary sinuses assist the other sinuses in decreasing the overall weight of the human skull. Normal and abnormal maxillary sinus anatomy may present challenges to practicing oral and maxillofacial surgeons who intend to place endosseous root-form implants. Root-form implants have revolutionized the potential for not only esthetic restoration but also functional rehabilitation of edentulous maxillary ridges.
Major challenges can face surgeons who intend to place implants if there is inadequate bone in the maxillary antrum to stabilize and integrate the implants. Compartmentalized or septum-divided topography within the sinus may also present challenges in treatment planning and final implementation of designed treatment plans. The advent of computed tomography (CT) specifically designed to assist in avoiding error in estimation of bone height has changed the paradigms of treatment. The surface area available for grafting and even the volume of particulate or block graft required can be scientifically determined before surgery. This presents a major boon for grafting and implant-placing surgeons. In this chapter we will examine the cause of over-pneumatized sinuses and the treatment goals and techniques to deal with this phenomenon.
Etiopathogenic/Causative Factors
The maxillary alveolus undergoes progressive, non-reversible bone loss after the removal of a tooth from the alveolar process. Over time this loss results in expansion of the maxillary sinus cavity known as over-pneumatization. This presents a daunting challenge to implant surgeons. There is usually a reduction in the amount of bone available to stabilize a maxillary implant once placed in the maxilla. In Cawood and Howell’s treatise on the patterns of maxillary and mandibular resorption in 1988, they devised a classification for edentulous and over-pneumatized maxillas and maxillary sinuses ( Fig. 21-1 ):
- •
Class 1: Dentate
- •
Class 2: Immediately after extraction; the alveolus has healed
- •
Class 3: Well-rounded ridge; width and height are acceptable
- •
Class 4: Knife edge width; typically acceptable height
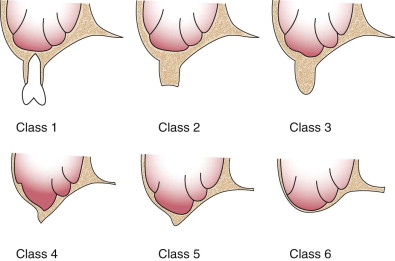
Unacceptable width:
- •
Class 5: Flat ridge; deficient width and height
- •
Class 6: Depressed ridge with loss of basilar bone and no distinctive pattern
There is increased morbidity in implant therapy if the fixture moves after placement, so one of the linchpin goals for successful implant therapy is primary stability. This tenet is of prime importance in the quest for good osseointegration of the implant fixture. Implants can be placed into over-pneumatized or atrophic maxillas (or both); however, augmentation with either particulate or corticocancellous grafts is usually required. Maxillary sinus cavities that have continued to expand after tooth loss are prevalent in a large section of the populace. The implant surgeon’s approach to restoring the area should be discussed with the patient, and all options for treatment (even those nonsurgical) should be broached during the treatment-planning consultation.
An element of paramount importance is maintenance of the integrity of the sinus membrane and its continued function. The lining of the maxillary sinus, known as the schneiderian membrane, is attached to the bordering bone of the maxillary sinus and is characterized by a periosteum overlaid with a thin layer of pseudo-ciliated stratified respiratory epithelium.
The normal thickness of the membrane is 0.3 to 0.8 mm in its natural state. Chronic sinus disease and additional sinus pathology may induce thickening of the mucosa but does not increase its tensile strength. This means that in the presence of disease or with a pristine sinus cavity, the sinus membrane is in danger of perforation unless great care is taken when dissecting and preparing the cavity before grafting. In studies of the histologic changes in the mucosal lining after implant placement, there was no change in the number of glands and goblet cells inside the mucosa.
The aforementioned study was performed without the addition of grafting materials, but extrapolation of the data suggests similar results in situations with grafting materials. A sinus grafted with particulate material may be at increased risk for infection and/or rhinosinusitis, but the membrane amazingly adapts to either challenge. Additional studies have also found that exposure of the implant in the sinus does not always lead to the development of sinus complications. The schneiderian membrane has proved to be an adaptable and amenable ally in restoration of an edentulous posterior maxilla in patients with over-pneumatization and attrition of the residual maxillary alveolus. Implant surgeons can use this adaptability to their advantage, even in patients with membrane tears. In a retrospective study of membrane perforations by Arkedian and colleagues, class II and class III perforations did not statistically change the outcome of implant placement into the grafted sinus. Implants osseointegrated successfully in 94% of patients on average. These numbers suggest adaptability even in the event of perforation when it is properly repaired.
Pathologic Anatomy
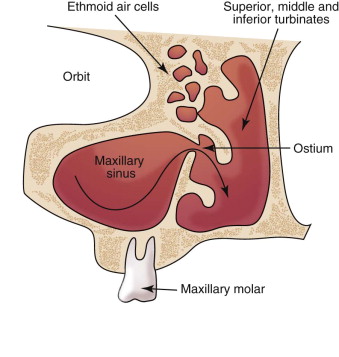
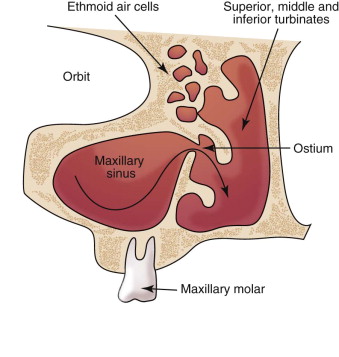
A properly functioning sinus uses the motility of the ciliated mucosa to move mucus and filter the air that moves across them. The maxillary ostium and mucosal lining contribute to normal function of the maxillary sinus. Maintenance of this anatomic relationship is dependent on careful manipulation of the membrane when it is elevated from the antrum floor. Direct elevation of the sinus in the medial and superior aspect of the sinus must be accomplished carefully to not disturb the ostium and cause blockage or inflammation. As noted in Figure 21-2 , the position of the ostium dictates the limit of dissection in the medial and superior planes of the sinus cavity.
An additional component that must be taken into consideration is the blood supply to the sinus and potential hemorrhage during the surgical procedure. Three arteries supply the maxillary sinus: the infraorbital, posterior superior alveolar, and lateral nasal arteries (posterior). The aforementioned vessels are all a division or branch of the internal maxillary artery. Most bleeding events during sinus surgery can be controlled by direct pressure and subsequent tamponade—however, the anatomy of the region may make it difficult to obtain direct pressure.
The changes in anthropometric measurements of the maxillary sinus are predictable and have been catalogued as mentioned earlier by Cawood and Howell. The pattern of loss of alveolar bone is normal after tooth loss; however, loss of basal bone is described as pathologic.
Common pathology that greatly influences outcomes in the sinus is the presence of sinus polyps, mucoceles, and persistent or refractory sinusitis. Sinus polyps and mucoceles are usually differentiated by their contents. Mucoceles (sometimes known as extravasation phenomena) are typically filled with fluid or mucin, are generally found along the floor of the sinus cavity, and have a classic smooth, dome-shaped morphology. Polyps are usually more dense in nature and consist of solid cells ; they are typically found along the roof and upper portions of the sinus cavity wall. Polyps may also erode bone, which is not a feature of mucoceles.
Refractory sinusitis may have an anatomic origin or be caused by exacerbations of infection and inflammation. Anatomic considerations involve impairment of the sinus lining or, potentially, blockage of the ostium. The different flora that inhabit the sinus may cause prolonged and difficult management challenges for the treating practitioner. Haemophilus influenzae , Streptococcus pneumoniae , and Moraxella catarrhalis are a few of the principal flora that must be addressed in acute and chronic exacerbations of sinusitis. Management of this disease process is discussed further in the section on postoperative care and follow-up in this chapter.
Pathologic Anatomy
A properly functioning sinus uses the motility of the ciliated mucosa to move mucus and filter the air that moves across them. The maxillary ostium and mucosal lining contribute to normal function of the maxillary sinus. Maintenance of this anatomic relationship is dependent on careful manipulation of the membrane when it is elevated from the antrum floor. Direct elevation of the sinus in the medial and superior aspect of the sinus must be accomplished carefully to not disturb the ostium and cause blockage or inflammation. As noted in Figure 21-2 , the position of the ostium dictates the limit of dissection in the medial and superior planes of the sinus cavity.
An additional component that must be taken into consideration is the blood supply to the sinus and potential hemorrhage during the surgical procedure. Three arteries supply the maxillary sinus: the infraorbital, posterior superior alveolar, and lateral nasal arteries (posterior). The aforementioned vessels are all a division or branch of the internal maxillary artery. Most bleeding events during sinus surgery can be controlled by direct pressure and subsequent tamponade—however, the anatomy of the region may make it difficult to obtain direct pressure.
The changes in anthropometric measurements of the maxillary sinus are predictable and have been catalogued as mentioned earlier by Cawood and Howell. The pattern of loss of alveolar bone is normal after tooth loss; however, loss of basal bone is described as pathologic.
Common pathology that greatly influences outcomes in the sinus is the presence of sinus polyps, mucoceles, and persistent or refractory sinusitis. Sinus polyps and mucoceles are usually differentiated by their contents. Mucoceles (sometimes known as extravasation phenomena) are typically filled with fluid or mucin, are generally found along the floor of the sinus cavity, and have a classic smooth, dome-shaped morphology. Polyps are usually more dense in nature and consist of solid cells ; they are typically found along the roof and upper portions of the sinus cavity wall. Polyps may also erode bone, which is not a feature of mucoceles.
Refractory sinusitis may have an anatomic origin or be caused by exacerbations of infection and inflammation. Anatomic considerations involve impairment of the sinus lining or, potentially, blockage of the ostium. The different flora that inhabit the sinus may cause prolonged and difficult management challenges for the treating practitioner. Haemophilus influenzae , Streptococcus pneumoniae , and Moraxella catarrhalis are a few of the principal flora that must be addressed in acute and chronic exacerbations of sinusitis. Management of this disease process is discussed further in the section on postoperative care and follow-up in this chapter.
Diagnostic Studies
In the modern age of oral and maxillofacial surgery, the integration of technology into all facets of surgery is an exciting event. Diagnostic modalities have leaped beyond alginate impressions and refractory casts, although the lessons learned with these methods still serve and are part of sound surgical principle. Modern computer simulations and three-dimensional graphics can allow surgeons to visualize all aspects of a surgical area and not be limited by line of sight or unfavorable anatomy. These are exciting times as we forge ahead with more accurate diagnosis to shorten patients’ surgical and recovery time.
Proper diagnostic work-up of a patient before grafting is essential for postoperative success and retention of the graft. As with any other surgery or medical treatment, the history and physical examination are the most important tools to gather information regarding any past procedures or trauma to the area in question. Plain films (Panorex and sometimes periapical radiographs) give the grafting surgeon initial insight into the grafting site and indicate potential barriers or hurdles to success. The presence of septa, anatomic limitations, and asymptomatic pathology in and around the sinus cavity may be noted. In some cases, mounted diagnostic casts give weight to the big picture of what the restorative dentist may have to encounter after grafting and implant placement. They can be used to determine whether there is enough interocclusal space and whether orthodontics or additional crowns and bridges may be needed to “open the bite” and provide restored implants.
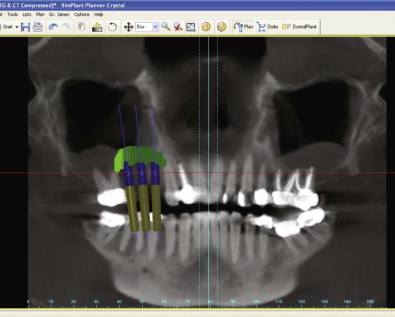
The advent of CT and digitized radiographs in 1972 has greatly assisted surgeons in proper treatment planning of their surgical case. CT can show up to 200 or more different levels or shades of gray to offer increased information and detail of anatomic structures. In contrast, a panoramic radiograph is limited to about 30 shades of gray in its detail. Refinement of these digitized images by treatment planning software allows the images to be fleshed out into three dimensions and simulated implants to be placed to show their viability in the particular case. Although there are good arguments to support the wider use of CT, there is also the “old-school” line of thought that with mounted models and diagnostic wax-ups, peri-apical and panoramic radiographs provide good intraoral examination. That money can be saved in the treatment planning of a procedure, if not the time. The density of bone in an area proposed for implant placement may also be determined with CT. The scan will measure the Hounsfield units to determine the density and therefore the ease or difficulty of preparation of the osteotomy site. According to Kraut, approximately 14% of patients seeking mandibular implants and 72% of patients seeking maxillary implants benefit from the use of CT in their treatment planning. Although it would be inappropriate and not cost-effective to use CT for all implant planning, it is fast becoming a more commonplace tool in the diagnostic armamentarium ( Fig. 21-3 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


